Practice Essentials
Uterine cancer is defined as any invasive neoplasm of the uterine corpus. No screening tests for cancer of the uterus are currently recommended for asymptomatic women. The mainstay of primary treatment in endometrial cancer and uterine sarcomas is surgery. (See the image below.)
 Adenocarcinoma of the endometrium. This tumor, which occupies a small uterine cavity, grows primarily as a firm polypoid mass. Courtesy of TELEPATH, Armed Forces Institute of Pathology (AFIP).
Adenocarcinoma of the endometrium. This tumor, which occupies a small uterine cavity, grows primarily as a firm polypoid mass. Courtesy of TELEPATH, Armed Forces Institute of Pathology (AFIP).
Signs and symptoms of uterine cancer
Most patients with endometrial cancer present with abnormal vaginal bleeding. Uterine sarcomas can present in a similar fashion to endometrial carcinomas with vaginal bleeding, and often pelvic pressure as well.
Diagnosis of uterine cancer
Laboratory studies
Although no laboratory tests aid in the diagnosis of uterine cancer, CA-125 has been used in surveillance of advanced or high-grade endometrial cancer.
Imaging studies
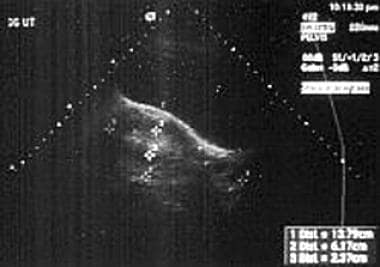
Ultrasonography helps exclude other pelvic pathology that might contribute to postmenopausal bleeding. Endometrial stripe thickness also helps in determining which women with negative findings on office endometrial biopsy samples should have a formal curettage.
See Workup for more detail.
Treatment of uterine cancer
Surgery is the mainstay of primary treatment in endometrial cancer and uterine sarcomas. Radiation has a key role in adjuvant treatment of endometrial cancers and sarcomas. Chemotherapy plays a role in adjuvant therapy for high-grade uterine sarcomas, in addition to high-grade, recurrent, or metastatic endometrial cancer. Hormonal therapy also has a role in adjuvant therapy in receptor-positive uterine cancers.
See Treatment for more detail.
Background
Invasive neoplasms of the female pelvic organs account for almost 15% of all cancers in women. The most common of these malignancies is uterine cancer. An estimated 66,570 cases are diagnosed annually, leading to 12,940 deaths. It is the fourth most common cancer, accounting for 7% of female cancers, following breast, lung, and colorectal cancer. [1]
Endometrial adenocarcinoma is the most common gynecologic malignancy in the United States. However, it has a favorable prognosis because the majority of patients present at an early stage, resulting in only 4% of cancer deaths in women. [1] Uterine sarcomas comprise < 9% of cancers of the uterine corpus; however, they are associated with more aggressive behavior and a poorer prognosis. [2]
History of the Procedure
Cancer of the uterine corpus is the most common pelvic gynecologic malignancy in the United States and in most developed countries with access to sufficient health care. Approximately 95% of these malignancies are carcinomas of the endometrium. The most common symptom in 90% of women is postmenopausal (PMP) bleeding. Most women recognize the need for prompt evaluation, although only 10-20% of women with postmenopausal vaginal bleeding have a gynecologic malignancy. Because of this prompt evaluation, 70-75% of women are diagnosed with surgical stage I disease.
Currently, no screening tests for cancer of the uterus are recommended for asymptomatic women. No evidence suggests that routine endometrial sampling or transvaginal sonography to evaluate the endometrial stripe in asymptomatic women has a role in early detection of uterine cancer, even in women who take tamoxifen after breast cancer or has a cancer syndrome. The early detection, presenting symptoms, and higher survival rate make it unlikely that screening will have a successful impact on improving survival rates.
Approximately eighty percent of endometrial carcinomas are endometrioid adenocarcinomas. Other histologic subtypes include adenosquamous, clear cell, and papillary serous carcinomas. [3] Sarcomas make up about < 9% of uterine corpus malignancies, including carcinosarcomas or mixed homologous müllerian tumors, 48-50%; leiomyosarcomas (LMSs), 38-40%; and endometrial stromal sarcomas (EESs), 8-10%. The remaining sarcomas are made up of heterologous tumors—tumors that contain histologic components foreign to the uterus, such as rhabdomyosarcomas, osteosarcomas, and chondrosarcomas. This article discusses endometrial cancer and uterine sarcomas. See the image below.
