Practice Essentials
Adrenal hemorrhage is a relatively uncommon condition with a variable and nonspecific presentation that may lead to acute adrenal crisis, shock, and death unless it is recognized promptly and treated appropriately. [1, 2, 3] Several risk factors have been associated with adrenal hemorrhage, based on case reports. Its pathologic characteristics typically include bilateral gland involvement with extensive necrosis of all 3 cortical layers and of medullary adrenal cells. Retrograde migration of medullary cells into the zona fasciculata, widespread hemorrhage into the adrenal gland that may extend into the perirenal fat, and, frequently, adrenal vein thrombosis may occur. Computed tomography (CT) scanning of the adrenals (thin slice) is the study of choice for demonstrating adrenal hemorrhage in the acute setting. [4] However, it is practical only in hemodynamically stable patients.
CT scan appearance is shown in the image below.
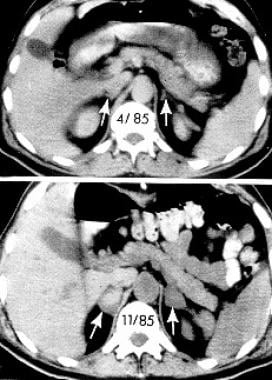 Computed tomographic (CT) scans of the abdomen show normal adrenal glands several months before the onset of hemorrhage (upper panel) and enlarged adrenals 2 weeks after an acute episode of bilateral adrenal hemorrhage (lower panel). The attenuation of the adrenal glands, indicated by arrows, is increased after the acute event. Reproduced from Rao RH, Vagnucci AH, Amico JA: Bilateral massive adrenal hemorrhage: early recognition and treatment. Ann Intern Med. Feb 1 1989;110(3):227-35 with permission from the journal.
Computed tomographic (CT) scans of the abdomen show normal adrenal glands several months before the onset of hemorrhage (upper panel) and enlarged adrenals 2 weeks after an acute episode of bilateral adrenal hemorrhage (lower panel). The attenuation of the adrenal glands, indicated by arrows, is increased after the acute event. Reproduced from Rao RH, Vagnucci AH, Amico JA: Bilateral massive adrenal hemorrhage: early recognition and treatment. Ann Intern Med. Feb 1 1989;110(3):227-35 with permission from the journal.
Signs and symptoms of adrenal hemorrhage
Pain that is nonspecific in location and quality is a very consistent feature of adrenal hemorrhage.
Fever (ie, temperature >38°C) is present in 50-70% of patients with adrenal hemorrhage, representing the most frequent finding in this condition.
Tachycardia has been reported in approximately 40-50% of patients early in the course of extensive, bilateral adrenal hemorrhage, and without aggressive therapy, it may progress to shock.
Fatigue, weakness, dizziness, arthralgias, myalgias, anorexia, nausea, vomiting, and diarrhea, which are present in approximately 50% of extensive, bilateral adrenal hemorrhage cases, are indicative of acute adrenal insufficiency.
A characteristic skin rash with a typical evolution occurs in approximately 75% of patients with Waterhouse-Friderichsen syndrome.
Workup in adrenal hemorrhage
Lab studies
A complete blood count (CBC) and differential generally are obtained to assist with therapeutic decisions, although these test results are nonspecific.
Serum electrolytes, blood urea nitrogen (BUN), creatinine, and plasma glucose may be of limited diagnostic use, but they also should be obtained to assist with patient management.
Serum cortisol, plasma adrenocorticotropic hormone (ACTH), serum aldosterone, and plasma renin activity (PRA) always should be obtained in suspected adrenal hemorrhage cases, because they provide important information on adrenal function.
The short cosyntropin (Cortrosyn) stimulation test confirms the diagnosis of adrenal insufficiency.
Imaging studies
Imaging studies in the workup of adrenal hemorrhage include the following:
-
CT scanning - CT scanning of the adrenals (thin slice) is the study of choice for demonstrating adrenal hemorrhage in the acute setting; [4] however, it is practical only in hemodynamically stable patients
-
Ultrasonography - Ultrasonographic examination of the adrenals (including Doppler ultrasonography) is quite helpful in neonatal adrenal hemorrhage cases, and it may reveal the presence of adrenal hemorrhage in utero; in older children or adults, ultrasonographic examination may be employed at the bedside, although it is operator dependent and may be limited by large body habitus
Management of adrenal hemorrhage
Medical therapies are used to replace adrenal function, to provide vital function support as needed, to treat underlying condition(s), and to correct fluid, electrolyte, and red cell mass deficits.
