Practice Essentials
A brain tumor is one of the most devastating forms of human illness, especially when occurring in the posterior fossa. Brainstem compression, herniation, and death are all risks in tumors that occur in this critical location. Tumors in the posterior fossa are considered critical brain lesions, primarily because of the limited space within the posterior fossa and the potential involvement of vital brain stem nuclei. The clinical presentation depends on the site of the tumor, biological behavior and aggressiveness of the tumor, and the rate of growth. At the time of presentation, the patient may be very ill from severe headache or frequent vomiting due to associated hydrocephalus. Symptoms may be caused by focal compression of the cerebellum or brain stem centers and increased intracranial pressure. [1, 2, 3, 4]
No specific causes of posterior fossa tumors exist; however, genetic factors,such as dysfunction of some tumor suppressor genes (p53 gene) and activation of some oncogenes may play a role in their development. [1] Environmental factors such as irradiation and toxins may also play a role.
Cushing probably was the first to report a large series of posterior fossa tumors. He published information about 61 patients with cerebellar medulloblastoma with mostly fatal outcomes. [5]
Advances in brain surgery for tumors were primarily due to discovery of anesthesia, asepsis, neurologic localization, and the ability to achieve hemostasis. Hippocrates, who likely performed it for headache, epilepsy, fractures, and blindness, first described trephination.
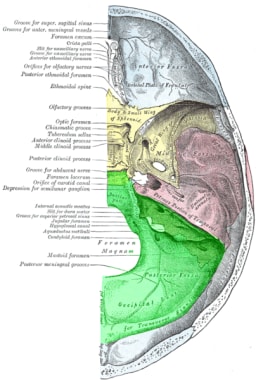
(An image of the posterior fossa anatomy is shown below.)
Posterior fossa tumors are more common in children than in adults. Central nervous system tumors are the most common solid tumors in children; between 54 and 70% of all childhood brain tumors originate in the posterior fossa. [6] About 15-20% of brain tumors in adults occur in the posterior fossa.
Progress in pediatric treatment for posterior fossa tumor has improved survival rates; however, most survivors present neurocognitive sequelae that impact academic achievement. Memory deficits are a core feature in survivors of pediatric posterior fossa tumor, especially when treatment requires radiotherapy. To limit these effects, dose constraints for specific brain areas involved in memory should be defined. During long-term follow-up, specific attention must be paid to identify these deficits and thereby limit their impact on quality of life. [7]
Posterior fossa tumors are very rare in infants, and information on this is scarce in the literature. In children younger than 1 year, posterior fossa tumors represent a unique challenge. Infants with high-grade tumors display the worst outcomes and the lowest survival, indicating that more effective strategies are needed. [8]
Certain types of posterior fossa tumors, such as medulloblastoma, pineoblastoma, ependymomas, primitive neuroectodermal tumors (PNETs), and astrocytomas of the cerebellum and brain stem, occur more frequently in children. Some glial tumors, such as mixed gliomas, are unique to children; they are located more frequently in the cerebellum (67%) and are usually benign.
Hydrocephalus is common in children with posterior fossa tumors, occurring in 71-90% of pediatric patients; approximately 10-40% demonstrate persistent hydrocephalus after posterior fossa tumor resection. [9, 10, 11, 12]
Hydrocephalus associated with posterior fossa tumors affects the quality of life of patients. Routine preoperative cerebrospinal fluid diversion is not necessary for most patients with posterior fossa tumor–related hydrocephalus. A high index of suspicion and aggressive surveillance are required for early identification and appropriate management of postresection hydrocephalus. Future studies are needed to address unanswered questions pertaining to the management of this condition. [13]
Patients older than 3 years are considered at standard risk or high risk and have long-term survival rates of approximately 85% and 70%, respectively. In patients 3 years or younger, survival rates are generally lower. [14]
Patients who present with posterior fossa tumors undergo surgery for the following goals [2, 15, 16, 17, 18, 19] :
-
To decompress the posterior fossa for the purpose of relieving pressure on the brain stem and/or to release intracranial pressure and avert the risk of herniation.
-
To diagnose the tumor based on histopathology.
-
To determine further plan of management depending on the nature of the tumor.
CT scan of the posterior fossa is inferior to MRI in diagnostic value because of the artifact produced from the surrounding thick bone. However, CT scan is helpful for postoperative follow-up. Cerebral angiography is useful to assess the vascular supply of the tumor, but with the wide availability of MRI, cerebral angiography is no longer used as the first option in brain tumor assessment.
