Practice Essentials
Spinal cord abscess is a rare entity, particularly in the pediatric population. Spinal cord abscesses can be located in extradural, subdural, and intradural (intramedullary or extramedullary) regions of the cord, with intramedullary being extremely uncommon. [1] Spinal epidural abscess (SEA), an infection of the spinal epidural space, is a potentially devastating entity that is rising in incidence. Its insidious presentation, variable progression, and potential for precipitous neurologic decline make diagnosis and management of SEA challenging. Prompt diagnosis is key because treatment delay can lead to paralysis or death. [2]
The term "intramedullary spinal cord abscess" (ISCA) may be redundant. As with SEA, quick diagnosis and treatment of this condition are critical to preventing long-term serious damage to the spinal cord or possibly death. Although we largely approach and treat these conditions similarly, we should not confuse ISCA with SEA, the latter of which is far more common. [3]
The etiology of ISCA is primarily infectious. There are basically 2 ways that someone can acquire an infection of the parenchyma of the spinal cord: by hematologic transport and by juxtaposition with infected tissue or cerebrospinal fluid. Although ISCA is usually secondary to SEA, other etiologies have been observed. One example is aortic valve endocarditis. In another case, ISCA was associated with a spinal dural arteriovenous fistula, which was conducive to hematogenous infection of the spinal cord. [1, 4, 5, 6, 7]
To remain viable, the spinal cord requires perfusion of its tissues with blood. When the pia mater is violated, or when a patient acquires infection in the bloodstream, the pathogen may penetrate the blood-cord barrier, leaving a certain segment of the population—especially those who are immunocompromised and intravenous drug users—at risk of developing an infection of the spinal cord due to mechanisms similar to those that may cause a brain abscess. [3]
Hart reported the earliest documented spinal cord abscess in 1830. Since then, at least 120 cases have been reported in the medical literature. [3] With modern antibiotics and neurosurgical techniques, even smaller numbers of these infections are expected to be encountered in the future. Because abscesses may occur anywhere along the spinal axis, anatomy varies with the location involved. The most common location for an intramedullary abscess is the posterior thoracic spinal cord.
Intramedullary spinal cord abscesses are rarely encountered in modern neurosurgical practice. Select patients are at high risk for developing an ISCA, which can result in acute neurologic deficits. Patients in whom conservative management has failed may benefit from early surgical intervention. Increased awareness of the ISCA is warranted for its clinical suspicion and emergent treatment in select circumstances. [8]
Spinal cord abscesses have many of the same characteristics as abscesses in other locations. Blood vessel involvement surrounded by an area of infection characterizes hematogenous spread. Areas of softening and early abscess formation characterize subacute infections (1-2 wk duration), whereas a classic abscess wall of fibrotic gliosis surrounding necrotic purulent material characterizes chronic infections. However, spinal cord abscesses do not destroy fiber tracts. Instead, they displace fiber tracts and spread along axonal pathways. [9]
A case of pediatric ISCA involved a 2-year-old boy with a history of neonatal meningitis due to Escherichia coli who presented with refusal to walk and was found to have ISCA at multiple levels. Culture of the abscesses again revealed E. coli. The patient was noted to have a pit located superiorly to his sacral spine. Imaging revealed the presence of a dorsal dermal sinus tract. This case illustrates that it is important to evaluate anatomic abnormalities, especially in the setting of serious bacterial infections such as meningitis, as they have the potential to serve as a reservoir for infection. [1]
