Practice Essentials
Hypertriglyceridemia, a condition in which triglyceride levels are elevated, is a common disorder in the United States. It is often caused or exacerbated by uncontrolled diabetes mellitus, obesity, and sedentary habits, all of which are more prevalent in industrialized societies than in developing nations. In epidemiologic and interventional studies, hypertriglyceridemia is a risk factor for coronary artery disease (CAD). Elevated triglycerides are determined by direct laboratory analysis of serum or plasma after a 10- to 12-hour fast. Determining which lipoprotein abnormality is the cause of hypertriglyceridemia is less straightforward.
Triglycerides are fats consisting of 3 fatty acids covalently bonded to a glycerol molecule. These fats are synthesized by the liver or, in the case of those derived from dietary sources, are ingested by the liver; the triglycerides are subsequently transported throughout the circulation by triglyceride-rich lipoproteins.
Hyperlipoproteinemia is a metabolic disorder characterized by abnormally elevated concentrations of specific lipoprotein particles in the plasma.
Hyperlipidemia (ie, elevated plasma cholesterol or triglyceride levels or both) is present in all hyperlipoproteinemias. The primary form includes chylomicronemia, hypercholesterolemia, dysbetalipoproteinemia, hypertriglyceridemia, mixed hyperlipoproteinemia, and combined hyperlipoproteinemia. Other diseases, such as diabetes mellitus, pancreatitis, renal disease, and hypothyroidism, cause the secondary form. [1]
Signs and symptoms of hypertriglyceridemia
Hypertriglyceridemia is usually asymptomatic until triglycerides are greater than 1000-2000 mg/dL. Signs and symptoms may include the following:
-
GI: Pain in the mid-epigastric, chest, or back regions; nausea, vomiting
-
Respiratory: Dyspnea
-
Dermatologic: Xanthomas
-
Ophthalmologic: Corneal arcus, xanthelasmas
See Clinical Presentation for more detail.
Workup in hypertriglyceridemia
On examination, findings may be normal, or they may include the following:
-
GI: Tenderness to palpation over mid-epigastric or upper right/left quadrants; hepatomegaly
-
Cardiovascular: Decreased pedal pulses or ankle/brachial index in presence of peripheral vascular disease
-
Ophthalmologic: Corneal arcus, lipemia retinalis, xanthelasmas [2]
-
Neurologic: Memory loss, dementia, and depression in the presence of chylomicronemia syndrome
Testing
Laboratory studies used to evaluate hypertriglyceridemia include the following:
-
Lipid analysis
-
Chylomicron determination
-
Fasting blood glucose level
-
TSH level
-
Urinalysis
-
Liver function studies
Procedures
If the diagnosis of eruptive xanthomas is in doubt, obtaining a biopsy of the suspicious lesions will reveal accumulations of fat (not cholesterol). A biopsy of cutaneous lesions suspected to be either planar or tuberous xanthomas will reveal cholesterol deposition.
See Workup for more detail.
Fredrickson classification
Hyperlipidemia has been defined by the Fredrickson classification, which is based on beta-quantification, a process involving ultracentrifugation followed by electrophoresis. [3] In this system, shown in Table 1, below, all categories except type IIa are forms of hypertriglyceridemia.
Table 1. Fredrickson Classification of Hyperlipidemia (Open Table in a new window)
Type |
Serum Elevation |
Lipoprotein Elevation |
I |
Cholesterol and triglycerides |
Chylomicrons |
IIa |
Cholesterol |
LDL |
IIb |
Cholesterol and triglycerides |
LDL, VLDL |
III |
Cholesterol and triglycerides |
IDL |
IV |
Triglycerides |
VLDL |
V |
Cholesterol and triglycerides |
VLDL, chylomicrons |
IDL = intermediate-density lipoprotein; LDL = low-density lipoprotein; VLDL = very low-density lipoprotein. Source: Fredrickson DS, Lees RS. A system for phenotyping hyperlipidaemia. Circulation. Mar 1965;31:321-7. [3] |
||
Type I is a rare disorder characterized by severe elevations in chylomicrons and extremely elevated triglycerides, always reaching well above 1000 mg/dL and not infrequently rising as high as 10,000 mg/dL or more. It is caused by mutations of either the lipoprotein lipase gene (LPL), which is critical for the metabolism of chylomicrons and very low-density lipoprotein (VLDL), or the gene's cofactor, apolipoprotein (apo) C-II.
Counterintuitively, despite exceedingly high elevations of triglyceride and, in some cases, of total cholesterol, these mutations do not appear to confer an increased risk of atherosclerotic disease. This fact may have contributed to the unfounded belief that hypertriglyceridemia is not a risk factor for atherosclerotic disease. Although chylomicrons contain far less cholesterol than other triglyceride-rich lipoproteins do, when serum triglyceride levels are severely elevated, cholesterol levels can also be quite high.