Some patients should undergo an emergency operation, especially if they present with acute symptoms of brain stem involvement or herniation. [9, 10, 19, 21]
(See the images below.)
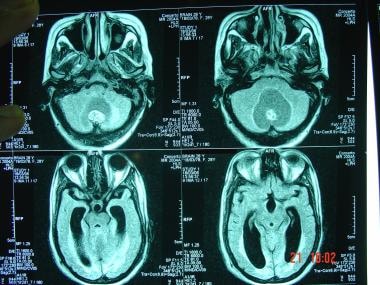 A 28-year-old female patient presented with headache, ataxia, and blurring of vision. A T1-weighted MRI image, sagittal view, shows dilatation of the lateral ventricles.
A 28-year-old female patient presented with headache, ataxia, and blurring of vision. A T1-weighted MRI image, sagittal view, shows dilatation of the lateral ventricles.
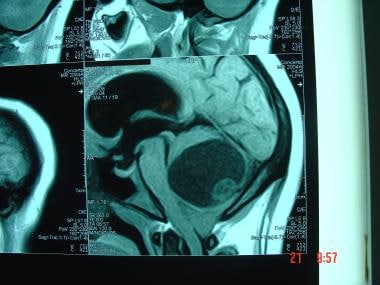 A 28-year-old female patient presented with headache, ataxia, and blurring of vision. A T1-weighted MRI image, sagittal view, shows an infratentorial mass with a large cystic component and small nodule. The mass is compressing the brainstem.
A 28-year-old female patient presented with headache, ataxia, and blurring of vision. A T1-weighted MRI image, sagittal view, shows an infratentorial mass with a large cystic component and small nodule. The mass is compressing the brainstem.
Performing a lumbar puncture in patients with suspected posterior fossa tumors is contraindicated. A risk of central herniation exists even with a very small amount of CSF drainage. To avoid this catastrophe, a thorough clinical examination, including funduscopy and a CT scan of the brain, should be performed before lumbar puncture.
Pathophysiology
Cerebellar astrocytoma
Cystic cerebellar astrocytoma constitute about 33% of all posterior fossa tumors in children. It represents 25% of all pediatric tumors. Average age at presentation is 9 years. Typically, cerebellar astrocytoma presents as a laterally located cyst with a well-defined solid component. The tumor may be solid or cystic and may be located medially in the vermis or laterally in the cerebellar hemisphere.
Primary neuroectodermal tumors
Primitive neuroectodermal tumors (PNETs) include medulloblastomas, medulloepitheliomas, pigmented medulloblastomas, ependymoblastomas, pineoblastomas, and cerebral neuroblastomas. These tumors originate from undifferentiated cells in the subependymal region in the fetal brain. PNETs are second to the cerebellar astrocytoma in frequency, constituting 25% of intracranial tumors in children.
Medulloblastoma
Medulloblastoma (MB) is a malignant embryonal tumor of the posterior fossa belonging to the family of PNETs. MB generally occurs during pediatric age, but in 14-30% of cases, it affects adults, most of whom are younger than 40 years, with an incidence of 0.6 cases per million per year, representing about 0.4-1% of tumors of the nervous system in adults. Current MB treatments for older patients are largely drawn from the pediatric experience, but the transferability and applicability of these treatments to adults remain an open question. [22]
Medulloblastoma initially arises in the inferior medullary velum and grow to fill the fourth ventricle, infiltrating the surrounding structures. Some erroneously thought it arose from medulloblast cells, which do not exist. It is better included in the family of PNETs. [23]
Ependymoma and ependymoblastoma
Ependymomas are rare central nervous system tumors. The current treatment strategy is gross total tumor removal. Adjuvant stereotactic radiosurgery after tumor removal might be considered if radiotherapy is not an option. The role of chemotherapy is unclear, and use of chemotherapy should be tailored to individual patients. [24]
Ependymomas are derived from ependymal cells. They occur more frequently in females, with 50% presenting in children younger than 3 years. An ependymoma has a much better prognosis than an anaplastic ependymoma (ependymoblastoma). Plastic ependymoma can mold itself to the available spaces inside or outside the ventricle without adhering to the ventricle.
Choroid plexus papilloma and carcinoma
Choroid plexus papilloma and carcinoma represent 0.4-0.6% of all intracranial tumors. They are more frequent in children than in adults (3% of childhood brain tumors). Sixty percent occur in the lateral ventricle and 30% in the fourth ventricle. The third ventricle and cerebellopontine angle are rare locations for this tumor. Cerebrospinal fluid (CSF) overproduction may occur, sometimes reaching more than 4 times normal volumes. In most cases, CSF analysis demonstrates increased protein, xanthochromia, or both.