Adrenalectomy (open or laparoscopic) may be performed. However, surgery generally is not required in cases of nontraumatic adrenal hemorrhage, except in patients with primary adrenal tumors or in rare cases, of extensive retroperitoneal hemorrhage secondary to adrenal hemorrhage.
In traumatic adrenal hemorrhage cases, surgery may be necessary for the treatment of associated injuries, the exploration of penetrating wounds, or the control of bleeding.
Pathophysiology
Although the precise mechanisms leading to adrenal hemorrhage are unclear in nontraumatic cases, available evidence has implicated adrenocorticotropic hormone (ACTH), adrenal vein spasm and thrombosis, and the normally limited venous drainage of the adrenal in the pathogenesis of this condition.
The adrenal gland has a rich arterial supply, in contrast to its limited venous drainage, which is critically dependent on a single vein. Furthermore, in stressful situations, ACTH secretion increases, which stimulates adrenal arterial blood flow that may exceed the limited venous drainage capacity of the organ and lead to hemorrhage.
In addition, adrenal vein spasm induced by high catecholamine levels secreted in stressful situations and by adrenal vein thrombosis induced by coagulopathies may lead to venous stasis and hemorrhage. Adrenal vein thrombosis has been found in several patients with adrenal hemorrhage, and it may occur in association with sepsis, heparin-induced thrombocytopenia, [7] primary antiphospholipid antibody syndrome, or disseminated intravascular coagulation (DIC).
Regardless of the precise mechanisms, extensive, bilateral adrenal hemorrhage commonly leads to acute adrenal insufficiency and adrenal crisis, unless it is recognized and treated promptly.
Epidemiology
Frequency
United States
Adrenal hemorrhage has been reported in 0.3-1.8% of unselected cases in autopsy studies, although extensive bilateral adrenal hemorrhage may be present in 15% of individuals who die of shock.
Mortality/Morbidity
Acute adrenal insufficiency (adrenal crisis) may occur in association with extensive, bilateral adrenal hemorrhage, and it is uniformly fatal if unrecognized and untreated. In contrast, unilateral adrenal hemorrhage is not associated with acute adrenal insufficiency.
Patients with adrenal hemorrhage may die because of underlying disease or diseases associated with adrenal hemorrhage, despite treatment with stress-dose glucocorticoids. Overall, adrenal hemorrhage is associated with a 15% mortality rate, which varies according to the severity of the underlying illness predisposing to adrenal hemorrhage. For example, patients with Waterhouse-Friderichsen syndrome (adrenal hemorrhage occurring in sepsis, most frequently meningococcal) have a 55-60% mortality rate. [8]
Chronic adrenal insufficiency occurs in most patients who survive extensive, bilateral adrenal hemorrhage, necessitating long-term glucocorticoid replacement. In contrast, the need for mineralocorticoid replacement is variable. Androgen replacement therapy may also be beneficial in women with chronic adrenal insufficiency. Rare case reports exist of patients who had complete recovery of adrenal function after an episode of extensive, bilateral adrenal hemorrhage and acute adrenal insufficiency.
Sex
Extensive, bilateral adrenal hemorrhage is more common in males (male-to-female ratio of 2:1), probably reflecting a male predilection for several of the underlying conditions associated with adrenal hemorrhage.
Age
Although adrenal hemorrhage may occur in people of any age, most patients with nontraumatic, extensive, bilateral adrenal hemorrhage are aged 40-80 years at the time of the acute event. In contrast, patients with traumatic adrenal hemorrhage typically are in the second to third decade of life.
Most patients with Waterhouse-Friderichsen syndrome are in the pediatric age group, although adults have infrequently been affected.
Adrenal hemorrhage in neonates is a well-described entity and has even been diagnosed in utero. A full discussion of this entity is beyond the scope of this review.
-
Computed tomographic (CT) scans of the abdomen show normal adrenal glands several months before the onset of hemorrhage (upper panel) and enlarged adrenals 2 weeks after an acute episode of bilateral adrenal hemorrhage (lower panel). The attenuation of the adrenal glands, indicated by arrows, is increased after the acute event. Reproduced from Rao RH, Vagnucci AH, Amico JA: Bilateral massive adrenal hemorrhage: early recognition and treatment. Ann Intern Med. Feb 1 1989;110(3):227-35 with permission from the journal.










