Practice Essentials
Blunt abdominal trauma (see the image below) is a leading cause of morbidity and mortality among all age groups. Identification of serious intra-abdominal pathology is often challenging; many injuries may not manifest during the initial assessment and treatment period.
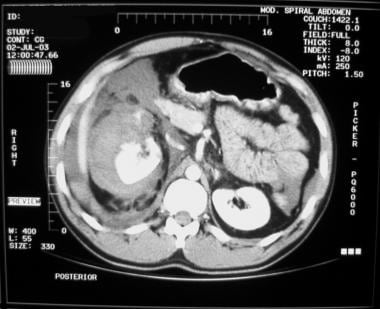 Blunt abdominal trauma. Right kidney injury with blood in perirenal space. Injury resulted from high-speed motor vehicle collision.
Blunt abdominal trauma. Right kidney injury with blood in perirenal space. Injury resulted from high-speed motor vehicle collision.
Signs and symptoms
The initial clinical assessment of patients with blunt abdominal trauma is often difficult and notably inaccurate. The most reliable signs and symptoms in alert patients are as follows:
-
Pain
-
Tenderness
-
Gastrointestinal hemorrhage
-
Hypovolemia
-
Evidence of peritoneal irritation
However, large amounts of blood can accumulate in the peritoneal and pelvic cavities without any significant or early changes in the physical examination findings. Bradycardia may indicate the presence of free intraperitoneal blood.
On physical examination, the following injury patterns predict the potential for intra-abdominal trauma:
-
Lap belt marks: Correlate with small intestine rupture
-
Steering wheel–shaped contusions
-
Ecchymosis involving the flanks (Grey Turner sign) or the umbilicus (Cullen sign): Indicates retroperitoneal hemorrhage, but is usually delayed for several hours to days
-
Abdominal distention
-
Auscultation of bowel sounds in the thorax: May indicate a diaphragmatic injury
-
Abdominal bruit: May indicate underlying vascular disease or traumatic arteriovenous fistula
-
Local or generalized tenderness, guarding, rigidity, or rebound tenderness: Suggests peritoneal injury
-
Fullness and doughy consistency on palpation: May indicate intra-abdominal hemorrhage
-
Crepitation or instability of the lower thoracic cage: Indicates the potential for splenic or hepatic injuries
See Clinical Presentation for more detail.
Diagnosis
Assessment of hemodynamic stability is the most important initial concern in the evaluation of a patient with blunt abdominal trauma. In the hemodynamically unstable patient, a rapid evaluation for hemoperitoneum can be accomplished by means of diagnostic peritoneal lavage (DPL) or the focused assessment with sonography for trauma (FAST). Radiographic studies of the abdomen are indicated in stable patients when the physical examination findings are inconclusive.
Diagnostic peritoneal lavage
DPL is indicated for the following patients in the setting of blunt trauma:
-
Patients with a spinal cord injury
-
Those with multiple injuries and unexplained shock
-
Obtunded patients with a possible abdominal injury
-
Intoxicated patients in whom abdominal injury is suggested
-
Patients with potential intra-abdominal injury who will undergo prolonged anesthesia for another procedure
FAST
Bedside ultrasonography is a rapid, portable, noninvasive, and accurate examination that can be performed by emergency clinicians and trauma surgeons to detect hemoperitoneum.
The current FAST examination protocol consists of 4 acoustic windows (pericardiac, perihepatic, perisplenic, pelvic) with the patient supine.
An examination is interpreted as positive if free fluid is found in any of the 4 acoustic windows, negative if no fluid is seen, and indeterminate if any of the windows cannot be adequately assessed.
Computed tomography
Computed tomography is the standard for detecting solid organ injuries. CT scans provide excellent imaging of the pancreas, duodenum, and genitourinary system.
CT scanning often provides the most detailed images of traumatic pathology and may assist in determination of operative intervention [1, 2, 3, 4] Unlike DPL or FAST, CT can determine the source of hemorrhage.
See Workup for more detail.
Management
Treatment of blunt abdominal trauma begins at the scene of the injury and is continued upon the patient’s arrival at the ED or trauma center. Management may involve nonoperative measures or surgical treatment, as appropriate.