Dermoid tumors
Dermoid tumors arise from incomplete separation of epithelial ectoderm from neuroectoderm at the region of the anterior neuropore; this usually occurs during the fourth week of gestation. The cyst wall often includes hair follicles, sweat glands, and sebaceous glands. The cyst grows slowly, and it gradually becomes filled by desquamated epithelium, sweat, and sebaceous materials. Aseptic meningitis is a sequela of cyst rupture. More commonly, the cyst occurs in the posterior fossa, at or near the midline. It may be extradural, vermian, or intraventricular. A dermal sinus may be connected to the mass. It may be detected clinically or by MRI.
Hemangioblastoma
Hemangioblastoma represents about 7-12% of all posterior fossa tumors. About 70% of hemangioblastomas occurring in the cerebellum are cystic. Age of presentation is 30-40 years old. Hemangioblastomas are more common in males. Hemangioblastoma may be associated with von Hippel-Lindau disease. [25]
Metastatic tumors
Three percent of all cranial metastatic lesions occur in the brainstem, and 18% occur in the cerebellum. Originating sites include breast, lung, skin, and kidney. Solitary metastasis is better treated by surgical removal before radiation therapy. Surgery also should be considered in case of radiosensitive original tumors or when the primary source is unknown.
Brainstem gliomas
Brainstem gliomas constitute 15% of all brain tumors. In children, brainstem glioma represents 25-30% of all brain tumors. Most brainstem gliomas are low-grade astrocytoma.
Relevant Anatomy
The posterior cranial fossa is the deepest and most capacious of the 3 cranial fossae. It contains the cerebellum, pons, and medulla oblongata. The foramen magnum is located centrally and inferiorly in the posterior fossa. The posterior fossa is surrounded by deep grooves containing the transverse sinuses and sigmoid sinuses.
The brainstem is the portion of the brain connecting the cerebral hemispheres with the spinal cord. It contains the midbrain, pons, and medulla oblongata. The brainstem is partially obscured by the cerebral hemispheres and cerebellum. The gray matter in the brainstem is scattered into numerous small masses called nuclei, many of which are motor or sensory nuclei of the cranial nerves.
The midbrain is the portion of the brain that connects the pons and the cerebral hemispheres. The dorsal segment of the midbrain is called the tectum; the more central and ventral portion is called the tegmentum.
The pons lies anterior to the cerebellum and superior to the medulla, from which it is separated by a groove through which the abducens, facial, and acoustic nerves emerge.
The medulla oblongata is the pyramid-shaped segment of brainstem between the spinal cord and pons. The lower half contains the remnants of the central canal; the posterior portion of the superior half forms the floor of the body of the fourth ventricle.
The cerebellum is located in the posterior fossa of the skull, dorsal to the pons and medulla. It is separated from the overlying cerebrum by an extension of dura mater, the tentorium cerebelli. It is oval in form, with its widest diameter along the transverse axis. It is composed of a small, unpaired central portion (the vermis) and 2 large lateral masses (the cerebellar hemispheres).
Prognosis
The 5-year survival rates exceed 60% for all patients and 80% for certain good-risk individuals with posterior fossa tumors. In cases of pilocytic cerebellar astrocytoma, the 25-year survival rate exceeds 94%.
Patients with medulloblastoma are classified into good-risk and bad-risk categories based on the following:
-
Age of presentation
-
Extension of surgical resection
-
Leptomeningeal dissemination or metastasis
Prognosis in medulloblastoma is worse for children younger than 2 years, for patients with subtotal resection (80%), and for those with subarachnoid metastasis or positive results on CSF cytology more than 2 weeks after surgery. In patients with ependymomas, the 5-year survival rate is 20%; in ependymoblastoma, the 5-year survival rate is only 6%.
Choroid plexus papilloma has excellent prognosis, as high as 100% survival rate. Choroid plexus carcinoma has a poor prognosis.
-
Posterior fossa anatomy.
-
A 28-year-old female patient presented with headache, ataxia, and blurring of vision. A T1-weighted MRI image, sagittal view, shows an infratentorial mass with a large cystic component and small nodule. The mass is compressing the brainstem.
-
A 28-year-old female patient presented with headache, ataxia, and blurring of vision. A T1-weighted MRI image, sagittal view, shows dilatation of the lateral ventricles.
-
The tumor (the infratentorial mass) after excision shows its vascular nature (see previous images).