Overview
Delivery of direct current (DC) shocks to the heart has long been used successfully to convert abnormal heart rhythms back to normal sinus rhythm. In 1775, Abildgaard reported using electricity to both induce and revive a hen from lifelessness. [1] Beck was the first physician to use DC defibrillation on a human to treat ventricular fibrillation (VF, vfib) in a 14-year-old during cardiac surgery in 1947. Fifteen years later, Lown applied synchronized DC shocks to the heart to convert atrial fibrillation (AF, afib) and ventricular tachycardia (VT, vtach) to normal sinus rhythm. [2]
Cardioversion is defined as a “synchronized DC discharge, and … does not apply to ventricular defibrillation or to the pharmacologic reversion of arrhythmias.” [3, 4] It is typically used to terminate life-threatening or unstable tachycardic arrhythmia (unstable ventricular and supraventricular rhythms) in patients who still have a pulse but who are hemodynamically unstable. [5] The DC electrical discharge is synchronized with the R or S wave of the QRS complex. Synchronization in the early part of the QRS complex avoids energy delivery near the apex of the T wave in the surface electrocardiogram (ECG), which coincides with a vulnerable period for induction of ventricular fibrillation. The peak of the T wave represents the terminal portion of the refractory state when adjacent heart fibers are in differing states of repolarization.
Defibrillation refers to an unsynchronized discharge of energy and is only recommended for ventricular fibrillation. It is used in patients who are in cardiac arrest. [5]
Basic principles
Transient delivery of an electrical current causes a momentary depolarization of most cardiac cells, thereby allowing the sinus node to resume normal pacemaker activity. In the presence of a reentrant-induced arrhythmia, such as paroxysmal supraventricular tachycardia (PSVT) and ventricular tachycardia (VT), electrical cardioversion interrupts the self-perpetuating circuit and restores a sinus rhythm. Electrical cardioversion is much less effective in treating arrhythmia caused by increased automaticity (eg, digitalis-induced tachycardia, catecholamine-induced arrhythmia) because the mechanism of the arrhythmia remains after the arrhythmia is terminated and therefore is likely to recur. [6]
At present, two types of defibrillators are in use for external cardioversion and defibrillation: a monophasic sinusoidal waveform (positive sine wave) and a biphasic truncated waveform. In 1997, a low-energy, impedance-compensating biphasic waveform was evaluated for atrial and ventricular arrhythmia management. This defibrillator automatically adjusted to the patient's transthoracic impedance, which is a feature that the monophasic models lack. Currently, there are several biphasic devices with similar efficacy available on the market.
The more recent use of biphasic cardioversion has shown that less energy is required to convert an arrhythmia to a normal sinus rhythm than with monophasic cardioversion. Consequently, use of biphasic energy results in fewer delivered shocks to the patient and less cumulative energy delivered. Potential benefits include fewer burn wounds, less tissue damage, and reduced damage to the heart muscle than is found with higher voltage shocks.
Indications
Cardioversion can be utilized to convert any arrhythmia that is not felt or that is known to be not incessant.
External cardioversion
Based on advanced cardiac life support (ACLS) guidelines, any patient with a narrow or wide QRS complex tachycardia (ventricular rate >150 beats per minute [bpm]) who is unstable (eg, chest pain, pulmonary edema, lightheadedness, hypotension) should be immediately treated with synchronized electrical cardioversion. [7] Synchronization to an R or S wave prevents the delivery of a shock during the vulnerable period of cardiac repolarization when ventricular fibrillaiton (VF, vfib) can be induced.
Synchronized electrical cardioversion may also be used to treat stable ventricular tachycardia (VT, vtach) that does not respond to a trial of intravenous medications. It is also recommended for the treatment of the following arrhythmias [8] :
-
Supraventricular tachycardia (SVT) due to reentry
-
Atrial fibrillation (AF, afib)
-
Atrial flutter
-
Atrial tachycardia (AT, atrial tach)
-
Monomorphic ventricular tachycardia with pulses
Internal cardioversion
Internal cardioversion for atrial fibrillation can be used in patients whose arrhythmia is resistant to external cardioversion or is inadvertently induced during an electrophysiologic study.
