Nguyen Y, Guillevin L. Eosinophilic Granulomatosis with Polyangiitis (Churg-Strauss). Semin Respir Crit Care Med. 2018 Aug. 39 (4):471-481. [QxMD MEDLINE Link].
[Guideline] Groh M, Pagnoux C, Baldini C, Bel E, Bottero P, Cottin V, et al. Eosinophilic granulomatosis with polyangiitis (Churg-Strauss) (EGPA) Consensus Task Force recommendations for evaluation and management. Eur J Intern Med. 2015 Sep. 26 (7):545-53. [QxMD MEDLINE Link]. [Full Text].
Guillevin L, Cohen P, Gayraud M, et al. Churg-Strauss syndrome. Clinical study and long-term follow-up of 96 patients. Medicine (Baltimore). 1999 Jan. 78(1):26-37. [QxMD MEDLINE Link].
Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol. 1951 Mar-Apr. 27(2):277-301. [QxMD MEDLINE Link].
Churg A. Pulmonary angiitis and granulomatosis revisited. Hum Pathol. 1983 Oct. 14(10):868-83. [QxMD MEDLINE Link].
Keogh KA, Specks U. Churg-Strauss syndrome: clinical presentation, antineutrophil cytoplasmic antibodies, and leukotriene receptor antagonists. Am J Med. 2003 Sep. 115(4):284-90. [QxMD MEDLINE Link].
Masi AT, Hunder GG, Lie JT, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum. 1990 Aug. 33(8):1094-100. [QxMD MEDLINE Link].
Jennette JC, Falk RJ, Andrassy K, et al. Nomenclature of systemic vasculitides. Proposal of an international consensus conference. Arthritis Rheum. 1994 Feb. 37(2):187-92. [QxMD MEDLINE Link].
[Guideline] Grayson PC, Ponte C, Suppiah R, Robson JC, Craven A, Judge A, et al. 2022 American College of Rheumatology/European Alliance of Associations for Rheumatology Classification Criteria for Eosinophilic Granulomatosis with Polyangiitis. Ann Rheum Dis. 2022 Mar. 81 (3):309-314. [QxMD MEDLINE Link].
Cottin V, et al; Groupe d’Etudes et de Recherche sur les Maladies Orphelines Pulmonaires (GERM“O”P). Revisiting the systemic vasculitis in eosinophilic granulomatosis with polyangiitis (Churg-Strauss): A study of 157 patients by the Groupe d'Etudes et de Recherche sur les Maladies Orphelines Pulmonaires and the European Respiratory Society Taskforce on eosinophilic granulomatosis with polyangiitis (Churg-Strauss). Autoimmun Rev. 2017 Jan. 16 (1):1-9. [QxMD MEDLINE Link].
Hellmich B, Ehlers S, Csernok E, Gross WL. Update on the pathogenesis of Churg-Strauss syndrome. Clin Exp Rheumatol. 2003 Nov-Dec. 21(6 Suppl 32):S69-77. [QxMD MEDLINE Link].
Lyons PA, Peters JE, Alberici F, et al. Genome-wide association study of eosinophilic granulomatosis with polyangiitis reveals genomic loci stratified by ANCA status. Nat Commun. 2019 Nov 12. 10 (1):5120. [QxMD MEDLINE Link]. [Full Text].
Franco J, Artes MJ. Pulmonary eosinophilia associated with montelukast. Thorax. 1999 Jun. 54(6):558-60. [QxMD MEDLINE Link].
Wechsler ME, Finn D, Gunawardena D, et al. Churg-Strauss syndrome in patients receiving montelukast as treatment for asthma. Chest. 2000 Mar. 117(3):708-13. [QxMD MEDLINE Link].
Hauser T, Mahr A, Metzler C, Coste J, Sommerstein R, Gross WL, et al. The leucotriene receptor antagonist montelukast and the risk of Churg-Strauss syndrome: a case-crossover study. Thorax. 2008 Aug. 63(8):677-82. [QxMD MEDLINE Link].
