Practice Essentials
Prior to the introduction of extracorporeal shockwave lithotripsy (ESWL) in 1980, the only treatment available for calculi that could not pass through the urinary tract was open surgery. Since then, ESWL has become the preferred tool in the urologist’s armamentarium for the treatment of renal stones, proximal stones, and midureteral stones. Compared with open and endoscopic procedures, ESWL is minimally invasive, exposes patients to less anesthesia, and yields equivalent stone-free rates in appropriately selected patients.
The efficacy of ESWL lies in its ability to pulverize calculi in vivo into smaller fragments, which the body can then expulse spontaneously. Shockwaves are generated and then focused onto a point within the body. The shockwaves propagate through the body with negligible dissipation of energy (and therefore damage) owing to the minimal difference in density of the soft tissues. At the stone-fluid interface, the relatively large difference in density, coupled with the concentration of multiple shockwaves in a small area, produces a large dissipation of energy. Via various mechanisms, this energy is then able to overcome the tensile strength of the calculi, leading to fragmentation. Repetition of this process eventually leads to pulverization of the calculi into small fragments (ideally < 1 mm) that the body can pass spontaneously and painlessly.
Technical aspects
All lithotripsy machines share 4 basic components: (1) a shockwave generator, (2) a focusing system, (3) a coupling mechanism, and (4) an imaging/localization unit.
Shockwave generator
Shockwaves can be generated in 1 of 3 ways, as follows:
-
Electrohydraulic: The original method of shockwave generation (used in the Dornier HM3) was electrohydraulic, meaning that the shockwave is produced via spark-gap technology. In an electrohydraulic generator, a high-voltage electrical current passes across a spark-gap electrode located within a water-filled container. The discharge of energy produces a vaporization bubble, which expands and immediately collapses, thus generating a high-energy pressure wave.
-
Piezoelectric: The piezoelectric effect produces electricity via application of mechanical stress. The Curie brothers first demonstrated this in 1880. The following year, Gabriel Lippman theorized the reversibility of this effect, which was later confirmed by the Curie brothers. The piezoelectric generator takes advantage of this effect. Piezoelectric ceramics or crystals, set in a water-filled container, are stimulated via high-frequency electrical pulses. The alternating stress/strain changes in the material create ultrasonic vibrations, resulting in the production of a shockwave.
-
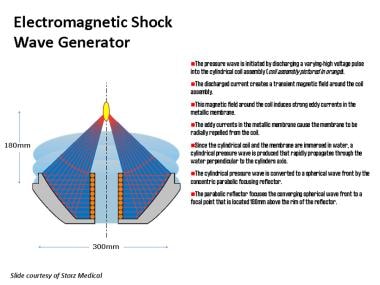
Electromagnetic: In an electromagnetic generator (as seen below), a high voltage is applied to an electromagnetic coil, similar to the effect in a stereo loudspeaker. This coil, either directly or via a secondary coil, induces high-frequency vibration in an adjacent metallic membrane. This vibration is then transferred to a wave-propagating medium (ie, water) to produce shockwaves.
Focusing systems
The focusing system is used to direct the generator-produced shockwaves at a focal volume in a synchronous fashion. The basic geometric principle used in most lithotriptors is that of an ellipse. Shockwaves are created at one focal point (F1) and converge at the second focal point (F2). The target zone, or blast path, is the 3-dimensional area at F2, where the shockwaves are concentrated and fragmentation occurs.
Focusing systems differ, depending on the shockwave generator used. Electrohydraulic systems used the principle of the ellipse; a metal ellipsoid directs the energy created from the spark-gap electrode. In piezoelectric systems, ceramic crystals arranged within a hemispherical dish direct the produced energy toward a focal point. In electromagnetic systems, the shockwaves are focused with either an acoustic lens (Siemens system) or a cylindrical reflector (Storz system).
Coupling mechanisms
In the propagation and transmission of a wave, energy is lost at interfaces with differing densities. As such, a coupling system is needed to minimize the dissipation of energy of a shockwave as it traverses the skin surface. The usual medium used is water, as this has a density similar to that of soft tissue and is readily available. In first-generation lithotriptors (Dornier HM3), the patient was placed in a water bath. However, with second- and third-generation lithotriptors, small water-filled drums or cushions with a silicone membrane are used instead of large water baths to provide air-free contact with the patient's skin. This innovation facilitates the treatment of calculi in the kidney or the ureter, often with less anesthesia than that required with the first-generation devices.
Localization systems
Imaging systems are used to localize the stone and to direct the shockwaves onto the calculus, as well as to track the progress of treatment and to make alterations as the stone fragments. The 2 methods commonly used to localize stones include fluoroscopy and ultrasonography.