Contraindications
Cardioversion is contraindicated for any arrhythmia that is known to be incessant, as these rhythms recur immediately or soon after.
Contraindications also include known digitalis toxicity–associated tachycardia, sinus tachycardia caused by various clinical conditions, and multifocal atrial tachycardia.
In addition, because patients with atrial fibrillation (AF, afib) are at risk for developing blood clots in the left atrium, predisposing them to increased stroke risk, patients who are not anticoagulated should not undergo cardioversion without a transesophageal echocardiographic study that can assess the presence of a left atrial thrombus. Even patients with atrial fibrillation who are optimally anticoagulated with non-vitamin K antagonist oral anticoagulants (NOACs) have a low but not negligible risk for thrombus in the left atrial appendage. [9]
Synchronized cardioversion should also not be used to treat ventricular fibrillation, because the cardioverter may not sense a QRS wave and may therefore fail to deliver a shock. Synchronized cardioversion is also not appropriate for the treatment of pulseless ventricular tachycardia (VT, vtach) or polymorphic (irregular) VT, as these require high-energy, unsynchronized shocks (ie, defibrillation doses). In addition, cardioversion is not effective for the treatment of junctional tachycardia. [8]
Technique
External cardioversion
Advanced cardiac (cardiovascular) life support (ACLS) guidelines should be followed as indicated. The key components in preparing the patient are intravenous access as well as the close availability of airway management equipment, sedative drugs, and a cardioverter/defibrillator monitoring device. Note the following:
-
The patient should be adequately sedated with a short-acting agent such as midazolam or propofol. In addition, an opioid analgesic, such as fentanyl, is commonly used. Reversal agents, such as flumazenil and naloxone, should be available.
-
The defibrillator should be placed in the synchronized mode, which permits a search for a large R or S wave. The delivered energy is selected. Most monophasic and biphasic models can deliver up to 360 joules. Manual button depression by the operator causes the defibrillator to discharge an electric current that lasts less than 4 milliseconds and avoids the vulnerable period of cardiac repolarization when ventricular fibrillation (VF, vfib) can be induced. The operator should be aware of this brief delay as the cardioverter searches for a large positive or negative deflection. If the deflections are too small for the defibrillator to synchronize, the clinician can change the leads or place them closer to the patient's chest or heart. If the patient develops ventricular fibrillation, always turn off synchronization to avoid delay in energy delivery.
-
Two options exist for the placement of the paddles on the chest wall. First is the anterolateral position in which a single paddle is placed on the left fourth or fifth intercostal space on the midaxillary line; the other paddle is placed just to the right of the sternal edge on the second or third intercostal space.
-
The second option is the anteroposterior position. A single paddle is placed to the right of the sternum, as above, and the other paddle is placed between the tip of the left scapula and the spine. Conductive gel or pre-gelled pads are commonly used to ensure good contact, because the skin can conduct away a significant portion of the current. Even under ideal circumstances, only 10-30% of the total current reaches the heart.
-
The paddles should be placed firmly against the chest wall to avoid arcing and skin burns. Although there is a risk of receiving a shock if touching the patient or the stretcher, bed, or other equipment in which the patient is in contact, evidence exists showing that continued contact with the patient is safe during biphasic defibrillation. [10] Pacemakers and implantable cardioverter-defibrillators (ICDs) should be at least 10 cm away from direct contact with the paddles, and these devices should eventually be interrogated for any postcardioversion malfunction. The anteroposterior approach is preferred in patients with implantable devices to avoid shunting the current to the implantable device and damaging the system.
-
Energy requirements for atrial fibrillation (AF, afib) are 100-200 joules initially and 360 joules for subsequent shocks. A study showed good response to higher energy shocks of 720 joules for the treatment of refractory atrial fibrillation. [11] Biphasic shocks require a typical energy level of 75 joules for the correction of atrial fibrillation. Cardioversion of atrial fibrillation secondary to hyperthyroidism is 90% successful. [12] Only 25% of patients with atrial fibrillation caused by severe mitral regurgitation are successfully treated, and half revert in the first 6 months. Atrial flutter and paroxysmal supraventricular tachycardia (PSVT) require less energy: 50 joules initially, then 100 joules if needed. Cardioversion of ventricular tachycardia (VT, vtach) involves shocks of 50-100 joules initially, and then 200 joules if unsuccessful.
