Practice Essentials
Erectile dysfunction (ED), formerly termed impotence, is defined as "the inability to attain and/or maintain penile erection sufficient for satisfactory sexual performance" or "the consistent or recurrent inability to attain and/or maintain penile erection sufficient for sexual satisfaction". [1] Although some cases, particularly in younger men, may primarily reflect psychological concerns, in many cases ED results from organic disease—notably, cardiovascular disease, diabetes mellitus, hyperlipidemia, and hypertension. [2] Thus, ED may serve as a marker for medical conditions in need of treatment. [1] Regardless of the cause, however, ED can have negative effects on patients' self-esteem, relationships, and overall quality of life. [1, 2]
Signs and symptoms
The first step in the management of ED is a thorough history that includes the following:
-
Sexual history
-
Medical history
-
Psychosocial history
A physical examination is necessary for every patient, emphasizing the genitourinary, vascular, and neurologic systems. A focused examination entails evaluation of the following:
-
Blood pressure
-
Peripheral pulses
-
Sensation
-
Status of the genitalia and prostate
-
Size and texture of the testes
-
Presence of the epididymis and vas deferens
-
Abnormalities of the penis (eg, hypospadias, Peyronie plaques)
There is a strong correlation between hypertension and ED. There is also a correlation between benign prostatic hyperplasia and ED, though the causality is unclear.
See Presentation for more detail.
Diagnosis
Laboratory testing for ED depends on information gathered during the interview; it is necessary for most patients, although not for all. Such testing may include the following:
-
Evaluation of hormonal status (testosterone, serum hormone–binding globulin, luteinizing hormone [LH], prolactin, thyroid-stimulating hormone [TSH]) – Note that the American College of Physicians (ACP) does not recommend for or against routine use of hormonal blood tests or hormonal treatment in ED patients
-
Screening blood studies (hemoglobin A1c, serum chemistry panel, lipid profile)
-
Prostate-specific antigen levels, if the patient is a candidate for prostate cancer screening (controversial)
-
Urinalysis
Functional tests that may be helpful include the following:
-
Biothesiometry – Infrequently indicated
-
Nocturnal penile tumescence testing – Once frequently performed, this is rarely used in current practice, though it can be helpful when the diagnosis is in doubt
-
Formal neurologic testing – Not needed in the vast majority of ED patients, though it may offer some benefit to patients with a history of central nervous system problems, peripheral neuropathy, diabetes, or penile sensory deficit
Imaging studies are not commonly warranted, except in situations where pelvic trauma has been sustained or surgery performed. Modalities that may be considered include the following:
-
Ultrasonography of the penis (to assess vascular function within the penis)
-
Ultrasonography of the testes (to help disclose abnormalities in the testes and epididymides; rarely indicated)
-
Transrectal ultrasonography (to disclose abnormalities in the prostate and pelvis that may interfere with erectile function)
-
Angiography (in patients who are potential candidates for vascular surgery)
See Workup for more detail.
Management
Treatment options for ED include the following:
-
Sexual counseling, if no organic causes can be found for the dysfunction
-
Oral medications
-
Injected, implanted, or topically applied medications
-
External vacuum and constriction devices
-
Surgery
Many patients with ED also have cardiovascular disease; thus, treatment of ED in these patients must take cardiovascular risks into account.
According to American Urological Association (AUA) guidelines, oral phosphodiesterase type 5 (PDE5) inhibitors are first-line therapy unless contraindicated. [1] Agents include the following:
-
Sildenafil
-
Vardenafil
-
Tadalafil
-
Avanafil
In patients with ED refractory to oral PDE5 inhibitors, one of these agents can be combined with an injection of PGE1. [3]
In a prospective, multicenter, single-armed study of ED patients who exhibited a suboptimal response to PDE5 inhibitors, the investigators found that percutaneous implantation of zotarolimus-eluting stents in focal atherosclerotic lesions was both safe and feasible and was associated with clinically meaningful improvement on subjective and objective measures of erectile function. [4]
Hormone replacement may benefit men with severe hypogonadism and may possibly be useful as adjunctive therapy when other treatments are unsuccessful. Replacement androgens are available in oral (rarely used), injectable, gel, and transdermal preparations.
Intracavernosal injection therapy may be considered and is almost always effective if the vasculature within the corpora cavernosa is healthy. Agents used include the following:
-
Alprostadil (most common)
-
Phentolamine
-
Papaverine
The Medicated Urethral System for Erections (MUSE) involves the formulation of alprostadil (PGE1) into a small intraurethral suppository that can be inserted into the urethra. This may be useful for men who do not want to use self-injections or those in whom oral medications have failed.