Indications for laparotomy in a patient with blunt abdominal injury include the following:
-
Signs of peritonitis
-
Uncontrolled shock or hemorrhage
-
Clinical deterioration during observation
-
Hemoperitoneum findings on FAST or DPL
Nonoperative management
In blunt abdominal trauma, including severe solid organ injuries, selective nonoperative management has become the standard of care. Nonoperative management strategies are based on CT scan diagnosis and the hemodynamic stability of the patient, as follows:
-
For the most part, pediatric patients can be resuscitated and treated nonoperatively; some pediatric surgeons often transfuse up to 40 mL/kg of blood products in an effort to stabilize a pediatric patient
-
Hemodynamically stable adults with solid organ injuries, primarily those to the liver and spleen, may be candidates for nonoperative management
-
Splenic artery embolotherapy, although not standard of care, may be used for adult blunt splenic injury
-
Nonoperative management involves closely monitoring vital signs and frequently repeating the physical examination
See Treatment and Medication for more detail.
Pathophysiology
Intra-abdominal injuries secondary to blunt force are attributed to collisions between the injured person and the external environment and to acceleration or deceleration forces acting on the person’s internal organs. Blunt force injuries to the abdomen can generally be explained by 3 mechanisms.
The first mechanism is deceleration. Rapid deceleration causes differential movement among adjacent structures. As a result, shear forces are created and cause hollow, solid, visceral organs and vascular pedicles to tear, especially at relatively fixed points of attachment. For example, the distal aorta is attached to the thoracic spine and decelerates much more quickly than the relatively mobile aortic arch. As a result, shear forces in the aorta may cause it to rupture. Similar situations can occur at the renal pedicles and at the cervicothoracic junction of the spinal cord.
Classic deceleration injuries include hepatic tear along the ligamentum teres and intimal injuries to the renal arteries. As bowel loops travel from their mesenteric attachments, thrombosis and mesenteric tears, with resultant splanchnic vessel injuries, can result.
The second mechanism involves crushing. Intra-abdominal contents are crushed between the anterior abdominal wall and the vertebral column or posterior thoracic cage. This produces a crushing effect, to which solid viscera (eg, spleen, liver, kidneys) are especially vulnerable.
The third mechanism is external compression, whether from direct blows or from external compression against a fixed object (eg, lap belt, spinal column). External compressive forces result in a sudden and dramatic rise in intra-abdominal pressure and culminate in rupture of a hollow viscous organ (ie, in accordance with the principles of Boyle law).
The liver and spleen seem to be the most frequently injured organs, though reports vary. The small and large intestines are the next most frequently injured organs. Recent studies show an increased number of hepatic injuries, perhaps reflecting increased use of CT scanning and concomitant identification of more injuries.
Etiology
Vehicular trauma is by far the leading cause of blunt abdominal trauma in the civilian population. Auto-to-auto and auto-to-pedestrian collisions have been cited as causes in 50-75% of cases. Other common etiologies include falls and industrial or recreational accidents. Rare causes of blunt abdominal injuries include iatrogenic trauma during cardiopulmonary resuscitation, manual thrusts to clear an airway, and the Heimlich maneuver.
Background
The care of the trauma patient is demanding and requires speed and efficiency. Evaluating patients who have sustained blunt abdominal trauma remains one of the most challenging and resource-intensive aspects of acute trauma care. [5, 6]
Blunt abdominal trauma is a leading cause of morbidity and mortality among all age groups. Identification of serious intra-abdominal pathology is often challenging. Many injuries may not manifest during the initial assessment and treatment period. Missed intra-abdominal injuries and concealed hemorrhage are frequent causes of increased morbidity and mortality, especially in patients who survive the initial phase after an injury.
Physical examination findings are notoriously unreliable. One reason is that mechanisms of injury often result in other associated injuries that may divert the physician’s attention from potentially life-threatening intra-abdominal pathology. Other common reasons are an altered mental state and drug and alcohol intoxication.
Coordinating a trauma resuscitation demands a thorough understanding of the pathophysiology of trauma and shock, excellent clinical and diagnostic acumen, skill with complex procedures, compassion, and the ability to think rationally in a chaotic milieu.