-
Either external paddles or stick-on electrode pads may be used to deliver the electric shocks.
-
Applying pressure to the pads using a rolled towel can improve cardioversion success by ensuring pad contact and minimizing skin burns.
-
In particularly difficult cases, two sets of pads and defibrillators can be used simultaneously to achieve synchronized cardioversion. [11]
Paddle/pad placement for the cardioversion of atrial fibrillation may vary, and the evidence suggests that placement is not a critical factor in the success of conversion. [13] However, anterolateral placement of the pads when conducting the initial shock appears to be more effective when utilizing biphasic defibrillators. In the event of postcardioversion bradycardia in which external pacing is required, non-apical pad placement may not capture the myocardium.
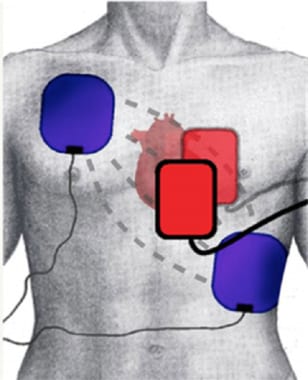 Common anatomic placements for the pads or paddles. The red pads represent the anteroposterior position. The blue pads represent the anterolateral position.
Common anatomic placements for the pads or paddles. The red pads represent the anteroposterior position. The blue pads represent the anterolateral position.
Internal cardioversion
The success of internal defibrillation with low-energy shocks to treat ventricular fibrillation and ventricular tachycardia resulted in further studies of internal cardioversion for the treatment of atrial fibrillation. Note the following:
-
The patient should receive anticoagulation as for external cardioversion, although anticoagulation should be withheld for safe venous puncture. Various techniques are available; the following is a commonly used procedure.
-
Three temporary catheters are inserted in the venous system and positioned under fluoroscopic guidance. Two catheters of large surface area are used for shock delivery, and a third quadripolar catheter is used for R-wave synchronization and temporary ventricular postshock pacing. The first defibrillation catheter is advanced into the distal coronary sinus; the second is positioned in the right atrium appendix or the lateral wall of the right atrium. These catheters are connected to an external defibrillator that delivers biphasic shocks. The quadripolar catheter is placed in the apex of the right ventricle and is also connected to an external pacemaker. In a study, right atrium-to-coronary sinus cardioversion vector was successfully used with mean energy of 5.6 ± 4.7 joules (0.4-35 joules). [14]
Treatment of a specific arrhythmia
Treatment strategies for atrial fibrillation include the following:
-
If the patient is clinically unstable, emergent cardioversion is recommended. Stable patients should have their ventricular rate controlled, and most should be anticoagulated with intravenous heparin and started on warfarin for stroke prevention because of a high risk of thromboembolism. If a high degree of certainty exists that atrial fibrillation is of less than 48 hours' duration, then a patient can proceed to cardioversion.
-
If the arrhythmia is of uncertain duration or of confirmed duration longer than 48 hours, then the patient can proceed to transesophageal echocardiography (TEE) for the evaluation of a thrombus in the atrium or appendage (a suggestion of smoke, or stagnant blood flow, is considered positive by some authorities). If the TEE findings are negative, the patient can proceed to elective cardioversion. Otherwise, these patients should be anticoagulated for 3 weeks before cardioversion with a repeat TEE.
-
All patients should be anticoagulated with warfarin for 4 weeks after cardioversion, because mechanical function of the atrium lags by up to 7 days after the restoration of sinus rhythm. If the foregoing treatment fails, patients can be managed with medical treatment alone, repeat cardioversion after antiarrhythmic (eg, ibutilide) treatment, ablation therapy, or atrial defibrillation. [15]
Treatment strategies for other supraventricular tachycardias (SVTs) include the following:
-
At present, recurrent atrial flutter is usually permanently cured by radiofrequency catheter ablation. If the patient is hemodynamically unstable, then cardioversion can be used.
-
Anticoagulation is recommended if external cardioversion is used in the treatment of atrial flutter, in a similar approach to patients with atrial fibrillation requiring cardioversion. Although atrial flutter was once perceived to be a lower risk for left atrial thrombus than atrial fibrillation, more recent data suggest that the risk of blood clot formation is equivalent.
