Practice Essentials
Thoracic outlet syndrome (TOS) is a collective term for a constellation of compressive problems that occur at the thoracic outlet. It has been an important clinical entity for more than a century.
In 1821, Cooper described axillary-subclavian artery symptoms due to compression from a cervical rib. In 1875, Paget described clinical symptoms resulting from subclavian vein thrombosis (eg, arm swelling, pain). In 1884, von Schroetter correctly attributed these upper-extremity symptoms to thrombosis or compression of the subclavian vein at the thoracic outlet. Consequently, venous thrombosis at the thoracic outlet is known as venous TOS or Paget-Schroetter syndrome. [1]
TOS has distinct clinical pictures (ie, neurogenic, arterial, and venous) caused by compression of the neurovascular structures at the thoracic outlet. Classification is based on which structure is primarily involved.
The indication for surgical treatment of neurogenic TOS is the failure of conservative treatment in a patient with disability so severe that the patient is unable to work or live comfortably. The indication for surgical treatment of venous TOS is controversial but is based on symptomatology and venographic evidence of compression at the thoracic outlet. Arterial TOS, however, in most circumstances should be treated surgically with first-rib resection and arterial repair.
Anatomy
The relevant anatomy of TOS focuses on the scalene triangle and the costoclavicular space. Reports of compression of the neurovascular bundle at the area of the pectoralis minor space exist, but this is very uncommon and will not be discussed further.
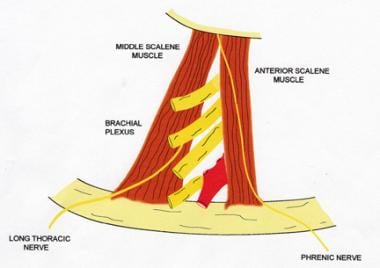
Neurogenic and arterial TOS result from compression that occurs in the scalene triangle, which is defined by the first rib, the anterior scalene muscle, and the middle scalene muscle. The subclavian artery and the branches of the brachial plexus pass through the borders of this triangle (see the image below).
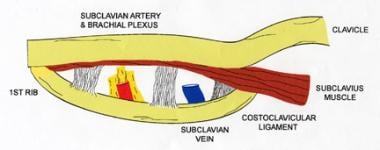
Venous TOS occurs secondary to compression that occurs in the costoclavicular space. The borders of the costoclavicular space are the first rib, the costoclavicular ligament, the subclavius, and the anterior scalene muscle. As the subclavian vein passes through this space, it is susceptible to compression by these structures, as depicted in the image below.
Other important local structures are the phrenic nerve, the lateral thoracic nerve, and the thoracic duct. The phrenic nerve passes from lateral to medial along the anterior border of the anterior scalene muscle, and the lateral thoracic nerve passes through the body of the middle scalene muscle. The thoracic duct joins cervical lymphatics and drains into the superior aspect of the jugulosubclavian vein confluence behind the left sternocleidomastoid muscle. Care must be taken to avoid injury to these structures during surgery.
A search for cervical, rudimentary, or broad first ribs should be done. These structures should be resected during surgical therapy. Rudimentary ribs usually arise higher in the neck than normal first ribs and typically articulate with the second rib rather than with the sternum. Cervical ribs and rudimentary first ribs occur in less than 0.5% of the population.
Abnormal scalene muscle anatomy also has been identified and may be a cause of some symptoms. For example, these muscles have been noted to interdigitate around the cords of the brachial plexus and thus have been implicated in the irritation of the cords of the brachial plexus.
In a study of 98 meticulously dissected cadavers, the authors noted a number of abnormalities of the thoracic outlet fibrous bands and cervical ribs, and other abnormalities were found in most of the patients. Only 10% of the dissected cadavers were found to have normal anatomy bilaterally.
Pathophysiology
Neurogenic TOS most commonly is associated with a history of neck trauma. Swollen and scarred muscles or aberrant scalene anatomy can irritate cords of the brachial plexus locally and lead to the neurologic symptoms.
Arterial TOS often is associated with cervical ribs or a rudimentary first rib. [2, 3] This aberrant anatomy leads to repeated intermittent arterial compression coinciding with arm movement. This repetitive localized trauma leads to intimal lesions, focal arterial stenosis, poststenotic dilatation, aneurysmal change, and subsequent thromboembolic complications. The second portion of the subclavian artery, which has a retroscalene position, often is the site of positional compression and stricture.
