Practice Essentials
An epidural hematoma (EDH) is an extra-axial collection of blood within the potential space between the outer layer of the dura mater and the inner table of the skull. It is confined by the lateral sutures (especially the coronal sutures) where the dura inserts. It is a life-threatening condition that may require immediate intervention and can be associated with significant morbidity and mortality if left untreated. Rapid diagnosis and evacuation are important for a good outcome. [1]
Epidural hematoma can develop following intrathecal puncture, spinal vascular malformation, or spontaneous hemorrhage. Prompt recognition of symptoms and referral to neurosurgical services are crucial for recovery. [2] The outcome for EDH is more favorable than decades ago, most probably reflecting a well-established chain of trauma care. Therefore, EDH is a treatable disease with a high probability of a favorable outcome. [3]
Trauma is the typical cause of EDH. A majority of cases related to a traumatic mechanism result from head injury due to motor vehicle collisions, physical assaults, or accidental falls. Nontraumatic mechanisms include infection/abscess, coagulopathy, hemorrhagic tumor, and vascular malformation. [1] Dystocia, forceps delivery, and excessive skull moulding through the birth canal have been implicated in EDH in newborns. [4]
Epidural hematoma is an easily treated form of head injury that is often associated with a good prognosis. In rare instances, such hemorrhages can be spontaneous. Spontaneous spinal epidural hematoma (SSEH) is a rare but potentially devastating condition if not appropriately identified and managed. A few case series regarding SSEH have described certain risk factors; however, much continues to be unknown regarding its pathophysiology and optimal management. [5]
Patients with EDH who meet surgical criteria and receive prompt surgical intervention can have an excellent prognosis when underlying primary brain damage from the traumatic event is limited. [6] A retrospective review of 58 patients surgically treated for acute EDH revealed that age and Glasgow Coma Scale score (GCS) are useful predictors of prognosis and can guide clinicians in making a prompt diagnosis. [7]
Epidural hematoma is a relatively common presentation to the emergency department. The condition is best managed by an interprofessional team that includes the emergency room physician, trauma team, radiologist, neurologist, neurosurgeon, intensivist, and intensive care unit nurses. [1]
The priority for the emergency physician is to stabilize the patient and check the ABCs (airway, breathing, circulation). This should be done urgently. Epidural hematoma is a neurosurgical emergency that requires urgent surgical evacuation to prevent irreversible neurologic injury and death secondary to hematoma expansion and herniation. Neurosurgical consultation should be urgently obtained, as it is important to intervene within 1 to 2 hours of presentation. [1]
Epidural hematoma has been associated with mortality rates in excess of 15%. The key prognostic feature is the level of consciousness at the time of presentation. [1] In general, preoperative motor examination, GCS score, and pupillary reactivity are significantly correlated with functional outcomes. Because many isolated EDHs do not involve underlying structural brain damage, the overall outcome is excellent if prompt surgical evacuation is undertaken.
The key to treating EDH is preventing it in the first place. Healthcare workers should educate the public on the importance of head safety equipment when playing sports or while working. [1]
Etiology
Epidural hematoma results from interruption of dural vessels, including branches of the middle meningeal arteries, veins, dural venous sinuses, and skull vessels. Continued bleeding and growth can result in elevation of intracranial pressure, which may be detected in a clinical setting by observing ipsilateral pupil dilation (secondary to uncal herniation and oculomotor nerve compression), as well as elevated blood pressure, slowed heart rate, and irregular breathing. This triad is known as the “Cushing reflex.” These findings may indicate the need for immediate intracranial intervention to prevent central nervous system depression and death. [1]
(An image depicting epidural hemorrhage is shown below.)
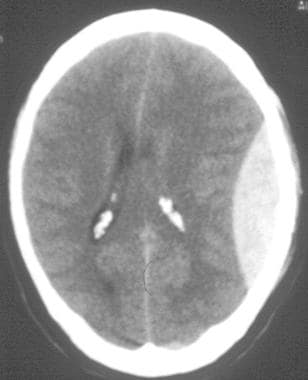 CT scan of an acute left-sided epidural hematoma. Note the typical convex or lens-shaped appearance. The hematoma takes this shape as the dura strips from the undersurface of the cranium, limited by the suture lines. A midline shift of the ventricular system is present. This hemorrhage requires immediate surgical evacuation.
CT scan of an acute left-sided epidural hematoma. Note the typical convex or lens-shaped appearance. The hematoma takes this shape as the dura strips from the undersurface of the cranium, limited by the suture lines. A midline shift of the ventricular system is present. This hemorrhage requires immediate surgical evacuation.
Pathophysiology
Epidural hematoma is mainly caused by structural disruption of the dural and skull vessels commonly associated with calvarial fractures. Laceration of the middle meningeal artery and its accompanying dural sinuses is the most common etiology.