Type IIb is the classic mixed hyperlipidemia (high cholesterol and triglyceride levels), caused by elevations in low-density lipoprotein (LDL) and VLDL.
Type III is known as dysbetalipoproteinemia, remnant removal disease, or broad-beta disease due to an individual’s decreased ability to convert VLDL and intermediate-density lipoprotein (IDL), a VLDL remnant, to LDL particles in the blood and because of a decreased clearance of chylomicron remnants. [4] Typically, patients with this rare condition have elevated total cholesterol (range, 300 600 mg/dL) and triglyceride levels (usually >400 mg/dL; may exceed 1000 mg/dL), [3] and these individuals are easily confused with patients with type IIb hyperlipidemia. Patients with type III hyperlipidemia have elevations in IDL.
Dysbetalipoproteinemia is the result of 2 "hits." [4] First, most affected individuals are homozygous for the apo E isoform, apo E2. Second, affected individuals usually have a metabolic disorder such as diabetes, obesity, or hypothyroidism. Consequently, those who are homozygous for apo E2 have a 1-2% risk of developing dysbetalipoproteinemia, and they are at high risk for atherosclerotic cardiovascular and peripheral vascular disease. [4] The condition responds well to treatment of the causative medical condition and to lipid-lowering medications.
Type IV is characterized by abnormal elevations of VLDL, and triglyceride levels are almost always less than 1000 mg/dL. Serum cholesterol levels are normal.
Type V is characterized by elevations of chylomicrons and VLDL. Triglyceride levels are invariably greater than 1000 mg/dL, and total cholesterol levels are always elevated. The LDL cholesterol level is usually low. Given the rarity of type I disease, when triglyceride levels above 1000 mg/dL are noted, the most likely cause is type V hyperlipidemia.
Triglyceride levels greater than 1000 mg/dL increase the risk of acute pancreatitis, and because triglycerides are so labile, levels of 500 mg/dL or greater must be the primary focus of therapy. If a patient also has a high risk for a cardiovascular event, LDL-lowering therapy should be considered.
Management of hypertriglyceridemia
Nonpharmacotherapeutic management
Nonpharmacologic management of hypertriglyceridemia is generally the initial treatment for patients with this condition. This primarily involves lifestyle modifications such as diet, exercise, weight reduction, smoking cessation, and limiting alcohol intake.
Pharmacotherapy
Medications used in the management of hypertriglyceridemia include the following:
-
Fibric acid derivatives (eg, gemfibrozil, fenofibrate)
-
Niacin (slow-release, immediate-release, extended-release formulations)
-
Omega-3 fatty acids (eg, icosapent, omega-3-acid ethyl esters)
-
HMG-CoA reductase inhibitors (eg, atorvastatin, fluvastatin, pitavastatin, pravastatin, lovastatin, simvastatin, rosuvastatin)
Surgical option
In general, surgical intervention is not necessary to treat hypertriglyceridemia. Plasmapheresis can be used in the setting of severe hypertriglyceridemia to reduce triglycerides in the acute setting. Ileal bypass surgery has been shown to improve all lipid parameters but should be reserved for severe hypertriglyceridemia refractory to all treatment.
See Treatment and Medication for more detail.
Pathophysiology
Triglycerides
Triglycerides are fats consisting of 3 fatty acids covalently bonded to a glycerol molecule. These fats are synthesized by the liver or, in the case of those derived from dietary sources, are ingested by the liver (as described below); the triglycerides are subsequently transported throughout the circulation by triglyceride-rich lipoproteins.
By dry weight, triglycerides make up approximately 86%, 55%, and 23% of chylomicrons, very low-density lipoproteins (VLDLs), and intermediate-density lipoproteins (IDLs), respectively, [5] as represented in the image below. Triglycerides are present in low-density lipoprotein (LDL) and high-density lipoprotein (HDL), but in much smaller quantities of 10% or less.
The following image shows composition of triglyceride-rich proteins.
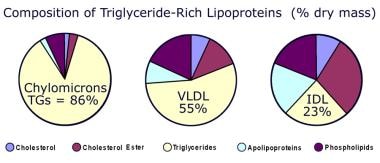 Composition of triglyceride (TG)-rich lipoproteins. IDL = intermediate-density lipoprotein; VLDL = very low-density lipoprotein.
Composition of triglyceride (TG)-rich lipoproteins. IDL = intermediate-density lipoprotein; VLDL = very low-density lipoprotein.