Another case report, of a 17-year-old man with ISCA. suggested rupture confirmed by magnetic resonance imaging (MRI). The patient presented with meningeal signs, severe paraplegia, sensory impairment with a sensory level, and urinary retention. Streptococcus intermedius was cultured from cerebrospinal fluid, sputum, and the maxillary sinus abscess. It appeared that S. intermedius transferred from the respiratory tract to the spinal cord hematogenously and formed the ISCA; then the ISCA ruptured. After 56 days of treatment with ampicillin, vancomycin, and meropenem, the patient could walk with a walker. Although this case suggested rupture of ISCA, the patient recovered with antibiotic therapy alone. The authors concluded that earlier diagnosis with MRI and aggressive antibiotic therapy appear to be critical factors for the prognosis of patients with ISCA. [10]
Yet another case report described a 4-year-old boy who had undergone previous surgery for spina bifida (meningocele and tethered cord syndrome). When he was unable to walk after 1 month, he was operated on with the diagnosis of ISCA and continued treatment at another hospital. A subsequent MRI after emergency surgery revealed progression of the intradural abscess. Due to no regression of neurologic deficits on follow-up and the risk of another operation, antimicrobial treatment as well as hyperbaric oxygen therapy (HBOT) was planned. At the end of 20 HBOT treatment sessions, the patient started to walk with support, and antibiotic treatment was completed in 6 weeks. In cases where surgical and antimicrobial treatments have failed, HBOT should be considered as an additional treatment method for children with spinal abscess. [11]
Patients with ISCA present with neurologic findings related to the level of spinal cord involvement; MRI with gadolinium is still the procedure of choice for early diagnosis. Successful outcomes depend upon early diagnosis, aggressive surgical treatment, and appropriate antibiotic treatment following surgery. Even when these guidelines are followed, 70% of patients are left with neurologic sequelae.
The presumptive diagnosis of intramedullary abscess requires prompt definitive diagnosis. This of course necessitates demonstration of infection with subsequent identification of the causative organism. A laminectomy is usually required to diagnose the condition to avoid further decline that may have occurred with continued conservative management. [8]
Neurologic deficits such as paraplegia may occur, depending upon the rapidity with which the abscess is diagnosed and treated and the spinal cord level at which damage is seen on imaging. [1] Because the abscess and the inflammatory process involve the surrounding vasculature, spinal cord infarction may lead to irreversible paraplegia.
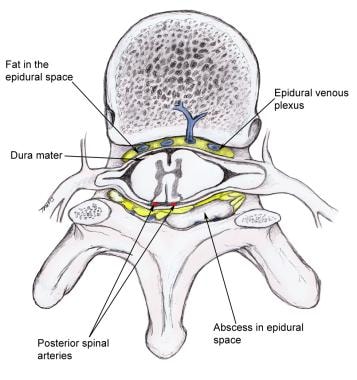
(See the image below.)
Problem
Spinal cord abscesses arise in spinal cord parenchyma and can be solitary or multiple, contiguous or isolated, and chronic or acute, depending upon the organism and the individual patient. As may be expected, solitary lesions are more common and most likely appear in the thoracic cord. Holocord abscesses have been reported in approximately 5 patients.
A case report describes an 18-year-old male who presented to the emergency department with high-grade fever and low backache of 2 weeks’ duration and loss of bowel and bladder control for 4 days. Holocord spinal epidural abscess (HSEA) was diagnosed upon neurologic examination that revealed intact motor power and sensation in all 4 limbs followed by rapid deterioration to complete quadriplegia within 24 hours. The patient was treated with emergent decompression via interval thoracic laminectomy and appropriate antimicrobial therapy and showed complete neurologic recovery at 10 months’ follow-up. This case suggests the possibility of a good prognosis for individuals with HSEA accompanied by neurologic deficit and emergent surgical decompression. [12]
Some researchers divide spinal cord abscesses into primary and secondary, depending on the source of infection. Abscesses are considered primary when no other infection source can be found. Secondary abscesses arise from another infection site, either distant from or contiguous to the spinal cord, most commonly from the lung, spine, heart valves, and genitourinary system. Intramedullary spinal cord abscesses most commonly arise from a secondary source such as the cardiopulmonary system or from a source in close proximity to the cord such as the mediastinum. These classifications rarely affect treatment or patient outcome.