External devices that may be used include the following:
-
Vacuum devices to draw blood into the penis
-
Constriction devices placed at the base of the penis to maintain erection
Selected patients with ED are candidates for surgical treatment. Procedures to be considered include the following:
-
Revascularization (rarely indicated)
-
Surgical elimination of venous outflow (rarely indicated)
-
Placement of penile implant (semirigid or malleable rod implant, fully inflatable implant, or self-contained inflatable unitary implant) – Once the only effective therapy for men with organic ED, this is the last option considered in current practice
Suggested measures for preventing ED include the following:
-
Optimal management of diabetes, heart disease, and hypertension
-
Lifestyle modifications to improve vascular function (eg, not smoking, maintaining ideal body weight, and engaging in regular exercise)
See Treatment and Medication for more detail.
Background
Erectile dysfunction (ED) affects 50% of men older than 40 years, [5] exerting substantial effects on quality of life. [6] This common problem is complex and involves multiple pathways. Penile erections are produced by an integration of physiologic processes involving the central nervous, peripheral nervous, hormonal, and vascular systems. Any abnormality in these systems, whether from medication or disease, has a significant impact on the ability to develop and sustain an erection, ejaculate, and experience orgasm.
A common and important cause of ED is vasculogenic. Many men with ED have comorbid conditions such as hyperlipidemia, hypercholesterolemia, tobacco abuse, diabetes mellitus, or coronary artery disease (CAD). [7] The Princeton III Consensus recommends screening men who present with ED for cardiovascular risk factors; ED may be the earliest presentation of atherosclerosis and vascular disease. [8]
Additionally, the physiologic processes involving erections begin at the genetic level. Certain genes become activated at critical times to produce proteins vital to sustaining this pathway. Some researchers have focused on identifying particular genes that place men at risk for ED. At present, these studies are limited to animal models, and little success has been reported to date. [5] Nevertheless, this research has given rise to many new treatment targets and a better understanding of the entire process.
The first step in treating the patient with ED is to take a thorough sexual, medical, and psychosocial history. Questionnaires are available to assist clinicians in obtaining important patient data. (See Presentation.) Successful treatment of sexual dysfunction has been demonstrated to improve sexual intimacy and satisfaction, improve sexual aspects of quality of life, improve overall quality of life, and relieve symptoms of depression. (See Treatment.)
The availability of phosphodiesterase-5 (PDE5) inhibitors—sildenafil, vardenafil, tadalafil, and avanafil—has fundamentally altered the medical management of ED. In addition, direct-to-consumer marketing of these agents over the last 15 years has increased the general public’s awareness of ED as a medical condition with underlying causes and effective treatments.
Unfortunately, some patients may have an overly simplified understanding of the role of PDE5 inhibitors in ED management. Such patients may not expect or be willing to undergo a long evaluation and testing process to obtain a better understanding of their sexual problem, and they may be less likely to involve their partner in discussing their sexual relationship with the physician. They may expect to obtain medications through a phone call to their doctor or even over the Internet, with minimal or no physician contact at all.
In such cases, the physician’s role may have to include efforts to educate patients about realistic sexual expectations (see Patient Education). These efforts can help prevent the misuse or overuse of these remarkable medications.
Although this article focuses primarily on the male with ED, it is essential to remember that the sexual partner plays an integral role in treatment. If successful and effective management is to be achieved, evaluation and discussion of any intervention must include both partners.
Diagnostic criteria (DSM-5) for erectile disorder
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), classifies erectile disorder as belonging to a group of sexual dysfunction disorders typically characterized by a clinically significant inability to respond sexually or to experience sexual pleasure. [9]
Sexual functioning involves a complex interaction among biologic, sociocultural, and psychological factors, and the complexity of this interaction makes it difficult to ascertain the clinical etiology of sexual dysfunction. Before any diagnosis of sexual dysfunction is made, problems that are explained by a nonsexual mental disorder or other stressors must first be addressed. Thus, in addition to the criteria for erectile disorder, the following must be considered:
-
Partner factors (eg, partner sexual problems or health issues)
-
Relationship factors (eg, communication problems, differing levels of desire for sexual activity, or partner violence)
-
Individual vulnerability factors (eg, history of sexual or emotional abuse, existing psychiatric conditions such as depression, or stressors such as job loss)
-
Cultural or religious factors (eg, inhibitions or conflicted attitudes regarding sexuality)
-
Medical factors (eg, an existing medical condition or the effects of drugs or medications)
The specific DSM-5 criteria for erectile disorder are as follows [9] :
-
In almost all or all (75-100%) sexual activity, the experience of at least one of the following three symptoms: (1) marked difficulty in obtaining an erection during sexual activity, (2) marked difficulty in maintaining an erection until the completion of sexual activity, or (3) marked decrease in erectile rigidity
-
The symptoms above have persisted for approximately 6 months
-
The symptoms above cause significant distress to the individual
-
The dysfunction cannot be better explained by nonsexual mental disorder, a medical condition, the effects of a drug or medication, or severe relationship distress or other significant stressors
The severity of delayed ejaculation is classified as mild, moderate, or severe on the basis of the level of distress the patient exhibits over the symptoms. The duration of the dysfunction is specified as follows:
-
Lifelong (present since first sexual experience)
-
Acquired (developing after a period of relative normal sexual functioning)
In addition, the context in which the dysfunction occurs is specified as follows:
-
Generalized (not limited to certain types of stimulation, situations, or partners)
-
Situational (limited to specific types of stimulation, situations, or partners)
Lifelong erectile disorder is associated with psychological factors, whereas acquired erectile disorder is more often related to biologic factors. Distress associated with erectile disorder is lower among older men than among younger men.