Triglyceride-rich lipoproteins come from 2 sources, often described as the endogenous and exogenous pathways. In the exogenous pathway, dietary fats (triglycerides) are hydrolyzed to free fatty acids (FFAs) and monoglycerides and are absorbed, with cholesterol, by intestinal cells. They are then reesterified and combined with apolipoproteins and phospholipids to form a nascent chylomicron, a process requiring microsomal triglyceride transfer protein (MTP). The initial apolipoproteins are apolipoprotein (apo) A, which are soluble and can transfer to HDL; and apo B48, a structural apolipoprotein that is not removed during catabolism of the chylomicron. Chylomicrons enter the plasma via the thoracic duct, where they acquire other soluble apolipoproteins, including apo CI, apo CII, apo CIII, and apo E, from HDL.
VLDLs and apolipoproteins
VLDLs are produced by a process analogous to the exogenous pathway. Triglycerides may derive from de novo FFA synthesis in the liver and are metabolized by lipoprotein lipase to IDL, also called VLDL remnants. Lipoprotein lipase hydrolyzes triglycerides, releasing FFAs, which are taken up by myocytes and hepatocytes. Some apo Cs, phospholipids, and apo Es are lost, and triglycerides are transferred to HDL in exchange for cholesterol esters. IDL is, thus, cholesterol-enriched and triglyceride-poor compared to unmetabolized VLDL. As IDL is metabolized by hepatic lipase to LDL, the remaining surface apolipoproteins are lost. [6, 4, 7]
Triglycerides may also derive from the uptake of remnant chylomicrons, VLDL, or FFAs from the plasma. Precursor VLDL combines triglycerides, the structural or transmembrane apo B100, and phospholipids, as well as cholesterol and some apo Cs and Es. The formation of the immature VLDL requires microsomal transfer protein (MTP). Once secreted into the plasma, VLDLs acquire more apo Cs and Es.
Apo Es
ApoEs are ligands that have greater affinity for the LDL receptor than does apo B100. In fact, the LDL receptor is more accurately designated the B/E receptor. Apo E also binds with high affinity to the LDL receptor-related protein, which takes up chylomicron remnants, VLDL, and IDL. In addition, apo E binds to cell-surface heparan sulfate proteoglycans (HSPGs), which assists in the hepatic uptake of remnant lipoproteins. [4]
The apo E gene has been cloned, sequenced, and mapped to chromosome 19. Genetically altered apo E–deficient mice develop severe dyslipidemia with accelerated atherosclerosis, whereas transgenic mice overexpressing apo E appear to be protected from atherosclerosis. [8, 9] Apo E has 3 isoforms that are present in slightly varying proportions, depending on race and geographic location. [6] Apo E3 is the most prevalent allele and for that reason was considered the “wild type” allele from which apo E2 and apo E4 were derived. Newer data, however, suggest that apoA4 was the earliest form of the protein. [10]
Most animals, including primates, possess an apo E4 equivalent. [11] Compared with apo E3, apo E2 has less affinity for the receptor, and apo E4 has more. The alleles differ in 2 amino acid positions, 112 and 158. Apo E2 is most commonly caused by cysteine substituted for arginine at position 158 in apo E3. In apo E4, an arginine is substituted for cysteine at position 112 in apo E3. The substitutions are recessive in that dysbetalipoproteinemia requires the presence of 2 apo E-2 isoforms. [11] Other very rare genetic variants of apo E exist, and several of these have been shown to have defective binding to the LDL receptor and LDL receptor-like protein. These variants act in a dominant fashion in that only 1 copy of apo E is necessary for susceptibility to development of type III hyperlipidemia.
Approximately 1% of individuals in White populations are homozygous for apo E2 (“first hit”); however, only 10% of these homozygotes will develop the condition. A “second hit” is necessary, most commonly metabolic abnormalities that cause increases in VLDL. [4] Other, less common genetic conditions can also predispose people to dysbetalipoproteinemia.