Epidemiology
Spinal cord abscesses occur more frequently in males than in females, with peak incidence in the first and third decades of life. Too few cases have been reported to define any racial predilection. It is uncertain whether this condition is more common in the United States than elsewhere in the world per capita. [3] Patients with a history of intravenous drug abuse are at particularly high risk, as are other immunocompromised patients such as those with HIV, diabetes, or multiple organ failure.
Etiology
The etiology of ISCA is primarily infectious. There are basically 2 ways that someone can acquire an infection of the parenchyma of the spinal cord: by hematologic transport and by juxtaposition with infected tissue or cerebrospinal fluid. Although ISCA is usually secondary to spinal cord epidural abscess, other etiologies have been noted. [3] Organisms most commonly cultured from spinal cord abscesses include Staphylococcus and Streptococcus species, followed by gram-negative organisms. Mixed flora abscesses are also encountered.
Other unusual organisms, including Actinomyces, Listeria, Proteus, Pseudomonas, Histoplasma capsulatum, and the tapeworm Sparganum, have been reported.
In 1899, Hoche demonstrated that abscesses may occur in areas of infarction, thus explaining the common incidence of septic spread to the lower half of the thoracic cord.
The Batson plexus (the confluence of epidural veins in the spinal canal) may contribute to the origin of an abscess by allowing organisms to lodge and thus develop in the spinal cord and its surrounding parenchyma.
Postoperative ISCA due to Mycoplasma hominis has been reported after a neurosurgical procedure. [13] Intramedullary Aspergillus abscess has also been reported. [14]
Presentation
As with most neurologic diseases, signs and symptoms depend upon abscess location and duration. In an acute presentation, symptoms of infection (eg, fever, chills, back pain, malaise) are common. Neurologic symptoms and signs include weakness, paresthesia, dysesthesia, bladder and bowel incontinence, and acute paraplegia. Neurologic signs and symptoms are dependent upon the location of the abscess in the spinal cord; the most common location for an intramedullary abscess is the thoracic spinal cord. Clinical symptoms are similar to those of patients with epidural abscesses, but percussion tenderness is not noted.
In more chronic cases, signs and symptoms mimic those of an intramedullary tumor, and neurologic symptoms predominate over those of a systemic infection. Neurologic progression is gradual. A high degree of awareness is necessary to diagnose chronic spinal cord abscess; in contrast, acute abscesses are generally encountered in extremely ill patients presenting with acute onset of back pain. [15]
Prognosis
The outcome for patients with spinal cord abscess is generally good with appropriate use of antibiotics and surgical treatment. However, abscess location determines residual neurologic deficits. The patient's degree of sepsis ultimately establishes overall mortality. Due to advancements in medicine in the areas of antibiotics, radiology, and surgery, the mortality rate for ISCA was reduced from 90% between 1840 and 1944 to 4% between 1998 and 2007. [3] With steroids and more timely localization through MRI, neurologic deficits can be reduced.
A case report of a patient with ISCA from Th5 to Th12 as shown on MRI concluded that earlier diagnosis with MRI and aggressive antibiotic therapy appear to be critical factors for the prognosis of patients with this extremely rare infection of the central nervous system. [10]
However, patients may be affected by devastating neurologic sequelae and may succumb to this disease. Overall mortality rates vary from 10 to 20%. Moreover, approximately 70% of patients demonstrate residual neurologic sequelae following appropriate treatment. It is important to note that a significant percentage of patients have recurrence of the abscess. Consequently, repeat MRIs are essential for patients' long-term and follow-up care.
In 2 cases of spinal dysraphism complicated by intramedullary abscess, in which children presented with neurologic decline and febrile illness and MRI showed intraspinal abscess, study authors reported that both underwent prompt surgical excision of the sinus tract, exploration of the cord, and treatment with intravenous antibiotics. Given that both demonstrated excellent neurologic recovery, authors concluded that complete surgical excision of the sinus and tract in addition to use of long-term antimicrobials can yield excellent neurologic outcomes. They advocate long-term follow-up because of the potential for late recurrence. [16]
-
Abscess that compresses the spinal cord and its vasculature.