Pathophysiology
Fibroblast growth factor receptor 2 (FGFR2) is a tyrosine kinase receptor involved in many biological processes. Mutations in FGFR2 have been reported in up to 10-12% of endometrial carcinomas. Inhibition of FGFR2 could be a new therapeutic target in endometrial carcinoma. Gatius et al suggest that FGFR2 has a dual role in the endometrium, inhibiting cell proliferation in normal endometria during the menstrual cycle but acting as an oncogene in endometrial carcinoma. [4]
Endometrial cancers are divided into 2 classes, each with differing pathophysiology and prognosis.
More than 80% of endometrial carcinomas are type I and are due to unopposed estrogen stimulation, resulting in a low-grade histology. It is often found in association with atypical endometrial hyperplasia, which is thought to be a precursor lesion. Type II endometrial cancers are thought to be estrogen independent, occurring in older women, with high-grade histologies such as uterine papillary serous or clear cell.
Endometrial cancer may originate in a small area (eg, within an endometrial polyp) or in a diffuse multifocal pattern. Early tumor growth is characterized by an exophytic and spreading pattern. This growth is characterized by friability and spontaneous bleeding, even at early stages. Later tumor growth is characterized by myometrial invasion and growth toward the cervix. Four routes of spread occur beyond the uterus:
-
Direct/local spread accounts for most local extension beyond the uterus.
-
Lymphatic spread accounts for spread to pelvic, para-aortic, and, rarely, inguinal lymph nodes.
-
Hematologic spread is responsible for metastases to the lungs, liver, bone, and brain (rare).
-
Peritoneal/transtubal spread results in intraperitoneal implants, particularly with uterine papillary serous carcinoma (UPSC), similar to the pattern observed in ovarian cancer.
Endometrioid adenocarcinoma of the endometrium, the most common histology, is usually preceded by adenomatous hyperplasia with atypia. If left untreated, simple and complex endometrial hyperplasia with atypia progress to adenocarcinoma in 8% and 29% of cases, respectively. Without atypia, simple and complex hyperplasia progress to cancer in only 1% and 3% of cases, respectively. See the image below.
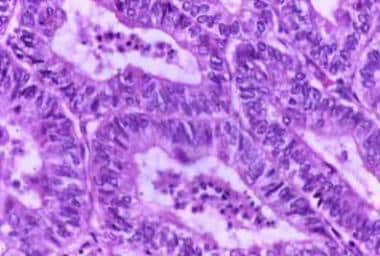 Typical histologic pattern, specifically cribriform glandular appearance, of endometrioid adenocarcinoma of the endometrium. Increased nuclear atypia and mitotic figures are present.
Typical histologic pattern, specifically cribriform glandular appearance, of endometrioid adenocarcinoma of the endometrium. Increased nuclear atypia and mitotic figures are present.
Endometrial adenocarcinoma is histologically characterized by cribriform glands (or glandular crowding) with little, if any, stromal tissue between the glands. Nuclear atypia, variation in gland size, and increased mitoses are common in adenocarcinoma. Well-differentiated tumors may be confused with complex hyperplasia with atypia histologically. Likewise, poorly differentiated tumors might be confused with sarcomas histologically. All papillary serous and clear cell histologies are considered grade 3. The differentiation of endometrial cancers is one of the most important prognostic factors. Grade 1, 2, and 3 tumors make up approximately 45%, 35%, and 20%, respectively, of adenocarcinomas of the endometrium. The 5-year survival rate of clinical stage I cancers is 94%, 88%, and 79% for grade 1, 2, and 3 tumors, respectively. The degree of histologic differentiation of adenocarcinoma of the endometrium as defined by the International Federation of Gynecology and Obstetrics (FIGO) is as follows:
-
FIGO grade 1 - 5% or less of solid/nonglandular areas
-
FIGO grade 2 - 6-50% of solid/nonglandular areas
-
FIGO grade 3 - More than 50% of solid/nonglandular areas
Less histologic differentiation is associated with a higher incidence of deep myometrial invasion and lymph node metastases. Subsequently, the depth of myometrial invasion and presence of tumor in the lymph nodes is directly related to recurrence rates and 5-year survival rates.