More than 90% of patients with dysbetalipoproteinemia are homozygous for apo E2; the remainder have a rare, usually dominant, defect in apo E2. In addition to the apoE2 homology or defect, and combined with a metabolic condition, other genetic factors have been suggested that increase the likelihood of developing dysbetalipoproteinemia. Polymorphisms in the apo A5, lipoprotein lipase and apo C3 have all been mentioned as possible cofactors for the condition. [6]
Accumulation of IDL is caused by the poor affinity of apo E2 to LDL receptors, whereas LDL uptake via apo B100 is unaffected. In fact, total cholesterol, LDL cholesterol, and apo B are usually low compared with those with apo E3. HDL cholesterol levels may be normal or decreased. The following 3 mechanisms have been postulated for the hypocholesterolemic effect of apo E2 [12] :
-
Increased upregulation of LDL receptors due to decreased binding of lipoproteins containing apo E2
-
Increased hepatic LDL uptake due to lower LDL receptor affinity of apo E2 and consequent decreased competition with the apo B100 born by LDL (its sole apolipoprotein)
-
Apo E2 interference with lipolysis of VLDL to LDL [4]
Chylomicron and VLDL metabolism
Any disturbance that causes increased synthesis of chylomicrons and/or VLDLs or decreased metabolic breakdown causes elevations in triglyceride levels. That disturbance may be as common as dietary indiscretion or as unusual as a genetic mutation of an enzyme in the lipid metabolism pathway. Essentially, hypertriglyceridemia occurs through 1 of the following 3 processes [13] :
-
Abnormalities in hepatic VLDL production, and intestinal chylomicron synthesis
-
Dysfunctional lipoprotein lipase -mediated lipolysis
-
Impaired remnant clearance
As shown in the images below, chylomicrons and VLDLs are initially metabolized by lipoprotein lipase, which hydrolyzes the triglycerides, releasing FFAs; these FFAs are stored in fat and muscle. With normal lipoprotein lipase activity, the half-lives of chylomicrons and VLDLs are about 10 minutes and 9 hours, respectively. Because of the large size of unmetabolized chylomicrons, they are unlikely to be taken up by macrophages, which are the precursors of foam cells. Foam cells promote fatty streak formation, the precursor of atherosclerotic plaque. Lipoprotein lipase activity produces chylomicron remnants that are small enough to take part in the atherosclerotic process. Chylomicron remnants are taken up by the LDL receptor or the LDL receptor-related protein. [14]
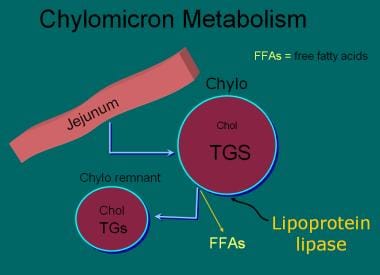 Lipoprotein lipase (LPL) releases free fatty acids (FFAs) from chylomicrons (chylo) and produces chylomicron remnants that are small enough to take part in the atherosclerotic process. Chol = cholesterol; TGs, TGS = triglycerides.
Lipoprotein lipase (LPL) releases free fatty acids (FFAs) from chylomicrons (chylo) and produces chylomicron remnants that are small enough to take part in the atherosclerotic process. Chol = cholesterol; TGs, TGS = triglycerides.
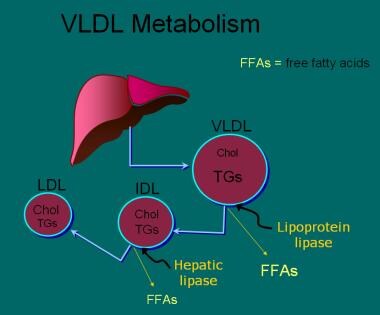 Once very low-density lipoprotein (VLDL) has been metabolized by lipoprotein lipase, VLDL remnants in the form of intermediate-density lipoprotein (IDL) can be metabolized by hepatic lipase, producing low-density lipoprotein (LDL), or they can be taken up by the LDL receptor via either apolipoprotein B (apo B) or apo E. Chol = cholesterol; TGs = triglycerides.
Once very low-density lipoprotein (VLDL) has been metabolized by lipoprotein lipase, VLDL remnants in the form of intermediate-density lipoprotein (IDL) can be metabolized by hepatic lipase, producing low-density lipoprotein (LDL), or they can be taken up by the LDL receptor via either apolipoprotein B (apo B) or apo E. Chol = cholesterol; TGs = triglycerides.
VLDL remnants have 1 of 2 fates: they can be metabolized by hepatic lipase, which further depletes triglycerides, producing LDL, or they can be taken up by the LDL receptor via either apo B or apo E. VLDL remnants are not only triglyceride-poor, they are also cholesterol enriched, having acquired cholesterol ester from HDL via the action of cholesterol ester transfer protein (CETP), which facilitates the exchange of VLDL triglycerides for cholesterol in HDL. This pathway may promote HDL's reverse cholesterol transport activity, but only if VLDL and LDL return cholesterol to the liver. If these lipoproteins are taken up by macrophages, the CETP transfer results in increased atherogenesis.
Chylomicron remnants, VLDL, VLDL remnants, and LDL are all atherogenic.
Etiology
Hypertriglyceridemia has many causes, including familial and genetic syndromes, metabolic disease, and drugs. [15, 16] Risks appear to include diet, stress, physical inactivity, and smoking.