Venous TOS usually results from compression of the subclavian vein by the subclavius and the costoclavicular ligament. [4] When local structures are placed in abnormal or unaccustomed positions by extremes of activity or injury, vein compression and subsequent vein thrombosis can result. Venous TOS tends to occur in the more active dominant extremity.
Arterial and venous TOS usually are associated with certain predisposing anatomic abnormalities, whereas neurogenic TOS is more likely to result after traumatic injury.
Etiology
The potential for either neurologic or vascular compression exists at the thoracic outlet. When compression occurs, one of the TOSs may develop. Neurogenic and arterial TOS result from compression that occurs in the scalene triangle (see the first image below), and venous TOS results from compression in the costoclavicular space (see the second image below). [5]
Epidemiology
Neurogenic TOS is the most common presentation, reported to occur in approximately 95% of patients. Arterial TOS is the next most common presentation, reported to occur in about 2-3% of patients who are affected. Venous TOS is the least common presentation, accounting for about 1-2% of patients with TOS.
In a single-institution study by Illig et al, the annual incidence of neurogenic TOS was cited as 2-3 cases per 100,000 population, whereas that of venous TOS was 0.5-1.0 per 100,000 population; arterial TOS was sporadic. [6]
Approximately 70% of patients with neurogenic TOS are females aged 20-50 years. Venous TOS occurs with a male-to-female ratio of 2:1.
Prognosis
Most patients do not experience full relief of symptoms after surgery for neurogenic TOS. A good result occurs when partial relief is achieved and symptoms do not progress. Approximately 40-80% of patients who undergo surgical treatment have some relief of symptoms. Approximately 10-15% of patients who initially experience symptomatic relief have recurrence of symptoms.
If only first-rib resection was performed, these patients may benefit from anterior and middle scalenectomy along with neurolysis. If only scalenectomy was performed, a second operation with first-rib resection and neurolysis may be considered. Only 40% of patients experience long-term symptomatic relief after reoperation for TOS.
Patients with arterial and venous TOS usually do well if workup and treatment have been appropriate.
A systematic review (40 case reports, 10 clinical studies, 28 literature reviews) by Garraud et al found that the prognosis for TOS in athletes appeared to be generally better than that in in the general population, possibly because of better physical condition and younger age. [7]
In a study that used data from the American College of Surgeons (ACS) National Surgical Quality Improvement Program (NSQIP) to evaluate 30-day outcomes of brachial plexus surgical decompression for TOS (N = 225), first and/or cervical rib resection (± scalenectomy; n = 205) was compared with rib-sparing scalenectomy (n = 20). [8] Rib resection was associated with longer operating times and hospital stays. Only eight patients experienced complications at 30 days, of whom seven were in the rib-resection group.
A review of outcomes for 538 patients who underwent 594 first-rib resections for neurogenic (n = 308), venous (n = 261), or arterial (n = 25) TOS reported excellent results, attributed to appropriate selection of neurogenic TOS patients, use of a standard protocol for venous TOS patients, and expeditious intervention in arterial TOS patients. [9]
A systematic review of outcomes for transaxillary first-rib excision (TAFRE), supraclavicular first-rib excision with scalenectomy (SCFRE), and supraclavicular release leaving the first rib intact (SCR) in patients with neurogenic TOS found that SCR had a high probability of a success rate greater than 80%, whereas both TAFRE and SCFRE had a low probability of a success rate greater than 80% but a high probability of a success rate greater than 70%. [10] The complication rates were 22.5% for TAFRE, 25.9% for SCFRE, and 12.6% for SCR.
-
Thoracic outlet obstruction. Scalene triangle.
-
Thoracic outlet obstruction. Costoclavicular space.
-
Thoracic outlet obstruction. Three-dimensional CT scan showing subclavian artery at the thoracic outlet.
-
Thoracic outlet obstruction. Three-dimensional CT scan showing subclavian artery with the arm abducted.
-
Thoracic outlet obstruction. CT scan, maximal intensity projection (MIP), showing subclavian artery in the neutral position.
-
Thoracic outlet obstruction. CT scan, maximal intensity projection (MIP), showing subclavian artery when arm is abducted.
-
Thoracic outlet obstruction. CT scan, maximal intensity projection (MIP), showing subclavian vein in neutral position.
-
Thoracic outlet obstruction. CT scan, maximal intensity projection (MIP), showing subclavian vein in abducted position.
-
Thoracic outlet obstruction. Angiogram showing subclavian artery aneurysm in abduction/external rotation (AER).
-
Thoracic outlet obstruction. Venogram showing venous stenosis.