Practice Essentials
The description of varicose veins as a clinical entity can be traced back as early as the fifth century BCE. Hippocrates, Galen, and others described the disease and treatment modalities that are still used today. [1] Throughout the centuries, surgical treatments have evolved from large open procedures to minimally invasive approaches.
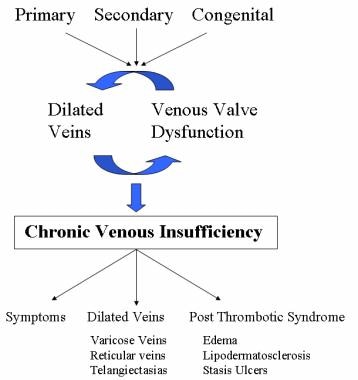
Varicose veins represent a significant clinical problem and are not just a “cosmetic” issue because of their unsightly nature. The problem arises from the fact that varicose veins actually represent underlying chronic venous insufficiency with ensuing venous hypertension. This venous hypertension leads to a broad spectrum of clinical manifestations, ranging from symptoms to cutaneous findings like varicose veins, reticular veins, telangiectasias, swelling, skin discoloration, and ulcerations.
Varicose veins and even chronic venous insufficiency can be managed conservatively with stockings and compression. More aggressive management can be pursued if cosmetic improvement is desired, if cutaneous findings or symptoms worsen despite conservative management, or if the patients prefer surgical management. Most procedures to treat varicose veins can be elective, and emergency treatment and workup are usually reserved for bleeding varicosities or cases where deep venous thrombosis (DVT) is suspected.
For patient education resources, see Varicose Veins, Blood Clot in the Legs, and Phlebitis.
Anatomy
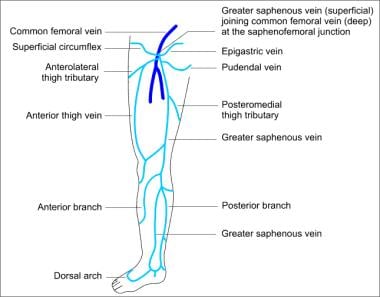
Two venous systems are found in the lower extremity: deep and superficial (see the image below). The deep system ultimately leads backs to the inferior vena cava (IVC), then to the heart. The superficial system is found above the deep fascia of the lower extremity, within the subcutaneous tissue. Many superficial veins exist, but they all drain into the two largest: the great saphenous vein (GSV; also referred to as the long or greater saphenous vein) and the small saphenous vein (SSV; also referred to as the short, smaller, or lesser saphenous vein).
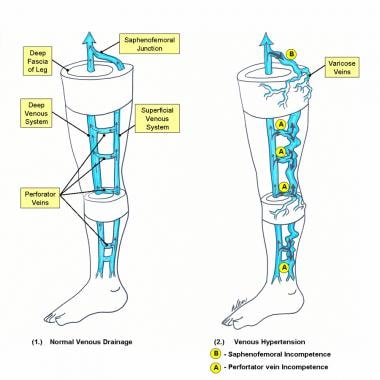 Schematic diagram of deep and superficial venous systems of lower extremity: (1) Normal venous drainage; arrows depict flow of venous blood. (2) Venous hypertension bold arrows are pathways of venous reflux.
Schematic diagram of deep and superficial venous systems of lower extremity: (1) Normal venous drainage; arrows depict flow of venous blood. (2) Venous hypertension bold arrows are pathways of venous reflux.
The GSV originates on the medial foot as part of the venous arch and receives tributaries from deep veins of the foot as it courses upward along the anterior aspect of the medial malleolus. From the ankle, the GSV continues along the anteromedial aspect of the calf to the knee and into the thigh, where it is found more medially.
From the upper calf to the groin, the GSV is usually contained within an envelope of thin fascia. Visualization of this fascial envelope is an important way of identifying the GSV with duplex ultrasonography (DUS). This fascial envelope often prevents the GSV from becoming significantly dilated, even when large volumes of reflux pass along its entire length. A normal GSV is typically 3-4 mm in diameter in the midthigh.
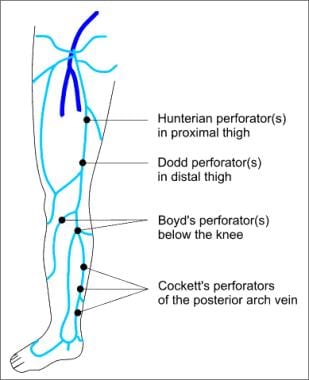
Along its course, a variable number of named perforating veins transverse the deep fascia of the lower extremity and connect the GSV to the deep system at the femoral, posterior tibial, gastrocnemius, and soleal veins (see the image below). The Cockett perforators, between the ankle and the knee, are a special group of perforating veins. Rather than directly connecting the superficial to the deep venous system, they connect the subfascial deep system with the posterior arch vein, which then empties into the GSV.
