Practice Essentials
A vascular ring is an unusual congenital condition in which the anomalous configuration of the arch, associated vessels, or both surrounds the trachea and esophagus, forming a complete or incomplete ring around them. [1, 2] Several other related vascular anomalies involving arch vessels do not form a complete ring but have been grouped descriptively with vascular rings because they produce similar symptoms related to compression of the trachea or esophagus. Both complete and incomplete rings are discussed in this article.
The first vascular ring described was a double aortic arch noted by Hommel in 1737. Bayford reported a retroesophageal right subclavian artery in 1794 after performing an autopsy on a woman who had experienced dysphagia for years and died of starvation. Maude Abbott described five cases of double aortic arch in 1932 and made the suggestion that surgical intervention should be undertaken in such cases.
Finally, in 1945, Gross used the term vascular ring in the New England Journal of Medicine publication that he wrote after performing the first successful division of a double aortic arch. Since that time, numerous reports of successful treatment have occurred, and the forms of aortic arch anomalies causing this problem have been well delineated.
The primary symptomatology associated with vascular rings relates to the structures that are encircled by the ring, chiefly the trachea and esophagus. Prompt diagnosis and treatment of these congenital abnormalities can be lifesaving.
Because vascular rings are not common, missed diagnosis is much more common than with other congenital heart disorders. For healthcare providers who look after pediatric patients, a high degree of suspicion, coupled with the appropriate imaging study, is required to make the diagnosis. A multimodality imaging approach (eg, with magnetic resonance imaging [MRI], computed tomography [CT], and esophagography) is often required for correct diagnosis (see Workup).
Surgical division of a vascular ring is indicated in all symptomatic patients. To avoid serious complications, surgery should not be delayed, especially in patients with symptoms of airway compression. Individuals who have no symptoms from a vascular ring may not require surgical intervention. Surgical repairs in most cases can be performed successfully and without long-term morbidity (see Treatment). [3, 4]
Anatomy
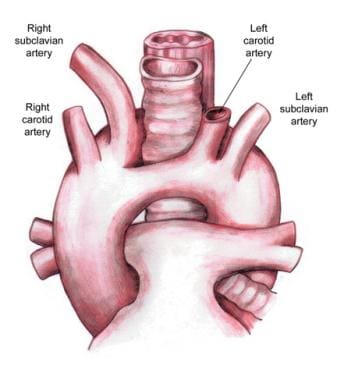
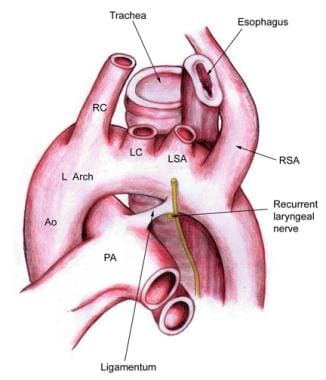
Double aortic arch
Visualization through a left thoracotomy shows a normally positioned left (anterior) arch exiting the pericardium and joining the left-side descending thoracic aorta after giving off the left subclavian artery. The ligament arteriosum is positioned normally. The posterior (right) arch joins the descending thoracic aorta at the same level as the anterior arch but reaches that point from an extreme posterior course behind the esophagus. Often, the posterior arch is visible only after circumferential dissection of the aorta at the level of its junction with the anterior arch. (See the image below.)
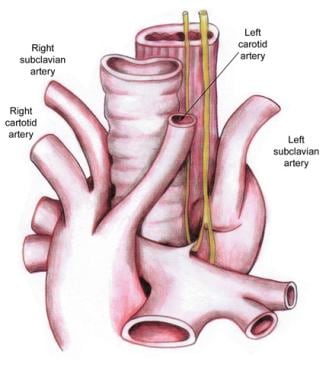
Right aortic arch with retroesophageal left subclavian artery and left ligamentum arteriosum
The arch travels to the right and behind the esophagus, joining the left-side descending aorta. As it takes this course, it gives off the left carotid artery first. Then, it sequentially gives off the right carotid, right subclavian, and left subclavian arteries. This last branch often has a retroesophageal position. The ligamentum arteriosum courses from the base of the left subclavian artery to the left pulmonary artery. (See the image below.)
Through a left thoracotomy, the structures visible in normal position are the descending thoracic aorta and the distal portion of the left subclavian artery. These structures can be traced proximally to identify the site where the left subclavian artery exits the right arch as it joins with the descending aorta. The ligamentum arteriosum can be found at the base of the subclavian artery and traced towards the pulmonary artery.