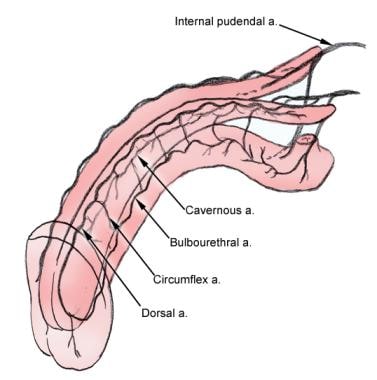
Anatomy
An understanding of penile anatomy is fundamental to management of ED. [3] The common penile artery, which derives from the internal pudendal artery, branches into the dorsal, bulbourethral, and cavernous arteries (see the image below).
The dorsal artery provides for engorgement of the glans during erection, whereas the bulbourethral artery supplies the bulb and the corpus spongiosum. The cavernous artery effects tumescence of the corpus cavernosum and thus is principally responsible for erection. The cavernous artery gives off many helicine arteries, which supply the trabecular erectile tissue and the sinusoids. These helicine arteries are contracted and tortuous in the flaccid state and become dilated and straight during erection. [10]
Venous drainage of the corpora originates in tiny venules that lead from the peripheral sinusoids immediately beneath the tunica albuginea. These venules travel in the trabeculae between the tunica and the peripheral sinusoids to form the subtunical venous plexus before exiting as the emissary veins (see the image below). [10]
 These images depict penile anatomy. Note the sinusoidal makeup of the corpora and thick fascia (ie, Buck fascia) that covers the corpora cavernosa. The major blood vessels to the corpora cavernosa enter through tributaries from the main vessels running along the dorsum of the penis.
These images depict penile anatomy. Note the sinusoidal makeup of the corpora and thick fascia (ie, Buck fascia) that covers the corpora cavernosa. The major blood vessels to the corpora cavernosa enter through tributaries from the main vessels running along the dorsum of the penis.
Sexual behavior involves the participation of autonomic and somatic nerves and the integration of numerous spinal and supraspinal sites in the central nervous system (CNS). The penile portion of the process that leads to erections represents only a single component.
The hypothalamic and limbic pathways play an important role in the integration and control of reproductive and sexual functions. The medial preoptic center, paraventricular nucleus, and anterior hypothalamic regions modulate erections and coordinate autonomic events associated with sexual responses.
Afferent information is assessed in the forebrain and relayed to the hypothalamus. The efferent pathways from the hypothalamus enter the medial forebrain bundle and project caudally near the lateral part of the substantia nigra into the midbrain tegmental region.
Several pathways have been described to explain how information travels from the hypothalamus to the sacral autonomic centers. One pathway travels from the dorsomedial hypothalamus through the dorsal and central gray matter, descends to the locus ceruleus, and projects ventrally in the mesencephalic reticular formation. Input from the brain is conveyed through the dorsal spinal columns to the thoracolumbar and sacral autonomic nuclei.
The primary nerve fibers to the penis are from the dorsal nerve of the penis, a branch of the pudendal nerve. The cavernosal nerves are a part of the autonomic nervous system and incorporate both sympathetic and parasympathetic fibers. They travel posterolaterally along the prostate and enter the corpora cavernosa and corpus spongiosum to regulate blood flow during erection and detumescence. The dorsal somatic nerves are also branches of the pudendal nerves. They are primarily responsible for penile sensation. [11]
Pathophysiology
Factors mediating contraction and relaxation
The degree of contraction of cavernosal smooth muscle determines the functional state of the penis. [12] The balance between contraction and relaxation is controlled by central and peripheral factors that involve many transmitters and transmitter systems.
The nerves and endothelium of sinusoids and vessels in the penis produce and release transmitters and modulators that control the contractile state of corporal smooth muscles. Although the membrane receptors play an important role, downstream signaling pathways are also important. The RhoA–Rho kinase pathway is involved in the regulation of cavernosal smooth muscle contraction. [13]
Factors that mediate contraction in the penis include noradrenaline, endothelin-1, neuropeptide Y, prostanoids, angiotensin II, and others not yet identified. Factors that mediate relaxation include acetylcholine, nitric oxide (NO), vasoactive intestinal polypeptide, pituitary adenylyl cyclase–activating peptide, calcitonin gene–related peptide, adrenomedullin, adenosine triphosphate, and adenosine prostanoids.
