Practice Essentials
Phlegmasia stems from a Greek term (phlegma) meaning inflammation. It has been used in the medical literature in reference to extreme cases of lower-extremity deep venous thrombosis (DVT) that cause critical limb ischemia (CLI) and possible limb loss. Phlegmasia alba dolens (PAD) describes the patient with swollen and white leg because of early compromise of arterial flow secondary to extensive DVT. This condition is also known as “milk leg,” especially as it affects women in the third trimester of pregnancy or post partum.
Phlegmasia cerulea dolens (PCD) is more advanced and considered a precursor of frank venous gangrene. [1] It is characterized by severe swelling and cyanosis and blue discoloration of the extremity. It was first described by Hildanus in the 16th century. Later, the term PCD was first used by Gregoire in 1938. Its rarity notwithstanding, phlegmasia is a life-threatening condition. It is crucial for nonvascular specialists to be able to recognize this condition promptly and accurately; treatment is time-sensitive. (See Presentation and Workup.)
Treatment should be initiated as soon as the diagnosis is suspected, beginning with anticoagulation and elevation of the involved extremity. If patients improve with elevation and anticoagulation and do not progress to CLI, compression therapy with stockings or elastic bandages may be helpful and may be used as tolerated. Catheter-directed thrombolytic therapy is the mainstay of therapy for the extensive DVT that is usually associated with phlegmasia. Open surgical thrombectomy is an alternative for patients who cannot undergo thrombolysis and who require thrombus removal. (See Treatment.)
For patients with acute compartment syndrome, a four-compartment fasciotomy and decompression are required. Finally, if all efforts fail, an amputation is necessary.
Pathophysiology
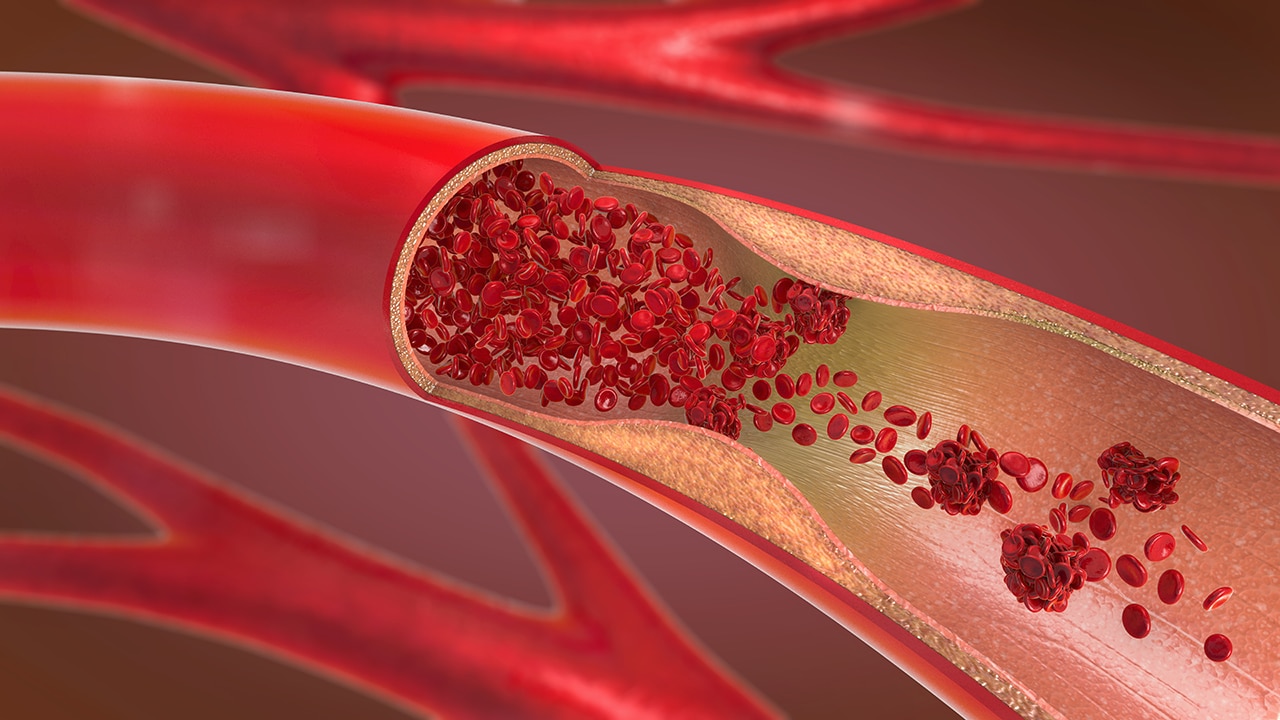
In PAD, the thrombosis involves only major deep venous channels of the extremity, thus sparing collateral veins. The venous drainage is decreased but still present; the lack of cyanosis differentiates this entity from PCD. In PCD, the thrombosis extends to collateral veins, resulting in severe venous congestion with massive fluid sequestration and more significant edema. Without established gangrene, these phases are reversible if proper measures are taken.
Of PCD cases, 40-60% also have capillary involvement, which results in irreversible venous gangrene that involves the skin, subcutaneous tissue, or muscle. [4] Under these conditions, the hydrostatic pressure in arterial and venous capillaries exceeds the oncotic pressure, causing fluid sequestration in the interstitium. Venous pressure may increase rapidly, as much as 16- to 17-fold within 6 hours. [5, 6]
Fluid sequestration may reach 6-10 L in the affected extremity within days. Circulatory shock, which is present in about one third of patients, and arterial insufficiency may ensue. The exact mechanism for the compromised arterial circulation is debatable but may involve shock, increased venous outflow resistance, and collapse of arterioles due to increased interstitial pressure.
Epidemiology
DVT affects as many as 2 million Americans every year. The majority of patients are treated medically, with anticoagulation being the mainstay of therapy to promote thrombus resolution and prevent propagation and embolization. Because phlegmasia is a rare condition, its incidence is unknown. The best estimate is derived from case series of patients treated for extensive DVT. In more recent series, 10-20% of patients undergoing thrombolysis with possible stenting for extensive DVT presented with phlegmasia. [7, 8, 9]
The prevalence is thought to be slightly higher in men than in women, with a male-to-female ratio of 1.5:1. [10]
Prognosis
Despite all the therapeutic modalities currently available, PCD and venous gangrene remain life-threatening and limb-threatening conditions, with overall mortality in the range of 20-40%. Pulmonary embolism (PE) is responsible for 30% of the deaths reported from PCD. Overall, amputation rates of 12-50% have been reported among survivors. The postphlebitic sequelae are apparent in 60-94% of survivors. Strict adherence to the use of long-term compression stockings helps control chronic edema. [10, 4]
-
Principal deep veins of the lower extremity.