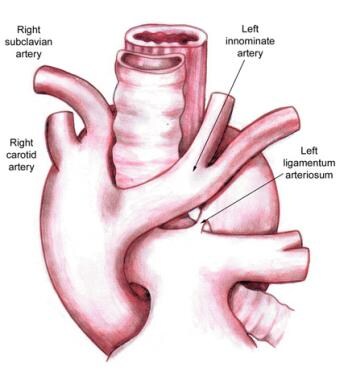
Right aortic arch with mirror-image branching and retroesophageal ligamentum arteriosum
In the rightward and retroesophageal course, the aortic arch gives off a left innominate artery, which in turn branches into the left carotid and subclavian arteries. The right carotid artery then branches from the arch, followed by the right subclavian. The ligamentum arteriosum exits distal to this point from the area of the Kommerell diverticulum and courses to the left pulmonary artery. (See the image below.)
As viewed through a left thoracotomy, the descending thoracic aorta is visible and can be traced proximally to the area of its merger with the right aortic arch, which joins it from behind the esophagus. In this area, the ductus diverticulum and ligamentum arteriosum can be found.
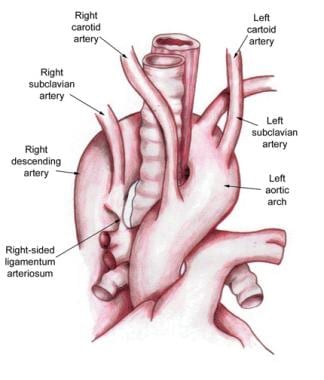
Left aortic arch with right descending thoracic aorta and right ligamentum arteriosum
The arrangement of this anomaly is the mirror image of right aortic arch with retroesophageal left subclavian artery and left ligamentum arteriosum. Approached through a right thoracotomy, structures are identified and traced in the same manner. (See the image below.)
Left aortic arch with right descending aorta and atretic right arch
In a retroesophageal position, the left arch passes to the left of the trachea to join the right descending thoracic aorta. The surgical view is via a right thoracotomy. At the level of this junction and immediately superior to a right ligamentum arteriosum, an atretic right arch is found. The brachiocephalic vessels in this case exit the left arch in a normal sequence.
Anomalous innominate artery
The brachiocephalic vessels exit the left arch in the normal sequence. The innominate artery may be more distally positioned and leftward on the arch than normal.
Retroesophageal right subclavian artery with left aortic arch and left ligamentum arteriosum
Rather than an innominate artery exiting the arch as the normal first brachiocephalic branch, the right carotid is the first brachiocephalic vessel. It is followed by the left carotid and then the left subclavian artery. The right subclavian artery is the last brachiocephalic branch to exit the arch, and it takes a course rightward and posterior to the esophagus. The ligamentum arteriosum is normally positioned on the left. (See the image below.)
Anomalous left pulmonary artery (pulmonary artery sling)
Instead of the normal pulmonary artery configuration, in which the main pulmonary artery gives rise to the right and left pulmonary arteries, the main pulmonary artery continues behind the ascending aorta and rightward as the right pulmonary artery, which then gives off the left pulmonary artery. The left pulmonary artery passes from right to left between the trachea and esophagus in its course to the left lung. The ligamentum arteriosum takes a course from the junction of the main and right pulmonary arteries posteriorly to the aorta. (See the image below.)
Pathophysiology
In spite of the significant variability in this group of structural abnormalities of the aortic arch, they all possess a common feature: They all produce some degree of compression on the major airway structures, the esophagus, or both. The location and severity of compression varies with the configuration of the lesion. Individuals with anomalies producing more severe compression are likely to present earlier in life.
Tracheal or tracheobronchial malacia and stenosis may develop in association with some of these lesions in the areas where the greatest degree of compression exists. This is particularly true in cases of anomalous left pulmonary artery.
Other congenital cardiac anomalies may be present in association with aortic arch anomalies.
The presence of a right aortic arch should always raise the suspicion of additional congenital cardiac disease. Right aortic arch has been reported in as many as 34% of cases of tetralogy of Fallot. Other intracardiac lesions found in association with a right aortic arch include double-outlet right ventricle, truncus arteriosus, ventricular septal defect with pulmonary atresia, transposition of the great vessels, tricuspid atresia, and absent left pulmonary artery.
Anomalous left pulmonary artery has also been associated with other cardiac defects in as many as 50% of cases. These include the aforementioned lesions, as well as persistent left superior vena cava (SVC), atrial septal defect, and ventricular defect. Complete tracheal rings (congenital absence of the membranous trachea) resulting in tracheal stenosis are another anomaly reported in as many as 50% of infants with anomalous left pulmonary artery. The combination of these two lesions is often termed the ring-sling complex.