Histological variants
The most common histologic subtype of endometrial cancer is endometrioid adenocarcinoma, accounting for about 75-80% of endometrial cancers. Less common histologies include adenosquamous (2%) and mucinous (2%). When corrected for grade, however, the presence of squamous components has not been demonstrated to cause a significant difference in prognosis compared to pure adenocarcinomas. PTEN mutation is thought to be an early event in low-grade endometrial cancers and is found in 55% of hyperplasia and 85% of cancers, whereas it is not found in benign endometrium.
Approximately 15-20% of endometrial cancers are type II cancers with papillary serous or clear cell histologies. Papillary serous histology represents 5-10% and clear cell histology represents less than 5% of endometrial cancers. They are considered high grade with poor prognosis. They have a propensity for early nodal or upper abdominal spread even with minimal or no myometrial invasion. The p53 mutation is more common in high-grade tumors, and ERBB-2 (HER-2/neu) mutation is common in type II cancers. Even with surgical stage I cancer, the 5-year survival rate is 60%. Histologically, uterine papillary serous carcinoma (UPSC) resembles papillary serous carcinoma of the ovary. Although adjuvant chemotherapy is helpful, UPSC does not have the same duration of response to cytotoxic agents (eg, paclitaxel, carboplatin) as its ovarian counterpart.
Carcinosarcomas or malignant mixed müllerian tumors (MMMT) are typically comprised of a high grade epithelial carcinoma and stromal sarcoma. The sarcomatous portion of the tumor may exhibit an endometrial stromal sarcoma (ESS) pattern, if differentiated. The MMMT is considered homologous if the sarcomatous tissue types are native to the uterus. MMMTs are termed heterologous only if identifiable extrauterine histology is demonstrated, such as rhabdomyosarcoma, chondrosarcoma, osteosarcoma, or liposarcoma. MMTs are characterized by early extrauterine spread and lymph node metastases. Extrauterine disease and lymph node metastases are directly related to depth of myometrial invasion and the presence of cervical disease. The presence of heterologous elements does not seem to affect prognosis in terms of the initial extent of disease. New evidence points to a substantial expression of c-kit receptors in MMMTs.
The histopathologic diagnosis of uterine sarcomas can be unclear until the time of definitive surgery. Diagnosis of leiomyosarcoma is dependent on the number of mitoses and the degree of cellular atypia. The diagnosis of leiomyosarcoma versus leiomyoma and leiomyoma with high mitotic activity or uncertain malignant potential is based on the metastatic potential of the tumor. The mitotic count and cellular atypia correlates to this metastatic potential. Although controversy continues to exist regarding the diagnosis of leiomyosarcoma, several studies support the theory that if the mitotic count is less than 5 per 10 high-powered fields (HPF), the tumor is a leiomyoma with negligible metastatic potential regardless of the presence of any cellular atypia. Likewise, the tumor has a high metastatic potential and is considered an leiomyosarcoma, regardless of the degree of cellular atypia, if the mitotic count is greater than 10 per 10 HPF. Some believe that mitotic count alone is not a good indicator of metastatic potential.
Endometrial Stromal Sarcomas (ESS) are a type of uterine cancer arising from the uterine mesenchymal tissue. ESS can be divided into 2 categories: low-grade ESS (LGESS) and high-grade or undifferentiated ESS (HGESS). LGESS is characterized by fewer than 5-10 mitoses per 10 HPF and minimal cellular atypia. These tumors can have a recurrence rate of up to 50% but demonstrate indolent growth and late recurrences. HGESS have a greater mitotic count and degree of cellular atypia with associated necrosis and invasion. Risk of recurrence in both LGESS and HGESS is determined not only by histological characteristics but also by surgical stage and extent of disease.
Uterine adenosarcomas are comprised of mixed epithelial and mesenchymal tissues. They are rare and usually diagnosed with disease confined to the uterus.
