Practice Essentials
Permanent communication caused by erosion of the pancreatic or peripancreatic artery into a pseudocyst gives rise to a rare but life-threatening complication known as a pancreatic pseudoaneurysm. Pancreatitis with secondary pseudocyst formation is the most common cause of pancreatic pseudoaneurysms, though they have been known to occur in the absence of a pseudocyst. [1] The literature confirms that differentiating a pseudoaneurysm from a bleeding pseudocyst is difficult. [2]
A pseudoaneurysm differs from a true aneurysm in that its wall does not contain the components of an artery but instead consists of fibrous tissue, which usually continues to enlarge, creating a pulsating hematoma.
Pancreatic pseudoaneurysm should be distinguished from primary peripancreatic vessel aneurysm, which tends to occur more often in women. The rare rupture of a primary aneurysm tends to occur in pregnancy and manifests as massive intraperitoneal bleeding with hemodynamic instability.
Overall, the splenic artery is the most frequent site of visceral artery pseudoaneurysms, followed by the hepatic artery. [3] Pseudoaneurysm formation may have an incidence as high as 10% in patients with chronic pancreatitis who undergo angiography.
Pancreatic pseudoaneurysms, though rather uncommon, are frequently accompanied by life-threatening complications, mainly rupture and bleeding. Hemorrhage can occur in the pseudocyst itself, via the ampulla of Vater, or by fistulation into nearby hollow organs.
Better outcomes require accurate, timely, and appropriate diagnosis and intervention (medical, surgical, or both). The standard of care in dealing with pancreatic pseudoaneurysms has been surgical intervention. However, owing to advances in the field of interventional radiology, the paradigm has largely shifted toward endovascular treatment of these lesions. [4, 5, 6, 7]
Anatomy
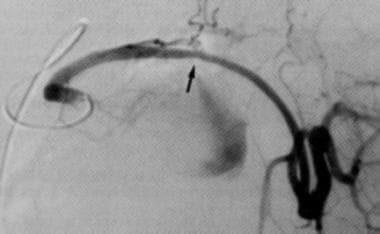
The splenic artery, which is most commonly involved in pancreatic pseudoaneurysm, is one of the three branches of the celiac artery, the other two being the common hepatic artery and the left gastric artery. Because the splenic artery runs along the pancreatic bed before reaching the spleen, it is the artery most commonly affected by the erosive effect of pancreatitis. (See the image below.)
After giving off the hepatic artery proper, the common hepatic artery becomes the gastroduodenal artery, which gives rise to the superior pancreaticoduodenal artery. The pancreaticoduodenal artery anastomoses with the inferior branch coming off the superior mesenteric artery to supply the head of the pancreas and the duodenum.
In addition to encasing the distal end of the common bile duct, the pancreas, a retroperitoneal organ, is near the C loop of the duodenum laterally and the lesser sac anteriorly. This explains why a pseudoaneurysm can erode and bleed into the bowel, biliary tree, retroperitoneum, or peritoneal cavity.
Pathophysiology
Pseudoaneurysms form when enzyme-rich peripancreatic fluid, often within a pseudocyst, leads to autodigestion and weakening of the walls of adjacent arteries.
These arteries then undergo aneurysmal dilatation, with the aneurysmal bulge most often contained within the pseudocyst. At this point, the dilated region is correctly termed an aneurysm rather than a pseudoaneurysm, because the blood is still contained within the complete, albeit thinned, arterial wall. Rupture of the aneurysm into the pseudocyst converts the pseudocyst into a pseudoaneurysm (defined as extravascular hematoma communicating with the intravascular space).
In some instances, a pseudocyst can erode into a nearby artery, causing the conversion of the pseudocyst into a pseudoaneurysm.
Despite these distinctions, all of these forms are generally classified as pseudoaneurysms, because the end result is the formation of a total or partial vascular cystic structure.
Classification
Pang et al proposed a management-based classification system for peripancreatic pseudoaneurysms that is based on the following three elements [8] :
-
Type of artery from which the pseudoaneurysm arises
-
Presence or absence of communication with the gastrointestinal (GI) tract
-
Presence or absence of a high concentration of pancreatic juice at the bleeding site
In this system, originating artery type is specified as follows:
-
Type I - Pseudoaneurysm arises from a minor artery but must be at least 5 mm away from its junction of origin from a type II or III artery
-
Type II - Aneurysm arises from a major artery that may be sacrificed without physiologic consequences (eg, the splenic and gastroduodenal arteries)
-
Type III - Aneurysm arises from a major artery that cannot be sacrificed without significant consequences for the patient (eg, the superior mesenteric artery or the hepatic artery proper)
GI tract communication is specified as follows:
-
Type A - No communication with the GI tract
-
Type B - Communication with the GI tract
Exposure to pancreatic juice is specified as follows:
-
Type 1 - No exposure to pancreatic juice
-
Type 2 - Exposure to pancreatic juice
Etiology
Moderate-to-severe pancreatitis with or without pseudocyst or abscess is the major etiologic factor for pseudoaneurysm formation. [9] However, a visceral pseudoaneurysm may develop as a sequela of blunt and penetrating abdominal trauma. [10]
Pseudoaneurysm formation may also occur after biliopancreatic resection for cancer. [11, 12] Patients who have an anastomotic leak and develop an intra-abdominal abscess may subsequently be prone to delayed arterial hemorrhage. Focal sepsis erodes through vessels and causes pseudoaneurysm formation and delayed rupture and bleeding.
Pancreatic transplantation is another, occasionally reported cause of pancreatic pseudoaneurysm formation. [13, 14, 15]
Prognosis
Patients treated with supportive measures have a mortality in excess of 90%. Mortality following surgical treatment of arterial hemorrhage of pancreatic origin is in the range of 28-56%.; it depends primarily on the anatomic location of the pseudoaneurysm, not on the surgical method used. [16]
Surgical intervention for treatment of pseudoaneurysm in the head of the pancreas has a 43% mortality, whereas surgery for a pseudoaneurysm in the body or tail of the pancreas has a mortality of 16%. (Pseudoaneurysms in the head of the pancreas necessitate a Whipple procedure, which likely contributes to the higher mortality.) Mortality for patients who suffer postoperative hemorrhage is in the range of 50-60%.
Embolotherapy has a high initial success rate (90-100%), though some reports indicate a recurrence rate of 37% and an overall mortality of 16%. Embolotherapy is the preferred initial therapy for bleeding originating from the head of the pancreas.
-
Splenic artery angiogram demonstrating contrast (white arrow) extravasating into a pseudoaneurysm (black arrow).
-
A CT scan with intravenous contrast enhancement (arrow) within a pancreatic pseudocyst indicating the presence of a pseudoaneurysm.
-
Preembolization angiogram depicting a splenic artery pseudoaneurysm.
-
Postembolization angiogram depicting successful coil embolization of a pseudoaneurysm.