Fluoroscopy, which is familiar to most urologists, involves ionizing radiation to visualize calculi. As such, fluoroscopy is excellent for detecting and tracking calcified and otherwise radio-opaque stones, both in the kidney and the ureter. Conversely, it is usually poor for localizing radiolucent stones (eg, uric acid stones). To compensate for this shortcoming, intravenous contrast can be introduced or (more commonly) cannulation of the ureter with a catheter and retrograde instillation of contrast (ie retrograde pyelography) can be performed.
Ultrasonographic localization allows for visualization of both radiopaque and radiolucent renal stones and the real-time monitoring of lithotripsy. Most second-generation lithotriptors can use this imaging modality, which is much less expensive to use than radiographic systems. Although ultrasonography has the advantage of preventing exposure to ionizing radiation, it is technically limited by its ability to visualize ureteral calculi, typically due to interposed air-filled intestinal loops. In particular, smaller stones may be difficult to localize accurately.
History of the Procedure
Evolution of shockwave lithotriptors
The Dornier HM3, originally designed to test supersonic aircraft parts, was the first shockwave lithotriptor introduced in the United States. Despite being somewhat dated, it is still one of the most effective lithotriptors and has become the standard to which other devices are compared. The design of the HM3 is based on an electrohydraulic shockwave generator; the shockwaves are focused via an ellipsoid metal water-filled tub in which both the patient and the generator are submerged. Biplanar fluoroscopy is used for localization, allowing placement of the calculi to be fragmented in the target zone.
Second-generation lithotriptors typically use piezoelectric or electromagnetic generators as the energy source. When coupled with the appropriate focusing device, these shockwave generators commonly have a smaller focal zone. Although a smaller focal zone may minimize damage to the surrounding tissue, this comes at a price. During respiratory excursion, the stone may move in and out of the focal zone; this may compromise fragmentation rates. The coupling device in a second-generation lithotriptor is a silicone-encased water cushion that coapts to the patient, a design that greatly simplifies the positioning of patients.
The newest-generation lithotriptors have been designed to offer greater portability and adaptability. These systems often provide imaging with both fluoroscopy and ultrasonography. The ability to alternate between imaging modalities allows the urologist to compensate for the deficiencies of either system.
Most current lithotriptors are powered by an electromagnetic generator. Electromagnetic generators and their focusing units are capable of delivering shockwaves that are similar in intensity to those of the HM3, but usually to a smaller focal zone. As mentioned above, this has the theoretical advantage of minimizing damage to surrounding soft tissue. However, because of the smaller focal zone, respiration may cause the stone to move out of the target zone for portions of the treatment. Although improved localization techniques and anesthetic manipulation can be used to account for this, the shockwaves applied while the stones are out of the target zone do not cause fragmentation. Thus, certain second- and third-generation machines are associated with higher failure rates, incomplete treatment, and the need for retreatment.
Pathophysiology
A stone is fragmented when the force of the shockwaves overcomes the tensile strength of the stone. Although incompletely understood, fragmentation is thought to occur through a combination of methods, including compressive and tensile forces, erosion, shearing, spalling, and cavitation. Of these various forces, the generation of compressive and tensile forces and cavitation are thought to be the most important.
When a shockwave is propagated through a medium (water), it loses very little energy until it crosses into a medium with a different density. If the medium is denser, compressive forces are produced on the new medium. Similarly, if the new medium is less dense, tensile stress is produced on the first medium. Upon hitting the anterior surface of a stone, the change in density creates compressive forces, causing fragmentation. As the wave proceeds through the stone to the posterior surface, the change from high to low density reflects part of the shockwave’s energy, producing tensile forces, which again disrupt and fragment the stone.
In cavitation, shockwave energy applied at a focal point leads to failure of the liquid with generation of water-vapor bubbles. These gaseous bubbles collapse explosively, creating microjets that fracture and erode the calculus. This process can be monitored with real-time ultrasonography during the treatment and appears as swirling fragments and liquid in the focal zone.
Indications
The current options available for the treatment of renal and ureteral calculi include conservative management (watchful waiting for spontaneous passage), extracorporeal shockwave lithotripsy (ESWL), endoscopic techniques (rigid or flexible ureteroscopic lithotripsy), and percutaneous treatments.
The American Urological Association Stone Guidelines Panel has classified ESWL as a potential first-line treatment for ureteral and renal stones smaller than 2 cm.
In the pediatric population, those with uncomplicated, non-infectious calculi can undergo ESWL with an age-dependent response. [1]
Indications for ESWL include the following:
-
Individuals who work in professions in which unexpected symptoms of stone passage may prompt dangerous situations (eg, pilots, military personnel, physicians) (In such individuals, definitive management is preferred to prevent adverse outcomes.)