Unlike subdural hematoma, cerebral contusion, or diffuse axonal injury of the brain, EDH is not generated secondary to head motion or acceleration.
In the posterior fossa, disruption of dural venous sinuses (eg, transverse sinus, sigmoid sinus) by fracture may lead to EDH. Disruption of the superior sagittal sinus may cause vertex EDH. Other nonarterial sources of epidural hemorrhage include venous lakes, diploic veins, arachnoid granulations, and the petrosal sinuses.
Anterior temporal tip epidural hematomas have been postulated to form because of disruption of the sphenoparietal sinus. [8]
Posterior fossa epidural hemorrhage can mimic a sinus thrombus by compressing and displacing the sinuses. It is important to recognize this possibility because treatment of a suspected thrombus with anticoagulation can worsen epidural hemorrhage. [9]
A small number of epidural hematomas have been reported in the absence of trauma. Etiologies include infectious disease of the skull, vascular malformation of the dura mater, and metastasis to the skull.
Spontaneous EDH can also occur in patients with coagulopathies associated with other primary medical problems (eg, end-stage liver disease, chronic alcoholism, other disease states associated with dysfunctional platelets).
Epidemiology
As many as 2% of all head-injured patients and 15% of those with fatal head injuries are estimated to have EDH; incidence is proportionate to age in the pediatric population. Approximately 17% of previously conscious patients who deteriorate into coma following a trauma have EDH. [10]
Males are more often affected than females. Furthermore, the incidence is higher among adolescents and young adults. The mean age of affected patients is 20 to 30 years, and EDH is rare after 50 to 60 years of age. As an individual's age advances, the dura mater becomes more adherent to the overlying bone. This decreases the chance that a hematoma can develop in the space between the cranium and the dura. [1]
Relevant Anatomy
Below the skull bone lies the dura mater, which overlies the leptomeningeal structures, the arachnoid, and the pia mater, which, in turn, overlie the brain. The dura mater consists of 2 layers; the outer layer serves as a periosteal layer for the inner surface of the skull.
As a person ages, the dura becomes more adherent to the skull, reducing the frequency of EDH formation. In infancy, the skull is more pliable and is less likely to fracture. Epidural hematoma can form when the dura is stripped from the skull during impact.
The dura is most adherent to the sutures that connect various bones of the skull. Major sutures include coronal sutures (frontal and parietal bones), sagittal sutures (both parietal bones), and lambdoid sutures (parietal and occipital bones). Epidural hematoma rarely extends beyond the sutures.
The region most commonly involved with EDH is the temporal region (70-80%). In the temporal region, the bone is relatively thin and the middle meningeal artery is close to the inner table of the skull. The incidence of EDH in the temporal region is lower among pediatric patients because the middle meningeal artery has not yet formed a groove within the inner table of the skull. [11] Epidural hematoma occurs in frontal, occipital, and posterior fossa regions with approximately equal frequency. It occurs less frequently in the vertex and in parasagittal areas.
An anatomic study found that the middle meningeal artery is accompanied by 2 dural sinuses that are situated along each side of the vessel. [12] Laceration of this artery is likely to cause a mixture of arterial and venous bleeding.
Prognosis
Factors that may influence outcomes of patients with EDS include the following:
-
Patient age
-
Time lapsed between injury and treatment
-
Immediate coma or lucid interval
-
Presence of pupillary abnormalities
-
GCS/motor score, on arrival
-
CT findings (ie, hematoma volume, degree of midline shift, signs of active hematoma bleeding, associated intradural lesions) [1]
-
CT scan of an acute left-sided epidural hematoma. Note the typical convex or lens-shaped appearance. The hematoma takes this shape as the dura strips from the undersurface of the cranium, limited by the suture lines. A midline shift of the ventricular system is present. This hemorrhage requires immediate surgical evacuation.
-
Axial CT scan that demonstrates a large vertex, bifrontoparietal epidural hemorrhage (EDH). Air bubbles are within the hematoma.
-
CT bone window image of same patient in Media file 2 that demonstrates a large midline fracture.
-
Coronal CT scan reconstruction that further clarifies the thickness and mass effect associated with this vertex epidural hemorrhage (EDH).
-
Sagittal CT scan reconstruction that further defines the anterior-posterior extent of the vertex epidural hemorrhage (EDH).
-
CT image of a pre-adolescent male with a left posterior fossa epidural hemorrhage (EDH). Such hemorrhages need to be watched carefully, and the surgical team should have a low threshold for surgical intervention because this region has less room to accommodate mass lesions.
-
Bone window of the same patient as Media file 6 that reveals a diastasis (separation) of the left mastoid suture.