Wechsler ME, Garpestad E, Flier SR, et al. Pulmonary infiltrates, eosinophilia, and cardiomyopathy following corticosteroid withdrawal in patients with asthma receiving zafirlukast. JAMA. 1998 Feb 11. 279(6):455-7. [QxMD MEDLINE Link].
Tuggey JM, Hosker HS. Churg-Strauss syndrome associated with montelukast therapy. Thorax. 2000 Sep. 55(9):805-6. [QxMD MEDLINE Link].
Vaglio A, Martorana D, Maggiore U, Grasselli C, Zanetti A, Pesci A, et al. HLA-DRB4 as a genetic risk factor for Churg-Strauss syndrome. Arthritis Rheum. 2007 Sep. 56(9):3159-66. [QxMD MEDLINE Link].
Chang HC, Chou PC, Lai CY, Tsai HH. Antineutrophil Cytoplasmic Antibodies and Organ-Specific Manifestations in Eosinophilic Granulomatosis with Polyangiitis: A Systematic Review and Meta-Analysis. J Allergy Clin Immunol Pract. 2021 Jan. 9 (1):445-452.e6. [QxMD MEDLINE Link].
Sinico RA, Sabadini E, Maresca AM. Mesalazine-induced Churg-Strauss syndrome in a patient with Crohn's disease and sclerosing cholangitis. Clin Exp Rheumatol. 2006 Mar-Apr. 24(2 Suppl 41):S104. [QxMD MEDLINE Link].
Orriols R, Munoz X, Ferrer J, Huget P, Morell F. Cocaine-induced Churg-Strauss vasculitis. Eur Respir J. 1996 Jan. 9(1):175-7. [QxMD MEDLINE Link].
Nappi E, De Santis M, Paoletti G, Pelaia C, Terenghi F, Pini D, et al. New Onset of Eosinophilic Granulomatosis with Polyangiitis Following mRNA-Based COVID-19 Vaccine. Vaccines (Basel). 2022 May 3. 10 (5):[QxMD MEDLINE Link]. [Full Text].
Eustace JA, Nadasdy T, Choi M. Disease of the month. The Churg Strauss Syndrome. J Am Soc Nephrol. 1999 Sep. 10(9):2048-55. [QxMD MEDLINE Link].
Boyer D, Vargas SO, Slattery D, Rivera-Sanchez YM, Colin AA. Churg-Strauss syndrome in children: a clinical and pathologic review. Pediatrics. 2006 Sep. 118(3):e914-20. [QxMD MEDLINE Link].
Keogh KA, Specks U. Churg-Strauss syndrome: update on clinical, laboratory and therapeutic aspects. Sarcoidosis Vasc Diffuse Lung Dis. 2006 Mar. 23(1):3-12. [QxMD MEDLINE Link].
Hasley PB, Follansbee WP, Coulehan JL. Cardiac manifestations of Churg-Strauss syndrome: report of a case and review of the literature. Am Heart J. 1990 Oct. 120(4):996-9. [QxMD MEDLINE Link].
Wechsler ME, Finn D, Gunawardena D, Westlake R, Barker A, Haranath SP, et al. Churg-Strauss syndrome in patients receiving montelukast as treatment for asthma. Chest. 2000 Mar. 117(3):708-13. [QxMD MEDLINE Link].
Sokolowska BM, Szczeklik WK, Wludarczyk AA, Kuczia PP, Jakiela BA, Gasior JA, et al. ANCA-positive and ANCA-negative phenotypes of eosinophilic granulomatosis with polyangiitis (EGPA): outcome and long-term follow-up of 50 patients from a single Polish center. Clin Exp Rheumatol. 2014 May-Jun. 32(3 Suppl 82):S41-7. [QxMD MEDLINE Link].
Sablé-Fourtassou R, Cohen P, Mahr A, Pagnoux C, Mouthon L, Jayne D, et al. Antineutrophil cytoplasmic antibodies and the Churg-Strauss syndrome. Ann Intern Med. 2005 Nov 1. 143(9):632-8. [QxMD MEDLINE Link].
