Practice Essentials
Subclavian artery thrombosis is a condition in which the blood flow through the subclavian artery is obstructed. [1] The occlusion typically arises secondary to damage to the intima of the vessel. This damage can occur as a result of external muscular compression and repetitive stress to the artery or because of atherosclerotic changes to the vessel. Embolic phenomena and hypercoagulable states are also contributing factors.
Symptoms occur secondary to lack of blood flow to the affected extremity. To maintain blood supply to the extremity, blood is naturally rerouted from the vertebral, carotid, and internal mammary arteries, producing the various steal syndromes.
Subclavian artery thrombosis is common in young athletic individuals who exert a significant amount of upper body activity. [2] Sudden occlusion from emboli followed by thrombosis of the artery is common in the population with signs of significant atherosclerotic disease.
The patient presenting with acute subclavian artery occlusion usually has a history of repetitive use of or stress injury to the upper extremity on the affected side. A history of upper-extremity claudication is common.
In situations where the occlusion is secondary to atherosclerosis, acute thromboses of the artery are generally asymptomatic. In fact, in 9% of autopsy series, the left subclavian artery was either stenotic or occluded. If symptoms are present, upper-extremity claudication on the affected side is most common. The patient may also present with dizziness, vertigo, imbalance, visual disturbances, or hemisensory dysfunction indicative of a subclavian steal syndrome. [3] However, note that subclavian steal is observed on 2% of cerebral angiograms and causes no symptoms.
Therapeutic intervention is indicated in any symptomatic patient once the etiology of the symptoms has been defined. Contraindications for surgical intervention include the following:
-
Inadequate distal runoff
-
Inadequate vessel size
-
Marked collateralization of the occluded area
-
Concomitant medical problems that would endanger the patient during a surgical intervention
In any operative procedure for subclavian artery thrombosis, care must be taken to protect the thoracic duct from damage. Future therapy for subclavian artery thrombosis is likely to involve increasing use of endovascular stents.
Anatomy
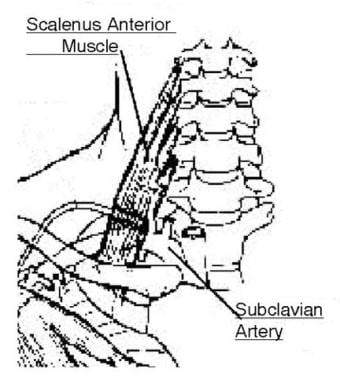
In patients with subclavian artery occlusion secondary to variations in the thoracic outlet, two areas can undergo vascular compression during hyperabduction of the extremity. One site is where the axillary artery passes posterior to the pectoralis minor and beneath the coracoid process. The other point is where the artery courses between the clavicle and the first rib. Fibrous tissue proliferation in this area can impose extrinsic compression on the vessel. (See the image below.)
Aberrant origins of the subclavian artery off the aortic arch can be a cause of subclavian artery occlusion. [4] In atherosclerotic disease, the carotid-subclavian and carotid-vertebral junctions are areas that appear to be predisposed to atheromata formation and calcification. Subsequently, this region is most likely to be involved in the occlusive process. [5] Areas of the subclavian artery that are exposed to repeated forms of injury resulting in intimal damage are predisposed to occlusion.
Pathophysiology
The affected artery demonstrates detectable intimal damage, which is usually secondary to compressive forces exerted by the muscles of the shoulder girdle that compress the artery. Bony abnormalities in this area can also contribute to the process. [6] As these muscles enlarge secondary to physical activity, they exert pressure on the artery. This pressure, coupled with exertional activity of the upper extremity, can stretch and compress the intima, thereby disrupting its natural integrity. This disruption precipitates platelet deposition in the area, with resulting thrombosis.
Atherosclerotic changes in the vessel occur secondary to the flow characteristics in the area. These depositions are accelerated by all of the dietary and sociologic influences that affect the progression of atherosclerotic disease, including smoking, hypercholesterolemia, and hypertension. Occlusion secondary to atherosclerosis is more insidious and often causes no symptoms. At times, the symptom complex of claudication precedes the actual loss of blood flow.
Patients with hypercoagulable states, either intrinsic or secondary to dehydration complicated by concomitant cardiac arrhythmias and systemic inflammatory processes, make up a small subset of individuals who may exhibit this pathology.
Etiology
The occlusion arises secondary to damage to the intima of the artery. This damage can occur as a result of external muscular compression and repetitive stress to the artery, atherosclerotic changes to the vessel, or inflammatory processes.
Embolic or thrombotic occlusion of the artery occurs, particularly in the presence of atherosclerotic stenoses. Hypercoagulable states contribute to this scenario.
Epidemiology
Symptomatic lesions occur in less than 1% of the population. In autopsy series, 9% of the population demonstrate stenosis or occlusion of one subclavian artery, usually on the left. About 2% of cerebral angiograms demonstrate asymptomatic subclavian steal.
Prognosis
The results from stenting procedures on the subclavian artery have documented an 87% patency rate after 3 years. Karpenko et al, in a study assessing endovascular treatment of atherosclerotic steno-occlusive disease of the subclavian artery in 245 patients, reported 4-year patency rates of 89.8% in patients with stenosis (n = 125) and 87% in those with occlusion (n = 120). [7]
Outcomes from operative treatment of subclavian artery thrombosis have demonstrated a patency rate of approximately 90% after 5 years.
The prognosis for the patient with atherosclerotic disease is directly dependent on the severity of the disease and on the willingness of the patient to make lifestyle modifications, including cessation of tobacco use and regulation of diet. If these modifications are made, the progression of the atherosclerotic process slows, and the risk of recurrence of thrombosis falls.
For the patient whose occlusion is secondary to thoracic outlet problems, the prognosis after therapy is excellent.
-
The anatomy of the subclavian artery in the thoracic outlet.
-
Carotid-subclavian bypass for subclavian steal syndrome.
-
Subclavian-subclavian or axillary-axillary bypass for subclavian artery occlusion.