Etiology
Endometrioid adenocarcinoma can be due to excess estrogen from various sources, either exogenous or endogenous. Exogenous sources have included unopposed estrogen replacement therapy or tamoxifen use. Tamoxifen increases endometrial cancer risk by its agonist activity on the estrogen receptors on the endometrial lining. Endogenous estrogen sources include obesity and polycystic ovary syndrome (PCOS) with anovulatory cycles, or estrogen-secreting tumors such as granulose cell tumors. Increasing body mass index has been associated with increasing risk of endometrial cancer. [5] Research has found a relative risk of 3 in women 21-50 lb overweight and relative risk over 10 in women more than 50 lb overweight. Androstenedione is converted to estrone, and androgens are aromatized to estradiol in the adipose tissue, leading to higher levels of unopposed estrogen in obese women. See Table 1.
Table 1. Factors Contributing to Endometrial Cancer (Open Table in a new window)
Risk Factor |
Number of Folds Increased Risk |
Estrogen only hormone replacement therapy (HRT) |
2-10 |
Obesity |
2-20 |
PCOS, chronic anovulation |
3 |
Tamoxifen |
2-3 |
Nulliparity |
2-3 |
Early menarche, late menopause |
2-3 |
Hypertension, diabetes |
2-3 |
The other factors associated with increasing one’s risk of endometrial cancer are believed to be related to the same mechanism of increased levels of unopposed estrogen. Nulliparity and infertility are likely related to chronic anovulation. Increased alcohol use can elevate estrogen levels. Late menopause and early menarche can be associated with more anovulatory cycles and thus more unopposed estrogen.
While there is no evidence that screening for endometrial cancer in high-risk populations, such as patients on tamoxifen or patients who have HNPCC syndrome, decreases mortality, some societies advocate screening with endometrial biopsies starting at age 35 years in patients with HNPCC.
Factors that decrease unopposed estrogen are associated with decreased risk of endometrial cancers. The use of combination oral contraceptive pills for 12 months decreases the risk of endometrial cancer by more than 40%. [6] Similarly, postmenopausal women taking the combined estrogen and progesterone hormone replacement therapy have also been found to decrease their rate of endometrial cancer. [7] Smoking is thought to decrease the risk of endometrial cancer by decreasing estrogen levels as well as leading to earlier menopause.
The following have been identified as risk factors for the various uterine sarcomas. Risk factors for uterine leiomyosarcomas may include early menarche, late menopause, and African American race. Women with a history of pelvic radiation are at greatest risk for carcinosarcomas and leiomyosarcomas. Nulliparous women may be at greater risk for both types of sarcomas. Tamoxifen use also increases the risk of endometrial carcinoma as well as uterine sarcomas.
Epidemiology
United States statistics
Approximately 66,570 women were predicted to develop this form of malignancy in 2021 in the United States. After doubling in the early 1970s, the incidence of uterine cancer has remained fairly constant. In 2021, 12,940 deaths were predicted. A woman's lifetime risk is approximately 3.1%. [1]
While endometrial cancer affects reproductive age as well as postmenopausal women, 75% of endometrial cancers occur in postmenopausal women, with the mean age of diagnosis at 61 years. Premenopausal women are at increased risk if they have certain risk factors. [8] The most common low-grade endometrioid endometrial cancers have been associated with obesity, nulliparity, anovulatory menstrual cycles, diabetes, and hypertension. In addition, these younger women are at higher risk for a synchronous primary ovarian cancer, with a rate up to 19-25%. [8, 9]
Another group of women at increased risk of premenopausal endometrial cancer are those with Lynch II syndrome, also known as hereditary nonpolyposis colorectal cancer (HNPCC). This is an autosomally dominant germline mutation in DNA mismatch repair (MMR) genes (MSH1, MSH2, MSH6) and accounts for 9% of patients younger than 50 years with endometrial cancer. These mutations lead to microsatellite instability in 90% of colon cancers and 75% of endometrial cancers. Besides colon cancer, women affected have a 40-60% risk of endometrial cancer by age 70 years, compared to a baseline population risk of 1.5% at the same age. Fifty-one percent of women had endometrial or ovarian cancer diagnosed first as the sentinel cancer. These women are also at increased risk for cancer of the ovary, stomach, small bowel, hepatobiliary system, pancreas, brain, breast, and ureter or kidney. [10, 11]
Incidence of endometrial cancer is higher among Caucasians compared with Asian or Black women; however, mortality is higher among Blacks. This is thought to be due to poor access to care and presentation at more advanced stages.