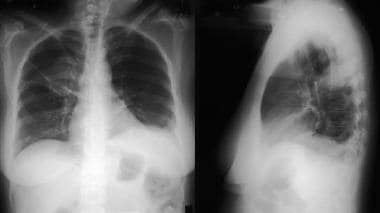
Choi YH, Im JG, Han BK, Kim JH, Lee KY, Myoung NH. Thoracic manifestation of Churg-Strauss syndrome: radiologic and clinical findings. Chest. 2000 Jan. 117(1):117-24. [QxMD MEDLINE Link].
Kim Y, Lee KS, Choi DC, et al. The spectrum of eosinophilic lung disease: radiologic findings. J Comput Assist Tomogr. 1997 Nov-Dec. 21(6):920-30. [QxMD MEDLINE Link].
Buschman DL, Waldron JA Jr, King TE Jr. Churg-Strauss pulmonary vasculitis. High-resolution computed tomography scanning and pathologic findings. Am Rev Respir Dis. 1990 Aug. 142(2):458-61. [QxMD MEDLINE Link].
Worthy SA, Müller NL, Hansell DM, Flower CD. Churg-Strauss syndrome: the spectrum of pulmonary CT findings in 17 patients. AJR Am J Roentgenol. 1998 Feb. 170(2):297-300. [QxMD MEDLINE Link].
Mavrogeni S, Karabela G, Gialafos E, Stavropoulos E, Spiliotis G, Katsifis G, et al. Cardiac involvement in ANCA (+) and ANCA (-) Churg-Strauss syndrome evaluated by cardiovascular magnetic resonance. Inflamm Allergy Drug Targets. 2013 Oct. 12(5):322-7. [QxMD MEDLINE Link].
Lie JT. Histopathologic specificity of systemic vasculitis. Rheum Dis Clin North Am. 1995 Nov. 21(4):883-909. [QxMD MEDLINE Link].
Katzenstein AL. Diagnostic features and differential diagnosis of Churg-Strauss syndrome in the lung. A review. Am J Clin Pathol. 2000 Nov. 114(5):767-72. [QxMD MEDLINE Link].
Chemmalakuzhy AJ, Zhou XJ, Hedayati SS. ANCA-negative glomerulonephritis associated with nonasthmatic Churg-Strauss syndrome. Nat Clin Pract Nephrol. 2008 Oct. 4(10):568-74. [QxMD MEDLINE Link].
Lhote F, Cohen P, Guilpain P, Guillevin L. [Churg-Strauss syndrome]. Rev Prat. 2008 Jun 15. 58(11):1165-74. [QxMD MEDLINE Link].
Hervier B, Durant C, Masseau A, Ponge T, Hamidou M, Mussini JM. Use of muscle biopsies for diagnosis of systemic vasculitides. J Rheumatol. 2011 Mar. 38(3):470-4. [QxMD MEDLINE Link].
Ford JA, Aleatany Y, Gewurz-Singer O. Therapeutic advances in eosinophilic granulomatosis with polyangiitis. Curr Opin Rheumatol. 2022 May 1. 34 (3):158-164. [QxMD MEDLINE Link].
Mukhtyar C, Flossmann O, Hellmich B, Bacon P, Cid M, Cohen-Tervaert JW, et al. Outcomes from studies of antineutrophil cytoplasm antibody associated vasculitis: a systematic review by the European League Against Rheumatism systemic vasculitis task force. Ann Rheum Dis. 2008 Jul. 67(7):1004-10. [QxMD MEDLINE Link].
Mohammad AJ, Hot A, Arndt F, Moosig F, Guerry MJ, Amudala N, et al. Rituximab for the treatment of eosinophilic granulomatosis with polyangiitis (Churg-Strauss). Ann Rheum Dis. 2016 Feb. 75 (2):396-401. [QxMD MEDLINE Link].
Kitching AR, Anders HJ, Basu N, Brouwer E, Gordon J, Jayne DR, et al. ANCA-associated vasculitis. Nat Rev Dis Primers. 2020 Aug 27. 6 (1):71. [QxMD MEDLINE Link]. [Full Text].
Jachiet M, Samson M, Cottin V, Kahn JE, Le Guenno G, et al. Anti-IgE monoclonal antibody (omalizumab) in refractory and relapsing eosinophilic granulomatosis with polyangiitis (Churg-Strauss): Data from 17 patients. Arthritis Rheumatol. 2016 Mar 4. [QxMD MEDLINE Link].