CHD risk factors
The National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) identifies the 2 or more of the following as risk factors for coronary heart disease (CHD) that can lead to the need for more aggressive intervention [14] :
-
Older age: In men, age 45 years or older, whereas in women, 55 years or older; the incidence of CHD is higher in the elderly than the young and in men more than women of the same age
-
Family history of premature CHD: Paternal or male primary relative with myocardial infarction (MI) before age 55 years or sudden death, or in maternal or female primary relative before age 65 years
-
Active tobacco use
-
Hypertension: Blood pressure higher than 140/90 mm Hg or current use of antihypertensive agents
-
Low level of high-density lipoprotein (HDL) cholesterol: Lower than 40 mg/dL
Genetic causes
Abnormalities of the enzyme pathway for chylomicron metabolism are the best-characterized genetic causes of hypertriglyceridemia. Lipoprotein lipase deficiency and apo C-II deficiency are caused by homozygous autosomal recessive genes present at conception.
Type I hyperlipoproteinemia is the best-characterized genetic cause of hypertriglyceridemia and is caused by a deficiency or defect in either the enzyme lipoprotein lipase or its cofactor, apo C-II. Lipoprotein lipase hydrolyzes triglycerides in chylomicrons and very low-density lipoprotein (VLDL), releasing free fatty acids. The enzyme is found in the endothelial cells of capillaries and can be released into the plasma by heparin. Lipoprotein lipase is essential for the metabolism of chylomicrons and VLDL, transforming them into their respective remnants. Apo C-II, an apolipoprotein present in both chylomicrons and VLDL, acts as a cofactor in the action of lipoprotein lipase.
The above pathway is affected by other genetic disorders, particularly type 1 or type 2 diabetes, because lipoprotein lipase requires insulin for full activity. That is, a secondary cause of hyperlipidemia, “second hit,” must be present for the dysbetalipoproteinemia to develop. In addition, the patient may be taking medications, such as protease inhibitors or tricyclic antidepressants, that exacerbate hyperlipidemia.
Two more recently described syndromes include mutations in ApoAV leading to a truncated ApoAV devoid of a lipid-binding domain and glycosylphosphatidylinositol-anchored HDL-binding protein 1 (GP1HBP1) causing decreased binding to LPL and reduced hydrolysis of chylomicrons. [17]
Genetic predisposition for dysbetalipoproteinemia is present in approximately 1% of the population, but only 1-2% of individuals with apolipoprotein (apo) E-2 actually develop this condition. More than 90% of patients with dysbetalipoproteinemia are homozygous for apo E2. Extremely rare forms are associated with other genetic mutations in the apo E gene or the complete absence of apo E.
Familial combined hyperlipidemia and familial hypertriglyceridemia
Two triglyceride disorders, familial combined hyperlipidemia and familial hypertriglyceridemia, are genetically controlled, but the mechanisms are not clearly defined but are likely associated with overproduction and decreased of apo B–containing particles.
Familial combined hyperlipidemia is an autosomal dominant disorder characterized by patients and their first-degree relatives who may have either isolated triglyceride or low-density lipoprotein (LDL) cholesterol elevations or both. Diagnosis of the disorder in a particular patient requires a family history of premature coronary artery disease (CAD) in 1 or more first-degree relatives and a family history for elevated triglycerides with or without elevated LDL cholesterol levels. The diagnosis is important for prognosis; 14% of patients with premature CAD have familial combined hyperlipidemia. [18]
Familial hypertriglyceridemia is also an autosomal dominant trait. [19] These patients and their families have isolated triglyceride elevations and may have an increased risk of premature CAD.
Genetic susceptibility factor effects
Known genetic susceptibility factor effects account for approximately 10-15% of the trait variances in blood lipid levels (LDL cholesterol, HDL cholesterol, triglycerides). [20] Genome-wide association studies (GWAS) have identified several loci associated with blood lipid traits, including hypertriglyceridemia. [21]
Hypertriglyceridemia is associated with several genes (in aggregate) including apoAV, GCKR, LPL, and APOB. [22] Patients with single nucleotide polymorphisms (SNPs) 40 kilobases (kb) from TRIB1 (a gene known to be strongly associated with dyslipidemia) have abnormal levels of triglycerides, as well as HDL cholesterol and LDL cholesterol. [23] In a large study of Japanese and Korean individuals, investigators reported that genetic variants of APOA5 (-1131T→C polymorphism [rs662799]) and BTN2A1 (C→T polymorphism [rs6929846]) synergistically affect the prevalence of dyslipidemia in East Asian populations and metabolic syndrome in Japanese individuals. [24]
Certain genetic variants can further predispose a patient with hypertriglyceridemia and certain environmental factors to consequences, such as CAD and MI. For example, the genetic variant R952QP of LRP8 (a gene at 1p31-32 that is associated with familial and premature CAD as well as high-level platelet activation) is associated with high triglyceride levels in patients who are have a history of being overweight, smoke, and have premature CAD/MI. [25]
Metabolic causes
Uncontrolled diabetes mellitus, both type 1 and type 2, is one of the most common causes of hypertriglyceridemia, and it is often severe in patients presenting with ketosis. Patients with type 1 diabetes mellitus are insulin deficient, and lipoprotein lipase is largely ineffective. Control of these patients' diabetes mellitus with insulin will restore lipoprotein lipase function, reducing triglyceride levels and restoring diabetes mellitus control.