-
Individuals with solitary kidneys in whom attempted conservative management and spontaneous passage of the stone may lead to an anuric state
-
Patients with hypertension, diabetes, or other medical conditions that predispose to renal insufficiency
Whereas current American Urological Association guidelines recommend ureteroscopy (URS) as the primary management of distal ureteral stones and ESWL as a secondary option, several studies demonstrated SWL to be an effective option in the management of distal ureteral calculi. Scotland et al reported a stone-free rate (SFR) of 78.8% after one SWL procedure and a SFR of 87.5% after two SWLs for distal ureteral stones. Of note, 3.8% of patients required a salvage URS following a failed second SWL to achieve stone-free status. [2] In a multicenter randomized controlled trial comparing SWL and ureteroscopic treatment as therapeutic options for ureteral stones, 22.1% of patients in the SWL arm needed further treatment versus 10.3% in the URS arm. The absolute risk difference was 11.7% in favor of URS, which was inside the 20% threshold the authors set for demonstrating noninferiority of SWL. [3]
Relevant Anatomy
See Preoperative details.
Contraindications
Absolute contraindications to extracorporeal shockwave lithotripsy (ESWL) include the following:
-
Acute urinary tract infection or urosepsis
-
Uncorrected bleeding disorders or coagulopathies
-
Pregnancy
-
Uncorrected obstruction distal to the stone
Relative contraindications include the following:
-
Body habitus: Morbid obesity and orthopedic or spinal deformities may complicate or prevent proper positioning. In these situations, attempting to position the patient prior to anesthetic induction is useful to ensure the practicality of the approach.
-
Renal ectopy or malformations (eg, horseshoe kidneys and pelvic kidneys)
-
Complex intrarenal drainage (eg, infundibular stenosis)
-
Poorly controlled hypertension (due to increased bleeding risk)
-
Gastrointestinal disorders: In rare cases, these may be exacerbated after ESWL treatment.
-
Renal insufficiency: Stone-free rates in patients with renal insufficiency (57%) (serum creatinine level of 2–2.9 mg/dL) were significantly lower than in patients with better renal function (66%) (serum creatinine level < 2 mg/dL).
-
History of previous Open Renal Stone Surgery: Overall stone-free rates after ESWL treatment found to be significantly lower in patients with a history of open stone surgery, especially for those with stones in the lower calyx (48.4% vs. 64%) [4]
Preexisting pulmonary and cardiac problems are not contraindications, provided they are appropriately addressed both preoperatively and intraoperatively. In patients with a history of cardiac arrhythmias, the shockwave can be linked to electrocardiography (ECG), thus firing only on the R wave in the cardiac cycle, coinciding with the refractory period of the cardiac cycle (ie, gated lithotripsy).
Ganem and Carson retrospectively reviewed patients treated with gated and ungated lithotripsy. The study population included those with preexisting hypertension and cardiac disease and those taking cardiac medications. Of the patients in the ungated group, 20% developed arrhythmias, although they were universally benign, resolving with conversion to a gated procedure. Conversely, only 1 of 357 patients in the gated lithotripsy group developed any arrhythmia. [5]
Eaton and Erturk studied 51 patients who underwent ungated lithotripsy, including several patients with preexisting cardiac arrhythmias. The 21 patients who had more than 6 premature ventricular contractions (PVC) intraoperatively had troponin measured 24 hours postoperatively. A selected sample of patients who did not develop arrhythmias also had troponin measured as a control group and the troponin levels did not vary significantly between the 2 groups. [6]
Investigators concluded that ESWL-induced ventricular ectopy was probably reflective of mechanical stimulation of the myocardium rather than myocardial injury. However, the authors caution that as rare reports exist of myocardial injury after ESWL, one should exercise caution when treating patients with renal stones who may be at increased risk for cardiac damage.
Based on these studies, patients with preexisting cardiac disease, not including documented preoperative arrhythmia, can probably undergo ungated lithotripsy safely. Close monitoring is imperative as those who develop arrhythmias can be safely converted to gated lithotripsy.
Cardiac pacemakers are also not contraindicated, although seeking assistance from a cardiologist for possible changes to pacemaker settings would be prudent.
Oral anticoagulants (eg, clopidogrel [Plavix] and warfarin [Coumadin]) should be discontinued to allow normalization of clotting parameters. Platelet function is normalized by discontinuing aspirin-containing products and nonsteroidal anti-inflammatory drugs (NSAIDs) 7 days before treatment.
-
Electromagnetic generator system.