Nitric oxide pathway
The NO pathway is of critical importance in the physiologic induction of erections. The drugs currently used to treat ED were developed as a result of experimental and clinical work showing that NO released from nerve endings relaxes the vascular and corporal smooth muscle cells of the penile arteries and trabeculae, resulting in an erection.
NO is produced by the enzyme NO synthase (NOS). [14] NOS plays many roles, ranging from homeostasis to immune system regulation. To date, 3 subtypes have been identified: nNOS, iNOS, and eNOS, which are produced by the genes NOS1, NOS2, and NOS3, respectively. This nomenclature is derived from the sources of the original isolates: neuronal tissue (nNOS), immunoactivated macrophage cell lines (iNOS), and vascular endothelium (eNOS). The subtypes are not, however, limited to the tissues from which they were first isolated.
All NOS subtypes produce NO, but each may play a different biologic role in various tissues. nNOS and eNOS are considered constitutive forms because they share biochemical features: They are calcium-dependent, they require calmodulin and reduced nicotinamide adenine dinucleotide phosphate for catalytic activity, and they are competitively inhibited by arginine derivatives. nNOS is involved in the regulation of neurotransmission, and eNOS is involved in the regulation of blood flow.
iNOS is considered an inducible form because it is calcium-independent. iNOS is induced by the inflammatory process, in which it participates in the production of nitrogenous amines. This subtype has been shown to be involved in carcinogenesis, leading to transitional cell carcinoma.
Inside the cell, NOS catalyzes the oxidation of L-arginine to NO and L-citrulline. Endogenous blockers of this pathway have been identified. The gaseous NO that is produced acts as a neurotransmitter or paracrine messenger. Its biologic half-life is only 5 seconds. NO may act within the cell or diffuse and interact with nearby target cells. In the corpora cavernosa, NO activates guanylate cyclase, which in turn increases cyclic guanosine monophosphate (cGMP). Relaxation of vascular smooth muscles by cGMP leads to vasodilation and increased blood flow.
Alteration of NO levels is the focus of several approaches to the treatment of ED. Inhibitors of phosphodiesterase, which primarily hydrolyze cGMP type 5, provided the basis for the development of the PDE5 inhibitors. Chen et al administered oral L-arginine and reported subjective improvement in 50 men with ED. [15] These supplements are readily available commercially. Reported adverse effects include nausea, diarrhea, headache, flushing, numbness, and hypotension.
Increasing evidence indicates that NO acts centrally to modulate sexual behavior and to exert its effects on the penis. NO is thought to act in the medial preoptic area and the paraventricular nucleus. Injection of NOS inhibitors prevents the erectile response in rats that have been given erectogenic agents.
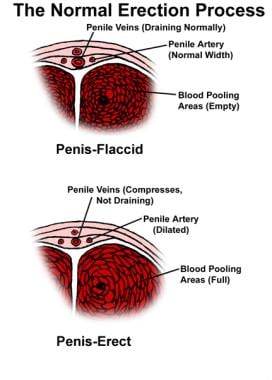
Normal erectile process
Erections occur in response to tactile, olfactory, and visual stimuli. The ability to achieve and maintain a full erection depends not only on the penile portion of the process but also on the status of the peripheral nerves, the integrity of the vascular supply, and biochemical events within the corpora. The autonomic nervous system is involved in erection, orgasm, and tumescence. The parasympathetic nervous system is primarily involved in sustaining and maintaining an erection, which is derived from S2-S4 nerve roots.
Sexual stimulation causes the release of neurotransmitters from cavernosal nerve endings and relaxation factors from endothelial cells lining the sinusoids. NOS produces NO from L-arginine, and this, in turn, produces other muscle-relaxing chemicals, such as cGMP and cyclic adenosine monophosphate (cAMP), which work via calcium channel and protein kinase mechanisms (see the image below). This results in the relaxation of smooth muscle in the arteries and arterioles that supply the erectile tissue, producing a dramatic increase in penile blood flow.
Relaxation of the sinusoidal smooth muscle increases its compliance, facilitating rapid filling and expansion. The venules beneath the rigid tunica albuginea are compressed, resulting in near-total occlusion of venous outflow. These events produce an erection with an intracavernosal pressure of 100 mm Hg.
Additional sexual stimulation initiates the bulbocavernous reflex. The ischiocavernous muscles forcefully compress the base of the blood-filled corpora cavernosa, and the penis reaches full erection and hardness when intracavernosal pressure reaches 200 mm Hg or more. At this pressure, both inflow and outflow of blood temporarily cease.
Detumescence results from cessation of neurotransmitter release, breakdown of second messengers by phosphodiesterase, and sympathetic nerve excitation during ejaculation. Contraction of the trabecular smooth muscle reopens the venous channels, allowing the blood to be expelled and thereby resulting in flaccidity.