Blunt abdominal trauma usually results from motor vehicle collisions (MVCs), assaults, recreational accidents, or falls. The most commonly injured organs are the spleen, liver, retroperitoneum, small bowel, kidneys (see the image below), bladder, colorectum, diaphragm, and pancreas. Men tend to be affected slightly more often than women.
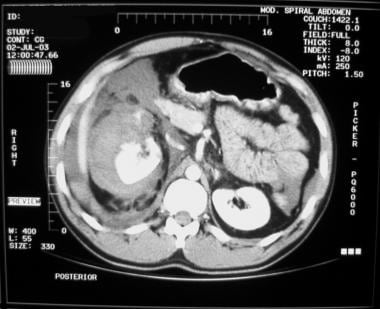 Blunt abdominal trauma. Right kidney injury with blood in perirenal space. Injury resulted from high-speed motor vehicle collision.
Blunt abdominal trauma. Right kidney injury with blood in perirenal space. Injury resulted from high-speed motor vehicle collision.
For more information, see the following:
Anatomy
The abdomen can be arbitrarily divided into 4 areas. The first is the intrathoracic abdomen, which is the portion of the upper abdomen that lies beneath the rib cage. Its contents include the diaphragm, liver, spleen, and stomach. The rib cage makes this area inaccessible to palpation and complete examination.
The second is the pelvic abdomen, which is defined by the bony pelvis. Its contents include the urinary bladder, urethra, rectum, small intestine, and, in females, ovaries, fallopian tubes, and uterus. Injury to these structures may be extraperitoneal in nature and therefore difficult to diagnose.
The third is the retroperitoneal abdomen, which contains the kidneys, ureters, pancreas, aorta, and vena cava. Injuries to these structures are very difficult to diagnose on the basis of physical examination findings. Evaluation of the structures in this region may require computed tomography (CT) scanning, angiography, and intravenous pyelography (IVP).
The fourth is the true abdomen, which contains the small and large intestines, the uterus (if gravid), and the bladder (when distended). Perforation of these organs is associated with significant physical findings and usually manifests with pain and tenderness from peritonitis. Plain x-ray films are helpful if free air is present. Additionally, diagnostic peritoneal lavage (DPL) is a useful adjunct.
Epidemiology
United States statistics
By nearly every measure, injury ranks as one of the most pressing health issues in the United States. More than 150,000 people die each year as a result of injuries, such as motor vehicle crashes, fires, falls, drowning, poisoning, suicide, and homicide. Injuries are the leading cause of death and disability for US children and young adults.
According to the 2000 statistics from the National Center for Injury Prevention and Control, trauma (unintentional and intentional) was the leading cause of death in persons aged 1-44 years. Further review of the data reveals that in those aged 15-25 years, 14,113 persons died from unintentional injuries, 73% of which were related to vehicular trauma. In individuals aged 25-34 years, 57% of the 11,769 deaths reported were from motor vehicle collisions.
In 2001, approximately 30 million people visited emergency departments (EDs) for the treatment of nonfatal injuries, and more than 72,000 people were disabled by injuries. Injury imposes exceptional costs, both in health care dollars and in human losses, to society.
The true frequency of blunt abdominal trauma, however, is unknown. Data collected from trauma centers reflect patients who are transported to or seek care at these centers; these data may not reflect patients presenting to other facilities. The incidence of out-of-hospital deaths is unknown.
One review from the National Pediatric Trauma Registry by Cooper et al reported that 8% of patients (total=25,301) had abdominal injuries. Eighty-three percent of those injuries were from blunt mechanisms. Automobile-related injuries accounted for 59% of those injuries. [7] Similar reviews from adult trauma databases reflect that blunt trauma is the leading cause of intra-abdominal injury and that MVC is the leading mode of injury. Blunt injuries account for approximately two thirds of all injuries.
Hollow viscus trauma is more frequent in the presence of an associated, severe, solid organ injury, particularly to the pancreas. Approximately two thirds of patients with hollow viscus trauma are injured in MVCs.
International statistics
In 1990, approximately 5 million people died worldwide as a result of injury. The risk of death from injury varied strongly by region, age, and sex. Approximately 2 male deaths due to violence were reported for every female death. Injuries accounted for approximately 12.5% of all male deaths, compared with 7.4% of female deaths.