Etiology
The various forms of this anomaly occur very early in embryologic development. They result from the abnormal or incomplete regression of one of the six embryonic branchial arches. Several papers have reported the close association of band 22q11 deletion with anomalies of the aortic arch, as well as other congenital cardiac abnormalities. [5]
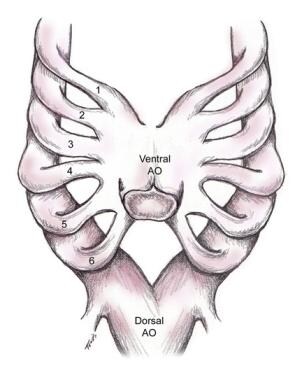
Early in normal development, both a dorsal and a ventral aortic arch are present. The two arches are connected by six embryonic branchial arches (see the image below). The third, fourth, and sixth embryonic arches are the most crucial in the development of the aortic arch and several of its major branches, as well as the ductus arteriosus and the main pulmonary arteries.
In normal development, each primitive arch either progresses into a functional vascular structure or involutes as follows:
-
The right and left first and second arches become a portion of the arterial supply to the face
-
The third arches develop into the carotid arteries
-
The dorsal aorta between the third and fourth arches involutes
-
The fourth arches are the primary contributors to the aortic arch itself, with the proximal right fourth arch developing into the proximal right subclavian artery; the distal portion of the right fourth arch involutes at the point where it joins the dorsal arch; the left fourth arch remains as the aortic arch in normal development
-
The fifth arches involute bilaterally
-
The ventral right sixth arch becomes the proximal right pulmonary artery; the ventral portion of the left sixth arch develops into the left pulmonary artery, while the dorsal portion becomes the ductus arteriosus
-
The entire left and the distal right subclavian arteries arise from the seventh segmental arterial branches of the dorsal aorta
Abnormal arch development (see Anatomy) results when one or more of the necessary involutions or other changes in embryonic arch structures does not occur.
Double aortic arch
The classic double aortic arch develops when involution of the distal right fourth arch does not take place. The fourth right and left arches both persist and join the left-side descending thoracic aorta. The right and left aortic arches encircle the trachea and the esophagus. In about 30% of cases of double aortic arch, the smaller, or less dominant, of the arches is atretic but remains in continuity with the descending aorta, maintaining the complete ring.
The double aortic arch forms a ring around the trachea and esophagus, compressing both of these structures. Tracheoesophageal compression typically results in early symptoms. This type of defect is rarely associated with intracardiac defects.
The Kommerell diverticulum, though more commonly associated with a right aortic arch (see below), has been known to occur with a double aortic arch as well. [6]
Abnormalities associated with right aortic arch
When the left fourth branchial arch involutes and the right remains, a right aortic arch is present. Right aortic arch occurs less frequently than 1 in 100,000 times in the general population and may exist in the absence of any other anomalies. Its presence is suggestive of the existence of an associated anomaly. About 30% of patients with tetralogy of Fallot have an associated right aortic arch.
Persistence of the right arch with involution of the left creates a situation in which the origins of the left subclavian artery and ductus arteriosus can vary. Several of these configurations can produce a vascular ring.
Right aortic arch with aberrant left subclavian artery and left ligamentum arteriosum
In this anomaly, the right arch first gives off the left carotid artery, which travels anterior to the trachea. It then gives off the right carotid, followed by the right subclavian artery and, finally, the left subclavian artery, which courses in a retroesophageal position and gives rise to the ligamentum arteriosum from its base.
The ligamentum arteriosum connects the left subclavian or descending aorta to the left pulmonary artery. The trachea and esophagus are surrounded by the ascending aorta anteriorly, the aortic arch on the right, the descending aorta posteriorly, and the ligamentum arteriosum and left pulmonary artery on the left. Almost 10% of these defects are associated with an intracardiac defect.
Right aortic arch with mirror-image branching and retroesophageal ligamentum arteriosum
In these cases, only partial resorption of the distal left fourth arch occurs. The first brachiocephalic vessel originating from the right arch is the left innominate artery, which, in turn, branches into a left carotid and a left subclavian artery. These vessels course anterior to the trachea.
Following these, a right carotid artery and then a right subclavian artery arise. The ligamentum arteriosum is the final structure arising from the arch in this sequence. It originates from the Kommerell diverticulum, an area that represents the nonresorbed remnant of the left fourth arch and is situated at the point of merger between the right arch and the proximal descending thoracic aorta.
