Practice Essentials
Gastric outlet obstruction (GOO, also known as pyloric obstruction) is not a single entity; it is the clinical and pathophysiological consequence of any disease process that produces a mechanical impediment to gastric emptying.
Clinical entities that can result in GOO generally are categorized into two well-defined groups of causes: benign and malignant. This classification facilitates discussion of management and treatment. In the past, when peptic ulcer disease (PUD) was more prevalent, benign causes were the most common; however, one review showed that only 37% of patients with GOO have benign disease and the remaining patients have obstruction secondary to malignancy. [1]
Gastric outlet obstruction can be a diagnostic and treatment dilemma. Despite medical advances in the acid suppression mechanism, the incidence of GOO remains a prevalent clinical problem in benign PUD. Also, an increase in the number of cases of GOO seems to be noted secondary to malignancy; this is possibly due to improvements in cancer therapy, which allow patients to live long enough to develop this complication.
As part of the initial workup, exclude the possibility of functional nonmechanical causes of obstruction, such as diabetic gastroparesis. Once a mechanical obstruction is confirmed, differentiate between benign and malignant processes because definitive treatment is based on recognition of the specific underlying cause.
Carry out diagnosis and treatment expeditiously, because delay may result in further compromise of the patient's nutritional status. Delay will also further compromise edematous tissue and complicate surgical intervention.
Orient initial management to identification of the primary underlying cause and to the correction of volume and electrolyte abnormalities. Barium swallow studies and upper endoscopy are the main tests used to help make the diagnosis. Tailor treatment to the specific cause. If medical therapy conducted for a reasonable period fails to alleviate the obstruction, then surgical intervention becomes appropriate. Typically, if resolution or improvement is not seen within 48-72 hours, surgical intervention is necessary. The choice of surgical procedure depends upon the patient's particular circumstances. Increasingly, endoscopic approaches are employed in the treatment of GOO. [2]
Anatomy
The stomach is located mainly in the left upper quadrant beneath the diaphragm and is attached superiorly to the esophagus and distally to the duodenum. The stomach is divided into four portions: cardia, body, antrum, and pylorus. Inflammation, scarring, or infiltration of the antrum and pylorus are associated with the development of GOO.
The duodenum begins immediately beyond the pylorus and mostly is a retroperitoneal structure, wrapping around the head of the pancreas. The duodenum classically is divided into four portions. It is intimately related to the gallbladder, liver, and pancreas; therefore, a malignant process of any adjacent structure may cause outlet obstruction due to extrinsic compression.
Pathophysiology
Intrinsic or extrinsic obstruction of the pyloric channel or duodenum is the usual pathophysiology of GOO; the mechanism of obstruction depends upon the underlying etiology.
Patients present with intermittent symptoms that progress until obstruction is complete. Vomiting is the cardinal symptom. Initially, patients may demonstrate better tolerance to liquids than solid food. In a later stage, patients may develop significant weight loss due to poor caloric intake. Malnutrition is a late sign, but it may be very profound in patients with concomitant malignancy. In the acute or chronic phase of obstruction, continuous vomiting may lead to dehydration and electrolyte abnormalities.
When obstruction persists, patients may develop significant and progressive gastric dilatation. The stomach eventually loses its contractility. Undigested food accumulates and may represent a constant risk for aspiration pneumonia.
Etiology
The major benign causes of GOO are PUD, gastric polyps, ingestion of caustics, pyloric stenosis, congenital duodenal webs, gallstone obstruction (Bouveret syndrome), pancreatic pseudocysts, and bezoars.
PUD manifests in approximately 5% of all patients with GOO. Ulcers within the pyloric channel and first portion of the duodenum usually are responsible for outlet obstruction. Obstruction can occur in an acute setting secondary to acute inflammation and edema or, more commonly, in a chronic setting secondary to scarring and fibrosis. Helicobacter pylori has been implicated as a frequent associated finding in patients with GOO, but its exact incidence has not been defined precisely.
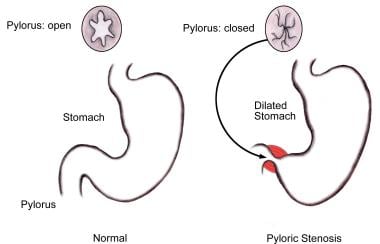
Within the pediatric population, pyloric stenosis constitutes the most important cause of GOO. Pyloric stenosis occurs in 1 per 750 births. It is more common in boys than in girls and also is more common in first-born children. Pyloric stenosis is the result of gradual hypertrophy of the circular smooth muscle of the pylorus. (See image below.)
Pancreatic cancer is the most common malignancy causing GOO. Outlet obstruction may occur in 10-20% of patients with pancreatic carcinoma. Other tumors that may obstruct the gastric outlet include ampullary cancer, duodenal cancer, cholangiocarcinomas, and gastric cancer. Metastases to the gastric outlet also may be caused by other primary tumors.
Epidemiology
The incidence of GOO has been reported to be less than 5% in patients with PUD, which is the leading benign cause of the problem. Five percent to 8% of ulcer-related complications result in an estimated 2000 operations per year in the United States. [3]
The incidence of GOO in patients with peripancreatic malignancy, the most common malignant etiology, has been reported as 15-20%.
-
Upper endoscopy showing multiple gastric polyps. Such polyps are a major cause of gastric outlet obstruction.
-
Anatomic changes associated with pyloric stenosis.
-
Plain radiograph of the abdomen. Enlarged stomach with calcified content.
-
Contrast study demonstrating an enlarged stomach. The point of obstruction is visualized at the pyloric-duodenal junction (string sign).
-
Completed myotomy in open pyloromyotomy for hypertropic pylotic stenosis.
-
Robotic-assisted esophagectomy pyloroplasty. Courtesy of Memorial Sloan-Kettering Cancer Center, featuring Inderpal S. Sarkaria, MD.