Besides perforating veins, the GSV has numerous superficial tributaries as it passes through the thigh (see the image below). The most important of these are the posteromedial and anterolateral thigh veins, found at the level of the midthigh, and the anterior and posterior accessory saphenous veins at the level of the canal of Hunter in the upper thigh, where a perforating vein often connects the GSV to the femoral vein.
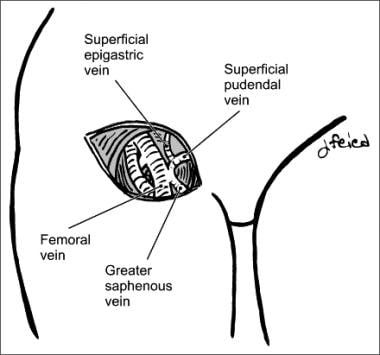
Just below its junction with the common femoral vein, the GSV receives several additional important tributary veins. These include the lateral and medial femoral cutaneous branches, the external circumflex iliac vein, the superficial epigastric vein, and the internal pudendal vein. These tributaries are frequently involved in the reflux that leads to the appearance of surface varicose veins on the lower thigh or upper calf.
The termination point of the GSV into the common femoral vein, located proximally at the groin, is called the saphenofemoral junction (SFJ) in the English literature but is known as the crosse (ie, shepherd's crook) in the French medical literature (see the image below). The terminal valve of the GSV is located within the junction itself. In most cases, at least one additional subterminal valve is present within the first few centimeters of the GSV. Most patients have a single subterminal valve that can be readily identified approximately 1 cm distal to the junctional valve.
The saphenopopliteal junction (SPJ) is located behind the knee where the SSV joins with the popliteal vein.
Pathophysiology
Varicose veins are simply dilated, tortuous veins of the subcutaneous/superficial venous system. However, the pathophysiology behind their formation is complicated and involves the concept of ambulatory venous hypertension. To understand this process, it is necessary to be familair with the anatomy of the lower-extremity venous system, as outlined above (see Anatomy).
In healthy veins, the flow of venous blood is through the superficial system into the deep system and up the leg and toward the heart (see the image below). One-way venous valves are found in both systems and the perforating veins. Incompetence in any of these valves can lead to a disruption in the unidirectional flow of blood toward the heart and result in ambulatory venous hypertension.
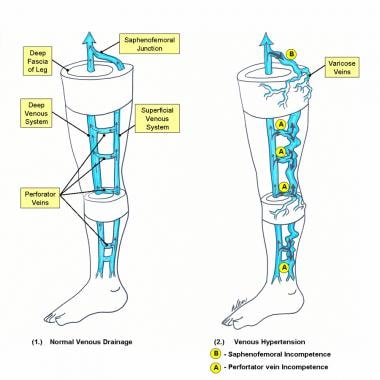 Schematic diagram of deep and superficial venous systems of lower extremity: (1) Normal venous drainage; arrows depict flow of venous blood. (2) Venous hypertension bold arrows are pathways of venous reflux.
Schematic diagram of deep and superficial venous systems of lower extremity: (1) Normal venous drainage; arrows depict flow of venous blood. (2) Venous hypertension bold arrows are pathways of venous reflux.
Furthermore, incompetence in one system can often lead to incompetence in another. In a study by Shami et al, the limbs of 59 patients with venous ulceration were assessed by color DUS scanning. [2] In 53% of patients only superficial venous reflux was found, in 15% isolated deep venous reflux was found, and in 32% a combination of deep and superficial venous reflux was found.
Incompetence in the superficial venous system alone usually results from failure at valves located at the SFJ and the SPJ. The gravitational weight of the column of blood along the length of the vein creates hydrostatic pressure, which is worse at the more distal aspect of the length of vein (see circle A in the image above). [3]
Reflux at or near the SFJ does not always come through the terminal valve of the GSV, nor does it always involve the entire trunk of the GSV. Reflux can enter the GSV below the subterminal valve or even immediately below the junction, passing through a failed subterminal valve to mimic true SFJ incompetence. Reflux can also pass directly into any of the other veins that join the GSV at that level, or it may pass a few centimeters along the GSV and then abandon the GSV for another branch vessel.