The ligamentum passes leftward and behind the esophagus and then travels anteriorly to join with the left pulmonary artery and complete the ring. More commonly, in cases of right aortic arch with mirror-image branching, the ligamentum arteriosum travels from the mirror-image innominate or left subclavian artery to the left pulmonary artery. A complete ring is not present in these cases. This type of vascular ring has a greater than 90% association with intracardiac defects.
Vascular rings associated with left aortic arch
Two extremely rare complete rings occur in the presence of a left aortic arch, and both are associated with a right-side descending thoracic aorta.
Left aortic arch with right descending aorta and right ligamentum arteriosum
The first arch vessel to exit the left aortic arch is the right common carotid, which passes anterior to the trachea. The left carotid is next, followed by the left subclavian artery. The right subclavian artery arises more distally as a branch of the proximal right-side descending aorta. The ligamentum arteriosum arises from the base of the right subclavian artery or a nearby diverticulum and travels to the right pulmonary artery.
Left aortic arch, right descending aorta, and atretic right aortic arch
The brachiocephalic vessels arise from the left-side arch in a normal arrangement. The left arch passes behind the esophagus to join a right-side descending aorta. An atretic right arch is present and completes the ring.
Arch abnormalities producing compression symptoms without anatomic ring
Anomalous innominate artery
The actual prevalence of this abnormality has been widely debated. This is because in as many as 90% of cases where symptomatic tracheal compression is produced by the innominate artery, the vessel is noted angiographically to have a normal origin from the aorta. When an anatomic abnormality is noted in these cases, the innominate artery appears to originate from a more distal and leftward position on the arch than normal. As it takes its course from left to right, it crosses the trachea anteriorly and in doing so may produce compression of the trachea.
Anomalous innominate artery is a rare cause of tracheomalacia or stenosis. It is exclusively seen in the pediatric population. This condition occurs as a consequence of the abnormal takeoff of the innominate artery, which results in anterior compression of the trachea. As the artery crosses over anteriorly, it impinges on the trachea at the level of the thoracic inlet. Classic symptoms of innominate artery compression syndrome include the following:
-
Asthmalike symptoms
-
Stridor
-
Apneic spells
-
Dyspnea
-
Recurrent lung infections
The diagnosis of innominate artery compression syndrome is not easy and may require imaging studies along with bronchoscopy. The majority of these children or infants present airway-obstructive symptoms that do not improve with conventional treatments. Once the diagnosis is made, all symptomatic infants must be referred to a surgeon.
This is one vascular disorder of the aortic arch that is repaired via a median sternotomy. The operation involves an aortopexy wherein the aortic arch is stabilized with sutures and the innominate artery is anchored to the posterior sternum so that it no longer compresses the trachea. With time, the angle of the innominate artery takeoff shifts, and the tracheal compression no longer occurs.
Retroesophageal right subclavian artery with left aortic arch and left ligamentum arteriosum
This is the most common of the arch-vessel anomalies, occurring in about 0.5% of the population. In these cases, the right subclavian artery does not arise from an innominate trunk with the right carotid artery but originates as the last brachiocephalic branch from the descending aorta and takes a retroesophageal route to its destination.
A normally positioned ligamentum arteriosum is present on the left. If a right ligamentum arteriosum were present instead of one on the left, its course would proceed from the base of this anomalous right subclavian artery to the right pulmonary artery, and a complete ring would exist. Instead, no true vascular ring is present in these cases. Most patients are symptomatic, but the occasional patient may present with dysphagia.
Anomalous left pulmonary artery or pulmonary sling
This abnormality occurs when the left main pulmonary artery arises as a branch of the right pulmonary artery instead of originating from the main pulmonary artery. This is believed to be an abnormality related to sixth aortic arch development. In this anomaly, the left pulmonary artery leaves the right and courses in a position cephalad to the right mainstem bronchus, proceeding around the right side of the trachea. It then travels between the trachea and esophagus as it goes to the left lung.
This lesion is often associated with hypoplasia and other abnormalities of the tracheal and bronchial cartilages. Most patients are symptomatic by 1 month after birth. Because the most severe compression is on the trachea, respiratory symptoms predominate. More than 50% of infants also have severe tracheobronchial anomalies, such as tracheomalacia, stenosis, webs, or complete tracheal rings. Intracardiac defects are also seen in 20% of these infants.