In patients with uncontrolled type 2 diabetes mellitus and hyperinsulinemia, triglycerides are elevated for several reasons, including the following:
-
Lipoprotein lipase is less effective in the insulin-resistant state
-
Overproduction of VLDL by the liver is common in patients with diabetes who are often overweight
-
Diabetes mellitus is one of the conditions that leads to incomplete metabolism of VLDL, causing increased remnant VLDL or IDL observed in dysbetalipoproteinemia (see Dysbetalipoproteinemia).
Mild to moderate elevations in triglycerides are common in obese patients, largely secondary to reduced efficacy of LPL and overproduction of VLDL.
Hypothyroidism commonly causes LDL cholesterol elevations, but it also may lead to mixed hyperlipidemia or isolated triglyceride elevations. Reduced hepatic lipase activity slows VLDL remnant catabolism. As with diabetes mellitus, untreated hypothyroidism may cause dysbetalipoproteinemia in patients with homozygous apo E-2.
Nephrotic syndrome is thought to increase hepatic synthesis of VLDL and may also slow catabolism of both LDL and VLDL. As in hypothyroidism, elevated LDL cholesterol levels are more common in this condition, but mixed hyperlipidemia or isolated triglyceride elevations may be observed. Higher levels of proteinuria are correlated with more severe hyperlipidemia.
Drugs
Medications that can cause hypertriglyceridemia include the following:
-
High-dose thiazide diuretics or chlorthalidone
-
High-dose beta-adrenergic blocking agents, excluding those with intrinsic sympathomimetic activity
-
Unopposed oral estrogen replacement therapy
-
Oral contraceptives with high estrogen content
-
Tamoxifen
-
Glucocorticoids
-
Oral isotretinoin
-
Antiretroviral therapy (including some protease inhibitors, nonnucleoside reverse transcriptase inhibitors)
-
Atypical antipsychotics
Other causes
Excessive alcohol intake and high-carbohydrate diets (>60% of caloric intake) are frequent causes of hypertriglyceridemia.
Acute pancreatitis may cause substantial elevations in triglycerides by unknown mechanisms. However, much more frequently, severe hypertriglyceridemia causes acute pancreatitis. In patients presenting with acute pancreatitis and triglycerides greater than 1000 mg/dL, it is prudent to not assume that the triglycerides are the cause of the pancreatitis. Other causes, such as common bile duct obstruction and alcoholism, must be considered as possible etiologies.
Nonetheless, a study by Sanchez et al found the rate of acute pancreatitis in persons with triglyceride levels of over 1000 mg/dL to be 1.21%, compared with 0.08% in those with levels below 200 mg/dL. [26]
A study by Zhang et al indicated that obesity and uric acid elevation have a strong additive interaction that increases the risk for nonalcoholic fatty liver disease and hypertriglyceridemia. The interaction was reportedly responsible for 27% and 26% of the expanded hypertriglyceridemia risk in men and women, respectively. [27]
In pregnant patients with a history of mildly to moderately elevated triglycerides in the nonpregnant state, hypertriglyceridemia (sometimes severe) may occur. Such patients should be monitored closely, particularly in the third trimester. In fact, simply looking for laboratory notation of lipemic serum in routine blood tests during pregnancy will avoid unexpected complications resulting from unrecognized and untreated hypertriglyceridemia during pregnancy.