Role of testosterone
Both ED and low testosterone (hypogonadism) increase with age. The incidence of the latter is 40% in men aged 45 years and older. [16] Testosterone is known to be important in mood, cognition, vitality, bone health, and muscle and fat composition. It also plays a key role in sexual dysfunction (eg, low libido, poor erection quality, ejaculatory or orgasmic dysfunction, reduced spontaneous erections, or reduced sexual activity). [17]
The association between low testosterone and ED is not entirely clear. Although these 2 processes certainly overlap in some instances, they are distinct entities. Some 2-21% of men have both hypogonadism and ED; however, it is unclear to what degree treating the former will improve erectile function. [18] About 35-40% of men with low testosterone see an improvement in their erections with testosterone replacement; however, almost 65% of these men see no improvement. [16]
One study examined the role of testosterone supplementation in hypogonadal men with ED. These men were considered nonresponders to sildenafil, and their erections were monitored by assessing nocturnal penile tumescence (NPT). After these men were given testosterone transdermally for 6 months, the number of NPTs increased, as did the maximum rigidity with sildenafil. [19] This study suggests that a certain level of testosterone may be necessary for PDE5 inhibitors to function properly.
In a randomized double-blind, parallel, placebo-controlled trial, sildenafil plus testosterone was not superior to sildenafil plus placebo in improving erectile function in men with ED and low testosterone levels. [20] The objective of the study was to determine whether the addition of testosterone to sildenafil therapy improves erectile response in men with ED and low testosterone levels.
However, in contrast, a recent systematic review of published studies, the authors concluded that overall, the addition of testosterone to PDE-5 inhibitors might benefit patients with ED associated with testosterone levels of less than 300 ng/dL (10.4 nmol/L) who failed monotherapy. [21] A limitation of existing studies are their heterogeneous nature and methodological drawbacks.
The mechanisms by which testosterone plays a role in erectile function are not completely understood. A study evaluating the effect of testosterone on erections in surgically castrated rabbits and control animals, in which the rabbits’ intracavernosal pressures were compared after cavernosal nerve stimulation, determined that castrated rabbits had much lower pressures after stimulation than control rabbits did. [22] Notably, the pressures increased when castrated rabbits received exogenous testosterone replacement.
Another study compared the response of surgically and medically castrated rabbits to vardenafil with that of control rabbits. [23] Castrated rabbits did not respond to vardenafil, whereas noncastrated rabbits did respond appropriately. This result suggests that a minimum amount of testosterone is necessary for PDE5 inhibitors to produce an erection.
Another study found that castrated rats had erections if given testosterone alone or dihydrotestosterone (DHT) and 5-alpha reductase inhibitors but not if given testosterone and 5-alpha reductase inhibitors. [24] This finding suggests that DHT is the active component and is necessary at a certain level for rats to have an erection.
This study also measured intracavernosal pressure to monitor erections and NOS activity in the penile cytosol. [24] NO levels correlated with intracavernosal pressure, which suggests that testosterone and DHT act through NOS. Testosterone and DHT may act at the genomic level to stimulate production of NOS.
It appears that testosterone has NOS-independent pathways as well. In one study, castrated rats were implanted with testosterone pellets and then divided into a group that received an NOS inhibitor (L-nitro-L-arginine methyl ester [L-NAME]) and a control group that received no enzyme. [25] The castrated rats that were given testosterone pellets and L-NAME still had partial erections, a result suggesting the presence of a pathway independent of NOS activity.
Etiology
ED usually has a multifactorial etiology. Organic, physiologic, endocrine, and psychogenic factors are involved in the ability to obtain and maintain erections. In general, ED is divided into 2 broad categories, organic and psychogenic. Although most ED was once attributed to psychological factors, pure psychogenic ED is in fact uncommon; however, many men with organic etiologies may also have an associated psychogenic component.
Conditions that may be associated with ED include diabetes, [26, 27, 28] hypertension, [29] , atrial fibrillation, [30] and CAD, as well as neurologic disorders, endocrinopathies, benign prostatic hyperplasia, [31] , sleep apnea [32] , chronic obstructive pulmonary disease (COPD), [33] and depression (see Table 1 below). [34, 35, 36, 37] In fact, almost any disease may affect erectile function by altering the nervous, vascular, or hormonal systems. Various diseases may produce changes in the smooth muscle tissue of the corpora cavernosa or influence the patient’s psychological mood and behavior.
