Practice Essentials
A spermatocele is a benign cystic accumulation of sperm that arises from the head of the epididymis. Although often disconcerting to the patient when noticed, these lesions are benign. Spermatoceles can develop in varying locations, ranging from the testicle itself to locations along the course of the vas deferens. [1, 2] Nevertheless, in common usage, spermatoceles are intrascrotal, paratesticular cystic collections of sperm that arise from the epididymis.
Usually smooth, soft, and well-circumscribed, spermatoceles are broadly described as scrotal masses. The differential diagnoses include hydrocele, varicocele, hernia, simple epididymal cyst, and neoplasm. [3] History, examination, and ultrasonography can aid in the differentiation.
Spermatoceles typically arise from the caput (head) of the epididymis, which is located on the superior aspect of the testicle. Conversely, hydroceles are fluid collections that cover the anterior and lateral surfaces the testicle. A varicocele is a dilated plexus of veins along the spermatic cord. A hernia results from persistent patency of the processus vaginalis allowing intra-abdominal contents to pass into the abnormal intrascrotal peritoneal extension.
In contrast to spermatoceles, both varicoceles and hernias may enlarge with the increased intra-abdominal pressure generated during Valsalva maneuvers. Epididymal cysts are often grouped with spermatoceles, and the two may be impossible to differentiate based on gross anatomy. In contrast to the epididymal cyst, spermatocele fluid typically contains sperm.
Spermatoceles are typically asymptomatic and do not require treatment. Intervention may be considered for uncomfortable, painful, or progressively enlarging spermatoceles.
History of the Procedure
The term spermatocele is derived from the Greek spermatos (sperm) and kele (cavity or mass). It has been recognized for more than 100 years.
Treatment for spermatoceles is with sclerotherapy or surgical excision. [4] In the former, aspiration of the fluid from the spermatocele is followed by injection of a sclerosing agent (eg, polidocanol, 99.5% alcohol, 5% ethanolamine oleate, phenol, tetracycline) to reduce recurrences. [5, 6, 7, 8, 9]
Surgery consists of spermatocelectomy; microsurgical spermatocelectomy may reduce the risk of epididymal injury, testicular atrophy, and recurrence. [10, 1] Pathological analysis of spermatocele specimens appears to offer little clinical benefit. [11]
Problem
A spermatocele is a cystic accumulation of sperm that contains fluid typically arising from the head of the epididymis. It is a common benign finding on routine physical examination and is usually smaller than 1 cm. Less commonly, spermatoceles may enlarge to several centimeters. Pain, discomfort, or resultant significant scrotal distortion may prompt surgical intervention. [12]
Epidemiology
Spermatoceles have been incidentally identified in 30% of patients undergoing scrotal ultrasonography for other reasons. The exact prevalence of this common condition has not been defined.
Spermatoceles can occur at any age. The peak incidence is in men over age 65 years. [13]
Etiology
The etiology of spermatoceles in humans remains undefined. Multiple etiologies have been proposed, although none is universally accepted. Some hypotheses include that spermatoceles may arise from efferent ductules, may be aneurysmal dilations of the epididymis, or may be dilation secondary to distal obstruction. In a mouse model of spontaneous spermatocele, distal efferent ducts were found to be occluded by agglutinated germ cells. [14]
Pathophysiology
The specific pathophysiology remains to be elucidated. Although distal obstruction has been theorized as a potential mechanism, the presence of motile sperm in up to 80% of spermatoceles suggests maintenance of proximal patency.
Presentation
Typically, spermatoceles are asymptomatic. They are often incidental findings on testicular self-examination or routine physical examination. As they usually arise from the head of the epididymis, they are found superior to the testicle. They are smooth and spherical and transilluminate on examination. Failure to transilluminate suggests a solid lesion, which warrants further evaluation, including scrotal ultrasonography and possible inguinal exploration. [15, 16, 17]
Torsion of a spermatocele is a very rare cause of acute scrotum pain and occurs when the cyst is twisted around its pedicle. The symptoms are similar to testicular torsion and the diagnosis is usually made during emergency scrotal exploration. [18]
Indications
Surgical intervention is not indicated for the incidental asymptomatic spermatocele. However, if discomfort, pain, or progressive enlargement is bothersome to the patient, discussion regarding excision may ensue. [19] Spermatocelectomy may be offered to symptomatic patients who are reasonable surgical candidates. Anticoagulation is a relative contraindication.
Relevant Anatomy
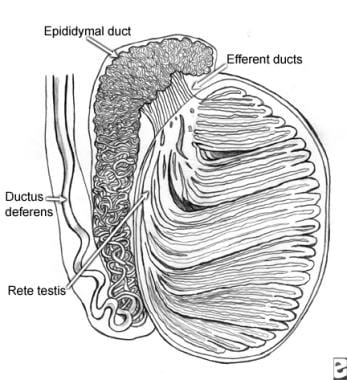
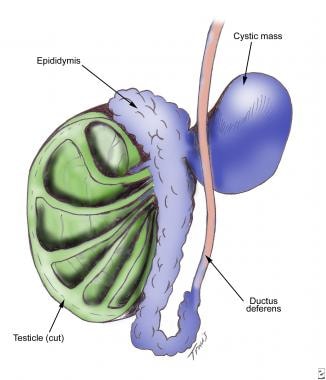
The first image below demonstrates a cross-section of the testicle, epididymis, and vas deferens. The second image is an illustration of a spermatocele. The last two images are intraoperative photographs of a large symptomatic spermatocele.
Contraindications
Needle aspiration of a spermatocele may lead to infection, spillage of irritating sperm within the scrotum, and reaccumulation of the spermatocele. Sclerotherapy is usually not performed in reproductive-aged men because of the risk of chemical epididymitis and resultant epididymal damage, which may contribute to future infertility.
Complications of spermatocelectomy include hematoma and, less commonly, wound infection, scrotal abscess, or recurrence. A partial or total epididymectomy may be preferable to spermatocelectomy if the spermatocele has too many adhesions and dissection is complex. [1]
-
A sagittal section of the testicle. Idiopathic obstruction of the epididymal ducts is one hypothesis that explains the formation of spermatoceles.
-
Diagram of a spermatocele.
-
Spermatocele as seen prior to incision.
-
Intraoperative view of spermatocele with adjacent testicle and spermatic cord.
-
Spermatocele after complete excision.
-
A scrotal ultrasound demonstrating a spermatocele visible to the left of a normal testis.
-
Microscopic view of spermatocele lined with cuboidal epithelium.