Epidemiology
United States statistics
The National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) defined elevated triglycerides as 150 mg/dL and higher. [14] Using that criterion, the Third National Health and Nutrition Examination Survey (NHANES) found that the prevalence of hypertriglyceridemia in US adults aged 20 years and older was approximately 35% in men and 25% in women. Triglyceride levels in Black men and women were 21% and 14%, respectively; 40% and 35% in Mexican American men and women, respectively; and in 37% and 25% in White American men and women, respectively. [28]
In Black individuals, the frequency of the alleles for apolipoprotein (apo) E2 is 12%; apo E3, 65%; and apoE4, 23%; in the White population, the frequencies are approximately 13%; 76%; and 11%, respectively. [11] The frequency of homology for apo E2 is 1.3%, but because of the necessary "second hit," only about 5% of homologous individuals have overt hyperlipidemia. [11]
Prevalence of severe hypertriglyceridemia, defined as triglycerides greater than 2000 mg/dL, is estimated to be to be 1.8 cases per 10,000 White adults, with a higher prevalence in patients with diabetes or alcoholism. [14] The most severe form of hypertriglyceridemia, lipoprotein lipase deficiency, occurs in approximately 1 case per 1 million; the frequency of apo C-II deficiency is even lower. The frequency of dysbetalipoproteinemia is less than 5 persons per 5,000 in the overall population. [11]
International statistics
Hyperlipoproteinemia has a high frequency in developed countries. The worldwide incidence of lipoprotein lipase deficiency is similar to that in the United States with the exception of small populations—such as in Quebec, Canada, where the number is significantly higher, probably due to the founder effect. Apo C-II deficiency is infrequent in all populations studied to date.
Globally, the frequency of all 3 major apoE alleles varies by racial group. The incidence of the apo E2 allele, however, is always far lower than that of the apo E3 allele. Frequencies as low as 4.1% and 4.6% were found in Finland and in Singhalese of Indian descent, respectively. [11] In addition to the US, the highest frequencies were found in New Zealand (12.0%) and in Malaysian Singhalese (11.4%). Frequencies in other populations ranged from 6.1% (Iceland) to 9.7 (Chinese Singhalese). [11]
Race-, sex-, and age-related demographics
As noted above, although the frequency of apo E2 varies somewhat by race, the prevalence of dysbetalipoproteinemia appears to be similar among races. The racial differences are a consequence not only of apo E2 frequency but also of the prevalence of the metabolic abnormalities necessary to cause dysbetalipoproteinemia.
Nonhispanic Blacks often have lower triglyceride levels, possibly related to an increase in LPL activity. [29] Racial predisposition has not been described for lipoprotein lipase deficiency or apo CII deficiency.
In the Prospective Cardiovascular Munster study (PROCAM), a large observational study, mild hypertriglyceridemia (triglycerides >200 mg/dL) was more prevalent in men (18.6%) than in women (4.2%). [30] Genetic mutations in both lipoprotein lipase and apo CII affect males and females in equal numbers.
Dysbetalipoproteinemia primarily affects older adults and is rare in children and premenopausal women. However, in the United States and some other Western populations, the increasing incidence of childhood obesity and type 2 diabetes may presage the emergence of dysbetalipoproteinemia in children. Estrogen improves the clearance of very low-density lipoprotein (VLDL) remnants, and estrogen treatment appears to improve dysbetalipoproteinemia in some postmenopausal women.
Triglycerides increase gradually in men until about age 50 years and then decline slightly. In women, they continue to increase with age. Mild hypertriglyceridemia (triglycerides >150 mg/dL) is slightly more prevalent in men beginning at age 30 years and women starting at age 60 years. [17, 28]
The manifestations of lipoprotein lipase and apo C-II deficiency (severe hypertriglyceridemia) are usually detected in childhood, although defective apo C-II sometimes presents in early adulthood.
Prognosis
Patients with hyperlipidemia are at extremely high risk of developing premature coronary artery disease (CAD) (30%). [31] If the disease is inadequately managed, the prognosis is poor, especially if other cardiovascular risk factors are present. If the patient complies with lipid-lowering therapy, dietary modification, and lifestyle modification and if therapy is successful, outcome is improved significantly.
Cardiovascular disease
Hypertriglyceridemia is correlated with an increased risk of cardiovascular disease (CVD), particularly in the setting of low high-density lipoprotein (HDL) cholesterol levels and/or elevated low-density lipoprotein (LDL) cholesterol levels. When low HDL cholesterol levels are controlled for, some studies demonstrate that elevated triglycerides do not correlate with risk of CVD. Others suggest that high triglyceride levels are an independent risk factor.
Because metabolism of the triglyceride-rich lipoproteins (chylomicrons, very low-density lipoprotein [VLDL]) and metabolism of HDL are interdependent and because triglycerides are very labile, the independent impact of hypertriglyceridemia on CVD risk is difficult to confirm. However, randomized clinical trials using triglyceride-lowering medications have demonstrated decreased coronary events in both the primary and secondary coronary prevention populations.