Table 1. Diseases and Conditions Associated With Erectile Dysfunction (Open Table in a new window)
Vascular causes |
Atherosclerosis Peripheral vascular disease Myocardial infarction Arterial hypertension Vascular injury from radiation therapy Vascular injury from prostate cancer treatment Blood vessel and nerve trauma (eg, from long-distance bicycle riding) Medications for treatment of vascular disease |
Systemic diseases |
Diabetes mellitus Scleroderma Renal failure Liver cirrhosis Idiopathic hemochromatosis Cancer and cancer treatment Dyslipidemia Hypertension |
Neurologic causes |
Epilepsy Stroke Multiple sclerosis Guillain-Barré syndrome Alzheimer disease Trauma |
Respiratory disease |
Chronic obstructive pulmonary disease Sleep apnea |
Endocrine conditions |
Hyperthyroidism Hypothyroidism Hypogonadism Diabetes |
Penile conditions |
Peyronie disease Epispadias Priapism |
Psychiatric conditions |
Depression Widower syndrome Performance anxiety Posttraumatic stress disorder |
Nutritional states |
Malnutrition Zinc deficiency |
Hematologic diseases |
Sickle cell anemia Leukemias |
Surgical procedures |
Brain and spinal cord procedures Retroperitoneal or pelvic lymph node dissection Aortoiliac or aortofemoral bypass Abdominal perineal resection Proctocolectomy Transurethral resection of the prostate Radical prostatectomy Cryosurgery of the prostate Cystectomy |
Medications |
Antihypertensives Antidepressants Antipsychotics Antiulcer agents (eg, cimetidine) 5-Alpha reductase inhibitors (eg, finasteride and dutasteride) Cholesterol-lowering agents Methadone |
Conditions associated with reduced nerve and endothelium function (eg, aging, hypertension, smoking, hypercholesterolemia, and diabetes) alter the balance between contraction and relaxation factors (see Pathophysiology). These conditions cause circulatory and structural changes in penile tissues, resulting in arterial insufficiency and defective smooth muscle relaxation. In some patients, sexual dysfunction may be the presenting symptom of these disorders.
Given the multiplicity of possible etiologic factors, it may be difficult to determine how much any given factor is contributing to the problem. A thorough evaluation is necessary for correct identification of the specific cause or causes in any given individual.
Vascular diseases
Vascular diseases account for nearly 50% of all cases of ED in men older than 50 years. These diseases include atherosclerosis, peripheral vascular disease, myocardial infarction (MI), and arterial hypertension.
Vascular damage may result from radiation therapy to the pelvis and prostate in the treatment of prostate cancer. [38] Both the blood vessels and the nerves to the penis may be affected. Radiation damage to the crura of the penis, which are highly susceptible to radiation damage, can induce ED. Data indicate that 50% of men undergoing radiation therapy lose erectile function within 5 years after completing therapy; fortunately, some respond to one of the PDE5 inhibitors.
Trauma
Trauma to the pelvic blood vessels or nerves can also lead result in ED. Bicycle riding for long periods has been implicated as an etiologic factor; direct compression of the perineum by the bicycle seat may cause vascular and nerve injury. [39] On the other hand, bicycling for less than 3 hours per week may be somewhat protective against ED. [39] Some of the newer bicycle seats have been designed to diminish pressure on the perineum. [39, 40]
Diabetes mellitus
Diabetes is a well-recognized risk factor for ED. A systematic review and meta-analysis found that the prevalence of ED was 37.5% in type 1 diabetes, 66.3% in type 2 diabetes, and 52.5% in diabetes overall—a rate approximately 3.5 times higher than that in controls. [41] The etiology of ED in diabetic men probably involves both vascular and neurogenic mechanisms. Evidence indicates that establishing good glycemic control can minimize this risk.
Abnormal cholesterol levels
The Massachusetts Male Aging Study (MMAS) documented an inverse correlation between ED risk and high-density lipoprotein (HDL) cholesterol levels but did not identify any effect from elevated total cholesterol levels. [16] Another study involving male subjects aged 45-54 years found a correlation with abnormal HDL cholesterol levels but also found a correlation with elevated total cholesterol levels. The MMAS included a preponderance of older men.
Respiratory diseases
Men with sleep disorders commonly experience ED. [42] Heruti et al recommended that in adult male patients, ED should be considered when a sleep disorder—especially sleep apnea syndrome—is suspected, and vice versa. [43]
Endocrine disorders
Hypogonadism that results in low testosterone levels adversely affects libido and erectile function. Hypothyroidism is a very rare cause of ED.
Penile conditions
Peyronie disease may result in fibrosis and curvature of the penis. Men with severe Peyronie disease may have enough scar tissue in the corpora to impede blood flow.
Mental health disorders
Mental health disorders, particularly depression, are likely to affect sexual performance. The MMAS data indicate an odds ratio of 1.82 for men with depression. Other associated factors, both cognitive and behavioral, may contribute. In addition, ED alone can induce depression.
Cosgrove et al reported a higher rate of sexual dysfunction in veterans with posttraumatic stress disorder (PTSD) than in veterans who did not develop this problem. [44] The domains on the International Index of Erectile Function (IIEF) questionnaire that demonstrated the most change included overall sexual satisfaction and erectile function. [45, 46] Men with PTSD should be evaluated and treated if they have sexual dysfunction.