Epidemiology
Vascular rings are uncommon anomalies and make up fewer than 1% of all congenital cardiac defects. They occur with about equal frequency in both sexes. No geographical or racial predominance exists. Some vascular rings are associated with other congenital heart defects; others may be isolated deficits.
The two most common types of complete vascular rings are double aortic arch and right aortic arch with left ligamentum arteriosum. These make up 85-95% of the cases. [7, 8, 2]
Two other complete vascular rings that are extremely rare (< 1%) are (1) right aortic arch with mirror-image branching and (2) left ligamentum arteriosum and left aortic arch with retroesophageal right subclavian artery, right-side descending aorta, and right ligamentum arteriosum.
Other named anomalies that produce symptoms but do not form a complete anatomic vascular ring make up the remainder and include the abnormally placed or anomalous innominate artery and the retroesophageal right subclavian artery with left-side aorta and left ligamentum arteriosum.
The anomalous left pulmonary artery or pulmonary artery sling makes up about 10% of cases, though the exact number is difficult to determine because there are so few case reports. [9] Although the pulmonary artery sling is not associated with the aortic arch or its branches, it arises from an abnormality of the sixth branchial arch and produces a complete ring. This anomaly is associated with intracardiac defects in 10-15% of cases.
Prognosis
About 95% of patients who undergo surgical correction of a vascular ring survive for long periods, and most of these are soon relieved of their symptoms. In those infants with no intracardiac or extracardiac defects, surgery for vascular rings carries essentially no mortality.
Among those with less optimal long-term results are patients with an anomalous left pulmonary artery with and without complete tracheal rings and those with severe associated congenital cardiac defects. In those patients with a severely deformed trachea or tracheomalacia, additional reconstruction procedures may be required in the future.
In a series reported by Backer et al, reoperation proved necessary for 26 of 300 patients who had undergone surgical intervention for vascular rings. [10] The four primary indications for reoperation were Kommerell diverticulum (18 patients), circumflex aorta (2 patients), residual scarring (2 patients), and tracheobronchomalacia necessitating aortopexy (4 patients).
A number of patients continue to show evidence of some pulmonary function abnormalities years after surgery. Several studies report that measured pulmonary function studies show some degree of airway obstruction in as many as 50% of patients 7-8 years postoperatively. Also, a large number of patients appear to have a pronounced bronchial responsiveness to histamine.
Naimo et al reported long-term outcomes of complete vascular ring division in 132 children from a 36-year experience at a single institution (median follow-up, 11.4 y; range, 44 d to 36 y). [11] In-hospital mortality was 1.5% (2/132), and no late deaths occurred. Overall survival was 98.3 ± 1.2% at 20 years. After surgical treatment, three patients experienced persistent tracheal compression, and 16 had tracheomalacia. The freedom-from-reoperation rate was 88.6 ± 4.0%. None of the patients required tracheal surgery during the follow-up period.
François et al assessed early and late outcomes (mean follow-up, 7.8 ± 5.8 y) in 62 patients (median age, 1 y) who underwent surgical treatment of a vascular ring (most commonly a double aortic arch [53%]). [12] Median extubation time was 4 hours, and median hospital stay was 5 days. Early mortality was 8% and was associated with the anatomic diagnosis, concomitant anomalies, and the need for preoperative intubation. At 1 month, 63% of patients were free of residual symptoms; at 6 months, 82% were. At final follow-up, the rate of freedom from inhalation therapy was 82%.
-
Slide tracheoplasty and left pulmonary artery sling repair. Procedure performed by Giles Peek MD, FRCS, CTh, FFICM, The Children’s Hospital at Montefiore, Bronx, NY.
-
Embryonic aortic arch with dorsal and ventral arches and 6 branchial arches on right and left.
-
Double aortic arch.
-
Right aortic arch with aberrant left subclavian artery and left ligamentum arteriosum.
-
Right aortic arch with mirror-image branching and retroesophageal ligamentum arteriosum.
-
Left aortic arch with right descending aorta and right ligamentum arteriosum.
-
Retroesophageal right subclavian artery with left aortic arch and left ligamentum arteriosum.
-
Aberrant left pulmonary artery or pulmonary artery sling.
-
Barium esophagogram of 30-year-old woman with vascular ring.
-
Single-stage correction of transposition of great arteries with ventricular septal defect, hypoplastic right aortic arch with bilateral ductuses, and aberrant left subclavian artery arising from left duct in newborn. Procedure performed by Giles Peek MD, FRCS, CTh, FFICM, The Children’s Hospital at Montefiore, Bronx, NY.