A study by Saadatagah et al supported the idea that elevated triglyceride levels contribute to the development of coronary heart disease (CHD). The investigators found that at 11.3-year follow-up, adults with primary isolated hypertriglyceridemia had a rate of incident coronary heart disease events of 18.9%, compared with 11.8% in controls. [32]
An understanding of lipoprotein catabolism provides an explanation for the absence of increased risk of CVD in patients with the most severe form of hypertriglyceridemia, type I hyperlipoproteinemia. The atherogenicity correlated with elevated triglyceride levels is thought to be secondary to increased levels of chylomicron and VLDL remnants. Remnants are smaller, richer in cholesterol, and more readily taken up by macrophages, which are converted to plaque-forming foam cells. The chylomicrons in patients with type I disease cannot be converted to remnants and, therefore, should not be atherogenic.
Using data from the National Health and Nutrition Examination Survey (2007-2014), Fan et al estimated that in adult statin users with triglyceride levels in the range between greater than 150 and 500 mg/dL, the mean 10-year risk of atherosclerotic cardiovascular disease is 11.3-19.1%, while in non–statin users falling within the same parameters, the mean 10-year risk is 6.0-15.6%. [33]
Pancreatitis
Extreme elevations of triglycerides, usually well above 1000 mg/dL, may cause acute pancreatitis and all the sequelae of that condition. (A study by Pedersen et al indicated that even nonfasting mild to moderate hypertriglyceridemia [177 mg/dL or above] raises the risk for acute pancreatitis; the investigators found, for example, the multivariable adjusted hazard ratio for acute pancreatitis to be 2.3 for persons with triglyceride levels of 177-265 mg/dL. [34] ) However, many patients tolerate triglycerides of 4000 mg/dL or higher without developing symptoms. [35]
The National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III) guidelines indicate that triglycerides are so labile that a level between 500 and 1000 mg/dL may in certain settings increase dramatically and should be a target of treatment even before ensuring that the LDL goal is reached. [14] Thus, these guidelines stipulate that if triglycerides are 500 mg/dL or greater, the initial management should be to lower the triglycerides to prevent pancreatitis. Only when the triglyceride level is below 500 should LDL-lowering be addressed.
The risk of recurrent pancreatitis secondary to hypertriglyceridemia can be avoided entirely by ensuring that levels are maintained well below 700 mg/dL. Because triglyceride levels are so labile, simply moderating levels to less than 1000 mg/dL does not decrease risk substantially, because the slightest metabolic imbalance or dietary indiscretion may push levels several hundred points higher.
Chylomicronemia syndrome
The chylomicronemia syndrome [36, 37] is an often unrecognized and less severe condition than pancreatitis that is usually caused by triglyceride levels greater than 1000 mg/dL. Recurrent episodes of ill-defined abdominal pain that may be accompanied by nausea and vomiting are the most common presenting symptom, but chest pain and dyspnea may sometimes occur. A papular rash may be present on the trunk, thighs, and buttocks, which resolves with treatment. Amylase and lipase are minimally, if at all, elevated. Symptoms resolve when triglyceride levels decrease well below 1000 mg/dL.
Patient Education
Patients often do not understand that triglycerides are a blood lipid that may be analyzed along with cholesterol. They should be informed about the risks of hypertriglyceridemia, including the increased risk of a cardiovascular event and risk of pancreatitis if levels are close to or above 1000 mg/dL.
Patients should be informed that triglycerides respond to the simple interventions of diet control, exercise, and appropriate weight loss. A trained dietitian should provide thorough diet instructions. Exercise counseling or monitoring may be helpful to treat the dyslipidemia and reduce the risk of symptomatic cardiovascular disease.
In addition, the provider should stress the importance of alcohol intake of no more than 1 drink per day, provide instructions on the use of medications, and provide comprehensive diabetes education to diabetic patients.
For patient education resources, Medscape Reference’s Cholesterol Center and Heart Health Center, as well as High Cholesterol, Understanding Your Cholesterol level, Lifestyle Cholesterol Management, Understanding Cholesterol-Lowering Medications, and Statins and Cholesterol.
-
Eruptive xanthomas on the back of a patient admitted with a triglyceride level of 4600 mg/dL and acute pancreatitis.
-
Close-up of eruptive xanthomas.
-
Composition of triglyceride (TG)-rich lipoproteins. IDL = intermediate-density lipoprotein; VLDL = very low-density lipoprotein.
-
Lipoprotein lipase (LPL) releases free fatty acids (FFAs) from chylomicrons (chylo) and produces chylomicron remnants that are small enough to take part in the atherosclerotic process. Chol = cholesterol; TGs, TGS = triglycerides.
-
Once very low-density lipoprotein (VLDL) has been metabolized by lipoprotein lipase, VLDL remnants in the form of intermediate-density lipoprotein (IDL) can be metabolized by hepatic lipase, producing low-density lipoprotein (LDL), or they can be taken up by the LDL receptor via either apolipoprotein B (apo B) or apo E. Chol = cholesterol; TGs = triglycerides.