When a perforating vein is the primary site of reflux, dilatation of the vessel proceeds both proximally and distally. When dilatation reaches the most proximal portion of the vein, the SFJ or the SPJ is often recruited as a secondary point of reflux. Although most large varices are tributaries off of an incompetent GSV or SSV, failed perforating veins or connecting veins can also give rise to independent varices in the GSV distribution without involving the saphenous system itself. Identifying the originating point and the primary pathway of reflux in the thigh is often difficult, which is why DUS has become so helpful in varicose vein workup. [4, 5]
Incompetence of the perforating veins leads to hydrodynamic pressure. The calf pump mechanism helps to empty the deep venous system, but if perforating vein valves fail, then the pressure generated in the deep venous system by the calf pump mechanism are transmitted into the superficial system via the incompetent perforating veins. [3]
Once venous hypertension is present, the venous dysfunction continues to worsen through a vicious circle. Pooled blood and venous hypertension leads to venous dilatation, which then causes greater valvular insufficiency. Over time, with more local dilatation, other adjacent valves sequentially fail, and after a series of valves has failed, the entire superficial venous system is incompetent.
As mentioned before, this can then cause subsequent perforator and deep venous valvular dysfunction. The inciting etiology of superficial valvular insufficiency is often difficult to determine because the clinical manifestations of venous hypertension are delayed (see Etiology).
The clinical findings of varicose veins, reticular veins, and telangiectasias are due to the hypertension in the superficial venous system that spreads to collateral veins and tributary veins, causing dilated tortuous structures. Treatment modalities are geared towards correcting the superficial venous hypertension. [6]
At times, the degree or venous hypertension does not correlate to the clinical findings. The presence and size of visible varicosities are not reliable indicators of the volume or pressure of venous reflux. A vein that is confined within fascial planes or is buried beneath subcutaneous tissue can carry massive amounts of high-pressure reflux without being visible at all. Conversely, even a small increase in pressure can eventually produce massive dilatation of an otherwise normal superficial vein that carries very little flow.
In contrast to the superficial veins, the deep veins do not become excessively distended. They can withstand the increased pressure because of their construction and the confining fascia.
Etiology
The etiology of varicose veins can be subdivided into three categories: primary, secondary, and congenital (see the image below).
The cause of primary varicose veins is valvular insufficiency of the superficial veins, most commonly at the SFV, resulting in venous hypertension.
Secondary varicose veins are mainly caused by DVT that leads to chronic deep venous obstruction or valvular insufficiency. Long-term clinical sequelae from this have been called the postthrombotic syndrome. This category also includes catheter-associated DVT. Pregnancy-induced and progesterone-induced venous wall and valve weakness worsened by expanded circulating blood volume and enlarged uterus can compress the IVC and hinder venous return from the lower extremities. Trauma is another possible cause of secondary varicose veins.
The congenital category includes any venous malformations. Examples include Klippel-Trenaunay variants and avalvulia.
Epidemiology
The incidence and prevalence of varicose veins has been studied in a number of cross-sectional studies.
In 1973, the US Tecumseh community health study estimated that about 40 million persons (26 million females) in the United States were affected. [7] In 1994, a review by Callam found that half of the adult population have minor stigmata of venous disease (women, 50-55%; men, 40-50%) and that fewer than half have visible varicose veins (women, 20-25%; men, 10-15%). [8] In 2004, these findings were also seen in a French cross-sectional study that found the odds ratio per year for varicose veins to be 1.04 for women and 1.05 for men. [9]
Age and sex have been the only consistently identified risk factors for varicose veins. [7, 9]
Prognosis
With appropriate treatment, the vast majority of patients have a good outcome and the progression of their disease is arrested. Surgical stripping of the GSV, or saphenectomy, has been the criterion standard to which most therapies are compared.