Globally, injury accounts for 10% of all deaths; however, injuries in sub-Saharan Africa are far more destructive than in other areas. In sub-Saharan Africa, the risk of death from trauma is highest in those aged 15-60 years, and the proportion of such deaths from trauma is higher than in any other region of the world. South Africa, for instance, has a traffic death rate per unit of distance traveled that is surpassed only by those of Korea, Kenya, and Morocco.
Estimates indicate that by 2020, 8.4 million people will die yearly from injury, and injuries from traffic collisions will be the third most common cause of disability worldwide and the second most common cause in the developing world.
Data from the World Health Organization (WHO) indicate that falls from heights of less than 5 meters are the leading cause of injury, and automobile crashes are the next most frequent cause. These data reflect all injuries, not just blunt injuries to the abdomen.
A review from Singapore described trauma as the leading cause of death in those aged 1-44 years. Traffic accidents, stab wounds, and falls from heights were the leading modes of injury. Blunt abdominal trauma accounted for 79% of cases. [8]
A similar paper from India reported that blunt abdominal trauma is more frequent in males aged 21-30 years; the majority of patients were injured in automobile accidents. A German study indicated that, of patients with vertical deceleration injuries (ie, falls from heights), only 5.9% had blunt abdominal injuries.
Age-related differences in incidence
Most studies indicate that the peak incidence is in persons aged 14-30 years. A review of 19,261 patients with blunt abdominal trauma revealed equal incidence of hollow viscus injuries in both children (ie, ≤14 y) and adults.
Sex-related differences in incidence
According to national and international data, blunt abdominal trauma is more common in men. The male-to-female ratio is 60:40.
Prognosis
Overall prognosis for patients who sustain blunt abdominal trauma is favorable. Without statistics that indicate the number of out-of-hospital deaths and the total number of patients with blunt trauma to the abdomen, a description of the specific prognosis for patients with intra-abdominal injuries is difficult. Mortality rates for hospitalized patients are approximately 5-10%.
The National Pediatric Trauma Registry reported that 9% of pediatric patients with blunt abdominal trauma died. Of these, only 22% were reported as having intra-abdominal injuries as the likely cause of death. [7]
A review from Australia of intestinal injuries in blunt trauma reported that 85% of injuries occurred from vehicular accidents. The mortality rate was 6%. In a large review of operating room deaths in which blunt trauma accounted for 61% of all injuries, abdominal trauma was the primary identified cause of death in 53.4% of cases.
Patient Education
Proper adjustment of restraints in motor vehicles is an important aspect of patient education. The following are key recommendations:
-
Wear lap belts in conjunction with shoulder restraints.
-
Adjust lap belts so that they fit snugly, and place them across the lower abdomen and below the iliac crests.
-
Wear restraints even in vehicles equipped with supplemental vehicle restraints (eg, airbags).
-
Adjust seats and steering wheels so that the distance between the abdominal wall and the steering wheel is as wide as possible while still allowing proper control of the vehicle.
Advise patients to practice defensive driving by observing speed limits and keeping a safe distance between them and other automobiles on the road.
For patient education resources, see the Kidneys and Urinary System Center, as well as Blood in the Urine and Bruises.
-
Blunt abdominal trauma. Normal Morison pouch (ie, no free fluid).
-
Blunt abdominal trauma. Free fluid in Morison pouch.
-
Blunt abdominal trauma. Normal splenorenal recess.
-
Blunt abdominal trauma. Free fluid in splenorenal recess.
-
Blunt abdominal trauma with splenic injury and hemoperitoneum.
-
Blunt abdominal trauma with liver laceration.
-
Blunt abdominal trauma. Right kidney injury with blood in perirenal space. Injury resulted from high-speed motor vehicle collision.
-
Ultrasound image of right flank. Clear hypoechoic stripe exists between right kidney and liver in Morison pouch.
-
Ultrasound image of left flank in same patient, with thin hypoechoic stripe above spleen and wider hypoechoic stripe in splenorenal recess.
-
Surgical cricothyroidotomy Seldinger. Video courtesy of Therese Canares, MD, and Jonathan Valente, MD, Rhode Island Hospital, Brown University.






