Practice Essentials
Sir James Paget first described thrombosis of the subclavian veins in 1875. [1] He coined the name gouty phlebitis to describe the spontaneous thrombosis of the veins draining the upper extremity. Paget noted that the syndrome was accompanied by pain and swelling of the affected extremity, but he incorrectly attributed the syndrome to vasospasm. In 1884, von Schrötter postulated that this syndrome resulted from occlusive thrombosis of the subclavian and axillary veins. [2] In 1949, in recognition of the work of these pioneers, Hughes coined the term Paget–von Schrötter syndrome. [3]
A related condition is thrombosis of the subclavian vein that is induced by the presence of indwelling catheters. The incidence of this condition has increased remarkably over the past two decades because of the extensive use of central venous catheters (CVCs) in patients with cancer, renal failure and other chronic medical conditions.
Because the symptoms of subclavian stenosis are fairly dramatic, most patients present promptly to the emergency department (ED), usually within 24 hours. However, not all patients with subclavian vein thrombosis are symptomatic. (See Presentation.)
Patients with suspected thrombophilia should have a full workup for hereditary causes. Appropriate studies should be performed before anticoagulation is initiated. Other tests to be performed should be relevant to the cause of the thrombosis. Imaging studies are done to provide objective verification of the presence of thrombus in the subclavian vein and may include chest radiography, ultrasonography (US), venography, computed tomography (CT), or magnetic resonance imaging (MRI). (See Workup.)
In patients with effort-induced vein thrombosis of less than 2 weeks' duration, thrombolytic therapy is recommended. Chronic axillary-subclavian vein thrombosis (ASVT) rarely responds to thrombolytics and generally is better treated either conservatively with warfarin or, if symptoms are severe, with surgical bypass. Surgery is rarely indicated for ASVT associated with central lines. (See Treatment.)
The demand for a more standardized treatment of subclavian vein thrombosis is growing. However, until randomized data from well-designed trials are available, absolute statements about treatments cannot be made. Linked medical records using administrative healthcare data sets may provide information (eg, readmission rate or level of outpatient services) on the results of treatment of large numbers of patients with subclavian vein thrombosis or significant risk factors (eg, central venous cannulation). Until such information is obtained, the best way of treating subclavian vein thrombosis is to prevent it by limiting the use of CVCs for extended periods.
For patient education resources, see Phlebitis.
Anatomy
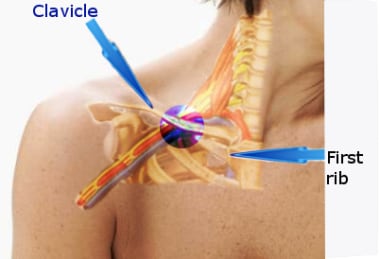
The subclavian vein courses over the first rib and posterior to the clavicle; the artery lies superior and posterior to the vein (see the image below).
Pathophysiology
During long-term venous catheterization of the subclavian vein and internal jugular vein in cancer patients, the risks of complications appear to be similar. However, for short-term catheterization, subclavian vein catheterization is recommended because of the decreased risks of thrombotic complications and catheter colonization by skin flora. For patients requiring hemodialysis, the femoral and internal jugular veins appear to have similar thrombotic complications. However, the risk of mechanical complications via the internal jugular vein appear to be higher. The subclavian vein should be avoided for both long- and short-term hemodialysis because the risk of thrombosis is very high. [4]
Differentiating catheter-associated subclavian vein thrombosis from Paget–von Schrötter syndrome is important because the two conditions appear to have different natural histories.
Paget–von Schrötter syndrome
This syndrome sometimes is referred to as spontaneous ASVT to express the usually dramatic unexpected presentation of the disorder in otherwise healthy, generally young individuals. [5] Over the past few decades, there has been growing recognition that the disorder can occur equally in both sexes and can affect all age groups. In the 1960s, the term effort-induced thrombosis was applied to this disease to acknowledge that it often follows unusually strenuous use of the arm or shoulder on the affected side.
The pathophysiology of effort-induced thrombosis is multifactorial. It involves compressive changes in the vessel wall, stasis of blood, overuse of the upper arm, and hypercoagulability. External compression of the axillary-subclavian vein has been suggested to contribute to the stasis of blood that engenders thrombosis. The factors that cause external compression include the following:
-
Anomalous subclavius or scalenus anterior, long transverse process of cervical spine, cervical rib, abnormal insertion of the first rib, congenital fibromuscular bands, or narrowing of the costoclavicular space from depression of the shoulder
-
Stress from exercise temporarily causing hypercoagulability
-
Repetitive shoulder-arm motion causing microscopic intimal tears in the vessel wall
These factors, taken together, satisfy the classic Virchow triad for thrombosis. Furthermore, coexistent hematologic abnormalities that can contribute to thrombosis include protein C deficiency, antithrombin III deficiency, factor V Leiden mutation, and prothrombin 20210A mutation.