Uterine sarcomas, regardless of the histologic subtype, are more common in Black women. Leiomyosarcoma (LMS) tends to occur more often in women aged 30-50 years compared with carcinosarcomas and endometrial stromal sarcomas (EES), which have a much higher incidence in women older than 50 years. A meta-analysis found the estimated rate of leiomyosarcomas to be 1 in 2000 uteri removed for presumed benign fibroids. A large health care system found an incidence of 3.6 occult uterine sarcomas per 1000 hysterectomies for fibroids. [12, 13]
Presentation
More than 90% of patients with endometrial cancer will present with abnormal vaginal bleeding, whether it is menorrhagia, metrorrhagia, or any amount of postmenopausal bleeding. Approximately 10% of postmenopausal bleeding will lead to a diagnosis of endometrial cancer. Advanced cases, especially patients with uterine papillary serous or clear cell histologies may present with abdominal pain and bloating or other symptoms of metastatic disease. Other presenting symptoms may include purulent genital discharge, pain, weight loss, and a change in bladder or bowel habits. Fortunately, most cases of endometrial cancer are diagnosed prior to this clinical presentation because of the recognition of postmenopausal bleeding as a possible early symptom of cancer. About 5% of women may be asymptomatic and diagnosed after workup of abnormal Papanicolaou test results.
Uterine sarcomas can present in a similar fashion to endometrial carcinomas with vaginal bleeding, and often pelvic pressure. Imaging will reveal a uterine mass and enlargement. Leiomyosarcoma may present in women early in the sixth decade of life with irregular menses or postmenopausal bleeding. Other symptoms include pain, pelvic pressure, and a rapidly enlarging pelvic mass. Unfortunately, the diagnosis is rarely made prior to definitive surgery. Endometrial stromal sarcoma (ESS) usually presents with postmenopausal bleeding, pelvic pain, and an enlarging mass. Like mixed müllerian tumors (MMT), ESS typically presents in the seventh decade of life. Weight loss, anorexia, and change in bowel or bladder habits are signs of advanced disease in all cases of uterine cancer.
Indications
The mainstay of primary treatment in endometrial cancer and uterine sarcomas is surgery. Radiation has an important role in adjuvant treatment of endometrial cancers and sarcomas. Chemotherapy plays a role in adjuvant therapy for high-grade uterine sarcomas, in addition to high grade, recurrent or metastatic endometrial cancer. Hormonal therapy also has a role in adjuvant therapy in receptor-positive uterine cancers. Details regarding all of these therapies are discussed later in this article.
Like endometrial cancer, primary surgical therapy is the first step in treatment of uterine sarcomas. In fact, these tumors are often found at the time of surgery for benign indications such as uterine leiomyomata and dysfunctional uterine bleeding. Often they are found incidentally on post-operative pathological evaluation of myomectomy or hysterectomy specimen.
Relevant Anatomy
See the images below for relevant surgical anatomy.
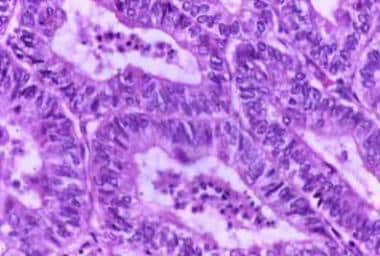 Typical histologic pattern, specifically cribriform glandular appearance, of endometrioid adenocarcinoma of the endometrium. Increased nuclear atypia and mitotic figures are present.
Typical histologic pattern, specifically cribriform glandular appearance, of endometrioid adenocarcinoma of the endometrium. Increased nuclear atypia and mitotic figures are present.
-
Typical histologic pattern, specifically cribriform glandular appearance, of endometrioid adenocarcinoma of the endometrium. Increased nuclear atypia and mitotic figures are present.
-
Transvaginal ultrasonography demonstrating an enlarged endometrial stripe (EMS = 2.4 cm).
-
Adenocarcinoma of the endometrium. This tumor, which occupies a small uterine cavity, grows primarily as a firm polypoid mass. Courtesy of TELEPATH, Armed Forces Institute of Pathology (AFIP).