Tiliakos A 4th, Shaia S, Hostoffer R, Kent L. The use of infliximab in a patient with steroid-dependent churg-strauss syndrome. J Clin Rheumatol. 2004 Apr. 10(2):96-7. [QxMD MEDLINE Link].
Casian A, Jayne D. Plasma exchange in the treatment of Wegener's granulomatosis, microscopic polyangiitis, Churg-Strauss syndrome and renal limited vasculitis. Curr Opin Rheumatol. 2011 Jan. 23(1):12-7. [QxMD MEDLINE Link].
Guillevin L, Cevallos R, Durand-Gasselin B, et al. Treatment of glomerulonephritis in microscopic polyangiitis and Churg-Strauss syndrome. Indications of plasma exchanges, Meta-analysis of 2 randomized studies on 140 patients, 32 with glomerulonephritis. Ann Med Interne (Paris). 1997. 148(3):198-204. [QxMD MEDLINE Link].
Bonaci-Nikolic B, Nikolic MM, Andrejevic S, Zoric S, Bukilica M. Antineutrophil cytoplasmic antibody (ANCA)-associated autoimmune diseases induced by antithyroid drugs: comparison with idiopathic ANCA vasculitides. Arthritis Res Ther. 2005. 7(5):R1072-81. [QxMD MEDLINE Link].
Wechsler ME, Akuthota P, Jayne D, Khoury P, Klion A, Langford CA, et al. Mepolizumab or Placebo for Eosinophilic Granulomatosis with Polyangiitis. N Engl J Med. 2017 May 18. 376 (20):1921-1932. [QxMD MEDLINE Link].
Koga Y, Aoki-Saito H, Kamide Y, Sato M, Tsurumaki H, Yatomi M, et al. Perspectives on the Efficacy of Benralizumab for Treatment of Eosinophilic Granulomatosis With Polyangiitis. Front Pharmacol. 2022. 13:865318. [QxMD MEDLINE Link]. [Full Text].
Espinoza LR. Combination therapy to treat churg-strauss syndrome: corticosteroids with short- or long-term cyclophosphamide pulses. Curr Rheumatol Rep. 2008 Dec. 10(6):427-9. [QxMD MEDLINE Link].
Yamasaki A, Tomita K, Fujii Y, Hasegawa Y, Watanabe M, Sano H, et al. Repressed ileal artery aneurysms in Churg-Strauss syndrome following combination treatment with glucocorticoid and cyclophosphamide. Rheumatol Int. 2008 Aug 8. [QxMD MEDLINE Link].
Ribi C, Cohen P, Pagnoux C, Mahr A, Arène JP, Lauque D, et al. Treatment of Churg-Strauss syndrome without poor-prognosis factors: a multicenter, prospective, randomized, open-label study of seventy-two patients. Arthritis Rheum. 2008 Feb. 58(2):586-94. [QxMD MEDLINE Link].
Tatsis E, Schnabel A, Gross WL. Interferon-alpha treatment of four patients with the Churg-Strauss syndrome. Ann Intern Med. 1998 Sep 1. 129(5):370-4. [QxMD MEDLINE Link].
Metzler C, Schnabel A, Gross WL, Hellmich B. A phase II study of interferon-alpha for the treatment of refractory Churg-Strauss syndrome. Clin Exp Rheumatol. 2008 May-Jun. 26(3 Suppl 49):S35-40. [QxMD MEDLINE Link].
Cohen P, Guillevin L, Baril L, et al. Persistence of antineutrophil cytoplasmic antibodies (ANCA) in asymptomatic patients with systemic polyarteritis nodosa or Churg-Strauss syndrome: follow-up of 53 patients. Clin Exp Rheumatol. 1995 Mar-Apr. 13(2):193-8. [QxMD MEDLINE Link].
[Guideline] Chung SA, Langford CA, Maz M, et al. 2021 American College of Rheumatology/Vasculitis Foundation Guideline for the Management of Antineutrophil Cytoplasmic Antibody-Associated Vasculitis. Arthritis Care Res (Hoboken). 2021 Aug. 73 (8):1088-1105. [QxMD MEDLINE Link]. [Full Text].