Catheter-induced subclavian vein thrombosis
Introducing catheters and transvenous pacemakers in to the subclavian vein alters the venous flow and increases turbulence. This results in platelet aggregation, release of procoagulants, and, ultimately, fibrin deposition. This causes a further reduction in the lumen of the vessel due to thrombus formation, which eventually culminates in total vessel occlusion. Intravenous (IV) medications and even parenteral nutrition have been known to cause thrombophlebitis. In patients with cancer, an additional contributing factor is that the tumor may generate procoagulant factors, predisposing to thrombosis at sites remote from the tumor.
Etiology
The primary etiology is referred to as effort-induced thrombosis or Paget–von Schrötter syndrome. It usually results from the excessive use of the involved arm by predisposed individuals. The secondary etiology is subclavian vein catheterization, especially in patients with cancer. (For detailed descriptions of catheterization techniques, see Central Venous Access via Infraclavicular (Subclavian) Approach to Subclavian Vein and Central Venous Access via Supraclavicular Approach to Subclavian Vein.)
Other causes include transvenous pacemakers, factor V Leiden mutation, protein C deficiency, protein S deficiency, antithrombin III deficiency, and prothrombin 20210A mutation. Long-term parenteral nutrition [6] and use of hemodialysis catheters [7] account for some cases of subclavian vein thrombosis. Trauma is only rarely associated with this syndrome. Overall, the risk of subclavian vein thrombosis is much greater when catheters are placed in the subclavian vein rather than the internal jugular vein. [7]
In a few cases, the diagnosis remains unknown. However, routine follow-up with these patients has revealed the development of lung cancer within 1 year of follow-up. The most common lung malignancy associated with subclavian thrombosis has been the Pancoast tumor.
Epidemiology
Before 1967, thrombosis of the axillary or subclavian vein accounted for 1-2% of all cases of deep vein thrombosis (DVT). Since then, the incidence has risen as a consequence of more frequent use of central venous access for multiple clinical conditions. Among patients with effort-induced thrombosis with subclavian vein stenosis, the thrombosis occurs in the dominant arm in 80% of cases.
Prognosis
Case fatality rates for untreated ASVT-related pulmonary embolism (PE) may be as high as 10%, a figure comparable to that seen with PE originating from the lower extremity. The long-term consequences of venous occlusion cause substantial morbidity related to persistent pain and swelling for protracted periods. These symptoms occasionally are severe and can be exacerbated by physical activity, particularly with extended use of the affected arm. Consequently, this syndrome can lead to occupational disability and can adversely impact the patient's quality of life.
Conservative treatment consisting of bed rest, limb elevation, and anticoagulation is associated with a worse outcome. Some reports suggest that as many as 74% of patients treated with these conservative measures have residual disability as compared with those who are treated with thrombolysis.
With advances in endovascular technology, there is more supporting evidence that these techniques are the modality of choice in the management of a patient with upper-extremity thrombosis. Anticoagulation or thrombolytic therapy alone has proved inadequate. Today, both benign and malignant causes of upper-extremity thrombosis can be managed with endovascular stenting. This technique allows much faster recovery while giving rise to less morbidity and fewer complications in the long run. [5]
A study by Mahmoud et al reported acceptable intermediate-term results for the treatment of Paget-Schrötter syndrome with a three-stage approach that included early thrombus removal, thoracoscopic first-rib resection, and postoperative venous balloon angioplasty. [8]
-
Figure shows area where subclavian vein is obstructed in neck region. Vein is usually compressed by first rib, clavicle, and serratus anterior muscle.
-
Venogram in patient with subclavian vein obstruction. Long-standing obstruction causes development of collaterals.
-
Recanalization after thrombolytic therapy and stent placement. Patient underwent first rib resection and scalenectomy later.
-
Young baseball pitcher who developed subclavian vein thrombosis with significant swelling of dominant right arm.
-
Subclavian vein prior to angioplasty.
-
Balloon dilatation of right subclavian vein.
-
Subclavian vein post balloon dilatation.