-
Other patients with SVT rarely require external cardioversion unless they are hemodynamically unstable.
Treatment strategies for other ventricular tachycardias include the following:
-
Patients who do not respond to intravenous medications in treating stable monomorphic ventricular tachycardia associated with acute coronary syndrome or acute myocardial infarction should be initially treated with 50 to 100 joules of synchronized shocks. If no response to low-energy shock is noted, then a 200-joule shock should be administered, followed by 300- and 360-joule shocks as needed.
-
In unstable ventricular tachycardia, unsynchronized shocks should be delivered. Biphasic defibrillators do not require escalating energy, but three sequential shocks of 150 joules should be used.
Special conditions
In pediatric patients with PSVT or ventricular tachycardia who are not hemodynamically stable, an initial synchronized shock of 0.5 J/kg is recommended. In subsequent attempts, the energy is increased.
During pregnancy, recommendations as for other adults are applicable.
Complications
Complications of electrical cardioversion may affect patients or healthcare workers. For example, the injury incidence is an estimated 1 case per 1700 defibrillatory shocks for paramedics in the field and 1 per 1000 defibrillatory shocks for emergency medical technician-defibrillator personnel. [16] Patients may become hypoxic or hypoventilate from sedation. Most burns from shocks are superficial partial-thickness burns, but a few are deep.
Cardiac complications include severe bradycardia or asystole after cardioversion, which are more apt to occur after long-duration atrial fibrillation (AF, afib), use of high doses of beta or calcium blockers, and antiarrhythmic agents, as well as in elderly patients. Other complications include hypotension and pulmonary edema.
Inducible arrhythmias include bradycardia, atrioventricular (AV) block, asystole, ventricular tachycardia (VT, vtach), and ventricular fibrillation (VF, vfib). In patients with acute coronary syndromes or acute myocardial infarction, bradycardia or AV blocks can be induced, and they may need placement of an external or internal pacemaker. Ventricular tachycardia and ventricular fibrillation commonly occur in patients with prior similar history.
Postcardioversion ventricular fibrillation consists of two types. The first type occurs immediately after a shock and is related to improper synchronization. This type of ventricular fibrillation readily responds to defibrillation (unsynchronized countershock).
The second type of postcardioversion ventricular fibrillation is related to digitalis toxicity and manifests within a few minutes of cardioversion. Initially, it can be a junctional or paroxysmal atrial tachycardia, then ventricular fibrillation, which can be difficult to convert to a sinus rhythm.
Although some of the complications appear critical, direct current (DC) synchronized cardioversion is usually safe and effective if performed under the care of well-trained personnel. Troponin I measurements after cardioversion were not elevated in patients with normal and reduced left ventricular function, suggesting lack of myocyte injury. [17]
Questions & Answers
Overview
What is synchronized electrical cardioversion?
What are the basic principles in synchronized electrical cardioversion?
Which cardiac disorders are treated with synchronized electrical cardioversion?
What are the indications for use of external synchronized electrical cardioversion?
Which conditions are treated with external synchronized electrical cardioversion?
What are the indications for use of internal synchronized electrical cardioversion?
What are the contraindications for synchronized electrical cardioversion?
How is external synchronized electrical cardioversion administered?
What is the role of paddle placement in synchronized electrical cardioversion?
How is internal synchronized electrical cardioversion administered?
How is synchronized electrical cardioversion administered to pediatric patients?
How is synchronized electrical cardioversion administered to pregnant patients?
What are the possible complications of synchronized electrical cardioversion?
-
Three-dimensional electroanatomic map of type I atrial flutter. The colors progress from blue to red to white, representing relative conduction time in the right atrium (early to late). An ablation line (red dots) has been created on the tricuspid ridge extending to the inferior vena cava. This interrupts the flutter circuit. CSO = coronary sinus os, IVC = inferior vena cava, RAA = right atrial appendage, TV = tricuspid valve annulus.
-
Common anatomic placements for the pads or paddles. The red pads represent the anteroposterior position. The blue pads represent the anterolateral position.