Prostate surgery
Prostate surgery for benign prostatic hyperplasia has been documented to be associated with ED in 10-20% of men. This association is thought to be related to nerve damage from cauterization. Newer procedures (eg, microwave, laser, or radiofrequency ablation) have rarely been associated with ED.
Radical prostatectomy for the treatment of prostate cancer poses a significant risk of ED. A number of factors are associated with the chance of preserving erectile function. If both nerves that course on the lateral edges of the prostate can be saved, the chance of maintaining erectile function is reasonable. The odds depend on the age of the patient. Men younger than 60 years have a 75-80% chance of preserving potency, but men older than 70 years have only a 10-15% chance.
The Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE) study, designed to determine whether an individual man’s sexual outcomes after most common treatments for early-stage prostate cancer could be accurately predicted on the basis of baseline characteristics and treatment plans, found that 2 years after treatment, 177 (35%) of 511 men who underwent prostatectomy reported the ability to attain functional erections suitable for intercourse. [47]
In comparison, 37% of men who had received external radiotherapy as their primary therapy reported the ability to attain functional erections suitable for intercourse, along with 43% of men who had received brachytherapy as primary treatment. Pretreatment sexual health-related quality of life score, age, serum prostate-specific antigen (PSA) level, race or ethnicity, body mass index, and intended treatment details were associated with functional erections 2 years after treatment. [47]
After surgery, one of the oral PDE5 inhibitors (sildenafil, vardenafil, or tadalafil) is frequently used to assist in the recovery of erectile function. The benefit of penile rehabilitation therapy is under investigation, but results have been mixed. [48, 49]
Medications
ED is an adverse effect of many commonly prescribed medications. For example, some psychotropic drugs and antihypertensive agents are associated with ED. Persistent posttreatment ED is a listed adverse effect of the 5-alpha reductase inhibitors finasteride and dutasteride and of alpha blockers.
However, a review of a United Kingdom medical record database found no evidence that the use of 5-alpha reductase inhibitors independently increase the risk for ED. In 71,849 men with benign prostatic hyperplasia (BPH), the risk of ED was not increased with the use of finasteride or dutasteride only (odds ratio [OR] 0.94), or a 5-alpha reductase inhibitor plus an alpha blocker (OR 0.92) compared with an alpha blocker only. In addition, the risk of ED was not increase in 12 346 men prescribed finasteride 1 mg for alopecia, compared with unexposed men with alopecia (OR 0.95). The risk of ED did increase with longer duration of BPH, regardless of drug exposure. [50]
Lifestyle
Exercise and lifestyle modifications may improve erectile function. Weight loss may help by decreasing inflammation, increasing testosterone, and improving self-esteem. Patients should be educated to increase activity, reduce weight, and stop smoking, as these efforts can improve or restore erectile function in men without comorbidities. Precise glycemic control in diabetic patients and pharmacologic treatment of hypertension may be important in preventing or reducing sexual dysfunction. [51]
Smoking
Cigarette smoking has been shown to be an independent risk factor. In studies evaluating more than 6000 men, the risk of developing ED increased by a factor of 1.5.
Epidemiology
United States and international statistics
Sexual dysfunction is highly prevalent in men and women. In the MMAS, 52% of the respondents reported some degree of erectile difficulty. Complete ED, defined as (1) the total inability to obtain or maintain an erection during sexual stimulation and (2) the absence of nocturnal erections, occurred in 10% of the respondents. Mild and moderate ED occurred in 17% and 25% of responders, respectively. [16]
Although the rate of mild ED in the MMAS remained constant (17%) in men aged 40-70 years, the number of men reporting moderate ED doubled (17-34%) and the number of men reporting complete ED tripled (5-15%). If the MMAS data are extrapolated to the US population, an estimated 18-30 million men are affected by ED. [52]
In the National Health and Social Life Survey (NHSLS), a nationally representative probability sample of men and women aged 18-59 years, 10.4% of men reported being unable to achieve or maintain an erection during the past year. [53] There is a striking correlation with the proportion of men in the MMAS who reported complete ED.
Studies conducted around the world report similar risk factors and similar prevalence rates for ED. [54, 55]
Age-related demographics
All studies demonstrate a strong association with age, even when data are adjusted for the confounding effects of other risk factors. The independent association with aging suggests that vascular changes in the arteries and sinusoids of the corpora cavernosa, similar to those found elsewhere in the body, are contributing factors. Other risk factors associated with aging include depression, sleep apnea, and low HDL levels.
Long-term predictions based on an aging population and an increase in risk factors (eg, hypertension, diabetes, vascular disease, pelvic and prostate surgery, benign prostatic hyperplasia, and lower urinary tract symptoms) suggest a large increase in the number of men with ED. In addition, the prevalence of ED is underestimated because physicians frequently do not question their patients about this disorder.
Prognosis
In a prospective population-based study of 1709 men aged 40-70 years, Araujo et al found that ED was significantly associated with increased all-cause mortality. [56] The increase primarily resulted from cardiovascular mortality.