In a randomized trial entitled the EVOLVeS (EndoVenous radiofrequency ObLiteration Versus ligation and Stripping) study, 68 legs were randomly assigned to undergo radiofrequency ablation (RFA) or surgical stripping of the GSV. Immediate success rates for RFA and stripping on the day of treatment were 95% and 100%, respectively. At 3 weeks, DUS confirmed closure of the GSV in 90.9% of the RFA group. [10]
In the extended 2-year follow-up, there was a nonsignificant difference of the cumulative rates of recurrent varicose veins: 14% for RFA and 21% for stripping. However global quality-of-life scores were still in favor of RFA. [11]
In a randomized trial of 137 legs, endovenous laser ablation (EVLA) was compared with saphenectomy. Both methods were equally efficacious at obliterating the GSV, but the saphenectomy group had higher postoperative pain scores. Other similar results between the saphenectomy and EVLA groups included time to resume normal physical activity (7.7 vs 6.9 days), time to resume work (7.6 vs 7 days), and total cost of the procedures ($3948 vs $4347 USD). [12]
In another trial of 280 patients randomized to EVLA compared with saphenectomy, follow-up was extended to more than 1 year. At 1 year, the authors noted lower rates of clinical recurrence with EVLA versus surgery (4% vs 20.4%). Twelve of 23 surgical recurrences were related to an incompetent below-the-knee GSV and 10 to neovascularization. In the EVLA group, five recurrences were reported; two were related to neoreflux in the groin tributaries and one to recanalization. [13]
In a subsequent randomized trial of 500 patients and 580 legs, endovenous ablation, RFA, foam sclerotherapy, and surgical stripping were compared. At 1 year, the failure rates were significantly different in each group. The highest failure rates were seen in the foam ablation (16.3%) and endovenous ablation (5.8%) groups. The lowest failure rates were seen in the RFA (4.8%) and stripping groups (4.8%), though these two groups also had the highest postintervention pain scores. [14]
Foam sclerotherapy has been compared with saphenectomy and sclerotherapy without foam in phase III randomized clinical trials. At 12 months, GSV closure rates were 87.2% for saphenectomy versus 68.2% for Varisolve (BTG, West Conshohocken, PA; now marketed in the United States as Varithena). [15] However, in the other arm (sclerotherapy without foam vs Varisolve), closure rates for Varisolve were much improved (93.8%). Although surgery was more efficacious, Varisolve caused less pain and allowed patients to return to normal more quickly. No pulmonary embolism (PE) was found, and DVT was found in 2.5% of Varisolve patients, no surgery patients, and 0.8% of those who received sclerotherapy without foam.
A study by Obi et al suggested that the combination of transilluminated powered phlebectomy with RFA may yield better outcomes, as measured by the venous clinical severity score, than the use of RFA alone. [16]
A study by Rass et al that included 400 patients with GSV incompetence found the rate of same-site occurrence to be higher after EVLA than after high ligation and stripping of the GSV at 5-year follow-up (18% vs 5%). [17]
In a randomized clinical trial comparing the results of conventional surgery, EVLA, and ultrasonography (US)-guided foam sclerotherapy in patients with varicose GSVs at 5 years, van der Velden et al found that the first two approaches were more effective than the third in obliterating the GSV at the end point of follow-up. [18]
A 2014 Cochrane review found clinical trial evidence to suggest that US-guided foam sclerotherapy, EVLA, and RFA are at least as effective as surgery in treating GSV varicosities, though this evidence was lacking in robustness. [19]
A 2016 Cochrane review comparing endovenous ablation (EVLA or RFA) or foam sclerotherapy with conventional surgical repair for SSV varicosities found that recanalization or persistence of reflux at 6 weeks and recurrence of reflux at 1 year were less frequent with endovenous treatment than with conventional surgery; however, because of low-quality evidence, foam sclerotherapy could not be effectively compared with conventional surgery. [20]
Wallace et al evaluated long-term (5-year) outcomes of EVLA and conventional surgery for symptomatic varicose veins due to GSV incompetence and found the former to be more effective on preventing clinical recurrence. [21] At 5 years, the clinical recurrence rate was 34.3% for surgery and 20.9% for EVLA. Technical success rates as assessed via DUS were 85.4% for surgery and 93.2% for EVLA. Patient-reported outcome measures were similar for the two groups.
In a randomized controlled trial that included 798 patients with primary varicose veins at 11 centers, Brittenden et al compared the 5-year outcomes of EVLA, US-guided foam sclerotherapy, and surgery. [22] The primary outcomes were disease-specific quality of life and generic quality of life, as well as cost-effectiveness. Disease-specific quality of life 5 years after treatment was better after EVLA or surgery than after foam sclerotherapy. The majority of the probabilistic cost-effectiveness model iterations favored laser ablation.
In a randomized controlled trial comparing the success rates and side effects of EVLA (n = 545) and RFA (n = 545) for the treatment of varicose veins in the lower extremities, Tofigh et al found no significant differences between the two procedures with respect to patient characteristics, incidence of major adverse events, and pain severity during the procedure and 8 and 24 hours afterward. [23]
-
Pathway leading to varicose veins and other clinical manifestations of venous hypertension.
-
Telangiectasias.
-
Reticular veins.
-
Varicose veins.
-
Lipodermatosclerosis.
-
Venous stasis ulcer.
-
Schematic diagram of deep and superficial venous systems of lower extremity: (1) Normal venous drainage; arrows depict flow of venous blood. (2) Venous hypertension bold arrows are pathways of venous reflux.
-
Named perforators along great saphenous distribution.
-
Major tributaries of great saphenous system.
-
Saphenofemoral junction.
-
Perforation-invagination (PIN) stripping schematic.
-
Ultrasonogram of great saphenous vein after foam sclerotherapy. Note that hyperechogenicity within vein is from foam.
-
Varisolve canister and appearance of foam with polidocanol.