Beasley R, Bibby S, Weatherall M. Leukotriene receptor antagonist therapy and Churg-Strauss syndrome: culprit or innocent bystander?. Thorax. 2008 Oct. 63(10):847-9. [QxMD MEDLINE Link].
Giavina-Bianchi P, Giavina-Bianchi M, Agondi R, Kalil J. Three months' administration of anti-IgE to a patient with Churg-Strauss syndrome. J Allergy Clin Immunol. 2007 May. 119(5):1279; author reply 1279-80. [QxMD MEDLINE Link].
Green RL, Vayonis AG. Churg-Strauss syndrome after zafirlukast in two patients not receiving systemic steroid treatment. Lancet. 1999 Feb 27. 353(9154):725-6. [QxMD MEDLINE Link].
Guillevin L, Lhote F, Gayraud M, et al. Prognostic factors in polyarteritis nodosa and Churg-Strauss syndrome. A prospective study in 342 patients. Medicine (Baltimore). 1996 Jan. 75(1):17-28. [QxMD MEDLINE Link].
Kaushik VV, Reddy HV, Bucknall RC. Successful use of rituximab in a patient with recalcitrant Churg-Strauss syndrome. Ann Rheum Dis. 2006 Aug. 65(8):1116-7. [QxMD MEDLINE Link].
Kümpers P, Erdbrügger U, Grossheim M, Meyer GP, Hiss M, Gwinner W, et al. Endothelial microparticles as a diagnostic aid in Churg-Strauss vasculitis-induced cardiomyopathy. Clin Exp Rheumatol. 2008 May-Jun. 26(3 Suppl 49):S86-9. [QxMD MEDLINE Link].
Lie JT. Illustrated histopathologic classification criteria for selected vasculitis syndromes. American College of Rheumatology Subcommittee on Classification of Vasculitis. Arthritis Rheum. 1990 Aug. 33(8):1074-87. [QxMD MEDLINE Link].
Pabst S, Tiyerili V, Grohé C. Apparent response to anti-IgE therapy in two patients with refractory "forme fruste" of Churg-Strauss syndrome. Thorax. 2008 Aug. 63(8):747-8. [QxMD MEDLINE Link].
Roccatello D, Baldovino S, Alpa M, Rossi D, Napoli F, Naretto C, et al. Effects of anti-CD20 monoclonal antibody as a rescue treatment for ANCA-associated idiopathic systemic vasculitis with or without overt renal involvement. Clin Exp Rheumatol. 2008 May-Jun. 26(3 Suppl 49):S67-71. [QxMD MEDLINE Link].
Todd DC, Cockcroft DW. Prolonged survival in Churg-Strauss syndrome. Ann Allergy Asthma Immunol. 2004 Jan. 92(1):92-3. [QxMD MEDLINE Link].
Greco A, Rizzo MI, De Virgilio A, Gallo A, Fusconi M, Ruoppolo G, et al. Churg-Strauss syndrome. Autoimmun Rev. 2015 Apr. 14 (4):341-8. [QxMD MEDLINE Link].
Wechsler ME, Akuthota P, Jayne D, Khoury P, Klion A, Langford CA, et al. Mepolizumab or Placebo for Eosinophilic Granulomatosis with Polyangiitis. N Engl J Med. 2017 May 18. 376 (20):1921-1932. [QxMD MEDLINE Link].
Wechsler ME, Akuthota P, Jayne D, Khoury P, Klion A, Langford CA, et al. Mepolizumab or Placebo for Eosinophilic Granulomatosis with Polyangiitis. N Engl J Med. 2017 May 18. 376 (20):1921-1932. [QxMD MEDLINE Link]. [Full Text].
Canzian A, et al; French Vasculitis Study Group and the European EGPA Study Group. Use of Biologics to Treat Relapsing and/or Refractory Eosinophilic Granulomatosis With Polyangiitis: Data From a European Collaborative Study. Arthritis Rheumatol. 2021 Mar. 73 (3):498-503. [QxMD MEDLINE Link].