In a prospective study from the Prostate Cancer Prevention Trial database, Thompson et al reported that men presenting with ED had a significantly higher chance of developing a cardiovascular event over a 7-year follow-up period. [57] The hazard ratio was 1.45, which is in the range of risk associated with current smoking or a family history of MI.
An analysis of 14 studies involving more than 90,000 patients with ED confirmed the relation between ED and an increased risk of cardiovascular events and mortality. [58] Compared with patients without ED, those with ED had a 44% increased risk of cardiovascular events, a 25% increased risk of all-cause mortality, a 62% increased risk of MI, and a 39% increased risk of cerebrovascular events. Treatment of ED, either through lifestyle interventions or by pharmacologic means, may improve prognosis and reduce risk.
Associated morbidity may include various other male sexual dysfunctions, such as premature (early) ejaculation and male hypoactive sexual desire disorder. The NHSLS found that 28.5% of men aged 18-59 years reported premature ejaculation, and 15.8% lacked sexual interest during the past year. An additional 17% reported anxiety about sexual performance, and 8.1% had a lack of pleasure in sex. [53]
Men with ED may also experience anxiety or depression [59] . Erectile disorder is common in men with lower urinary tract symptoms related to BPH.
Patient Education
The laboratory results should be discussed with the patient and, if possible, with his sexual partner. This educational process allows a review of the basic aspects of the anatomy and physiology of the sexual response and an explanation of the possible etiology and associated risk factors (eg, smoking and the use of various medications). Treatment options and their benefits and risks should be discussed. This type of dialogue allows the patient and physician to cooperate in developing an optimal management strategy.
Patients with both ED and cardiovascular disease who receive treatment with an oral PDE5 inhibitor require education regarding what to do if anginal episodes develop while the drug is in their system. Such education includes stressing the importance of alerting emergency care providers to the presence of the drug so that nitrate treatment is avoided.
Patients receiving penile prostheses should be instructed in the operation of the prosthesis before surgery and again in the postoperative period. The prosthesis usually is not activated until approximately 6 weeks after surgery, so as to allow the edema and pain to subside. The prosthesis is checked in the office before the patient begins to use it.
For patient education information, see the Erectile Dysfunction Health Center
-
These images depict penile anatomy. Note the sinusoidal makeup of the corpora and thick fascia (ie, Buck fascia) that covers the corpora cavernosa. The major blood vessels to the corpora cavernosa enter through tributaries from the main vessels running along the dorsum of the penis.
-
Vascular anatomy of the penis.
-
This penile tumescence monitor is placed at the base and near the corona of the penis. It is connected to a monitor that records a continuous graph depicting the force and duration of erections that occur during sleep. The monitor is strapped to the leg. The nocturnal penile tumescence test is conducted on several nights to obtain an accurate indication of erections that normally occur during the alpha phase of sleep.
-
The presence of normal skin sensation adequate to produce an erection is measured with this device.
-
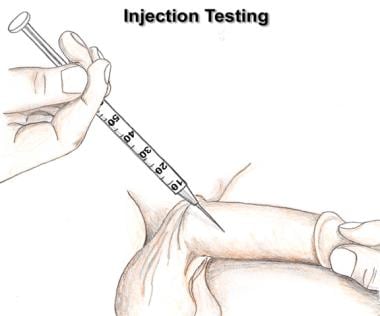
A vasodilator such as prostaglandin E1 can be injected into one of the corpora cavernosa. If the blood vessels are capable of dilating, a strong erection should develop within 5 minutes.
-
Erectile dysfunction. This diagram depicts a cross-section of penile anatomy and is used to instruct patients in the technique of administering intracorporeal medications.
-
The Medicated Urethral System for Erections (MUSE) is a small suppository placed into the urethra with this device.
-
This image depicts a vacuum device used to produce an erection (also see next image). In this image, the elements are shown. They include the cylinder, a pump to create a vacuum, and a constriction ring to be placed at the base of the penis after an erection has been obtained in order to maintain the erection.
-
This image demonstrates the vacuum device in place (see previous image). Note the presence of the constricting ring at the base of the penis.
-
This is one of many types of constricting devices placed at the base of the penis to diminish venous outflow and improve the quality and duration of the erection. This is particularly useful in men who have a venous leak and are only able to obtain partial erections that they are unable to maintain. These constricting devices may be used in conjunction with oral agents, injection therapy, and vacuum devices.
-
Two rigid cylinders have been placed into the corpora cavernosa. This type of implant has no inflation mechanism but provides adequate rigidity to the penis to allow penetration.
-
This inflatable penile prosthesis has 3 major components. The 2 cylinders are placed within the corpora cavernosa, a reservoir is placed beneath the rectus muscle, and the pump is placed in the scrotum. When the pump is squeezed, fluid from the reservoir is transferred into the 2 cylinders, producing a firm erection. The deflation mechanism is also located on the pump and differs by manufacturer.