Background
Injuries to major abdominal vessels are uncommon but highly lethal vascular crises. Predictably, exsanguinating hemorrhage is the most important cause of early death. Intra-abdominal vascular injuries are associated with extremely rapid rates of blood loss and pose challenges of exposure during celiotomy, [1, 2, 3] given the posterior position of the major abdominal vascular structures (except for the portal vein and the hepatic artery).
Essential to the successful management of these injuries is a thorough knowledge of intra-abdominal vascular anatomy and a familiarity with the techniques of proximal and distal control combined with selective application of primary repair, bypass, or ligation as indicated.
See the following for more information:
Anatomy
The following anatomic locations should be distinguished:
-
Midline supramesocolic hemorrhage or hematoma (superior to the transverse mesocolon) is usually caused by injury to the suprarenal aorta, the celiac axis, the proximal superior mesenteric artery (SMA), or the proximal renal artery.
-
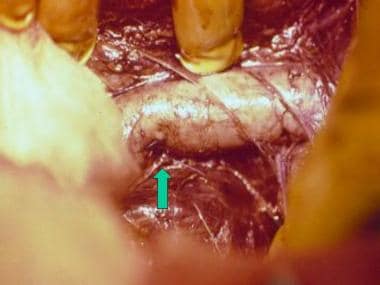
Midline inframesocolic hemorrhage or hematoma results from infrarenal aorta or inferior vena cava (IVC) injury (see the image below).
-
Lateral perirenal hematoma or hemorrhage suggests injury to the renal vessels or kidneys.
-
Lateral pelvic hematoma or hemorrhage indicates injury to the iliac artery, the iliac vein, or both.
Pathophysiology
In blunt trauma, rapid deceleration during a motor vehicle accident (MVA) results in an avulsion of the small branches of major vessels (eg, mesenteric tear). Another mechanism of injury is related to a direct crush or blow to the major vessels, resulting in an intimal tear with thrombosis or vessel rupture and hemorrhage.
Penetrating injuries directly disrupt the vessel wall or create intimal flaps secondary to the blast effect. Because of the anatomical position of the major vascular structures in the abdomen, injuries to these vessels have a high probability of association with other major injuries in the abdomen, particularly to the small bowel.
Hemorrhagic shock from intra-abdominal hemorrhage often leads to metabolic acidosis accompanied by coagulopathy and hypothermia—the so-called lethal triad of trauma. The use of systolic blood pressure at any predefined cutoff value when considered out of context with other potential indicators of shock is neither particularly specific, nor sufficiently sensitive, to be useful clinically for the diagnosis of shock. In contrast, the shock index (ie, heart rate divided by systolic blood pressure) may suggest compensated shock when either heart rate or blood pressure considered separately do not. Metabolic acidosis in trauma patients is the result of lactate overproduction, most often from decreased oxygen delivery as a result of hypovolemic shock.
Acidosis adds to the overall lethality of preexisting injury primarily by depression of myocardial contractility and by impairment of coagulation. Furthermore, hypothermia (below 34°C) inhibits platelet function and slows coagulation factor activation. This self-perpetuating cycle is responsible for 80% of deaths in patients with major vascular injury and must be rapidly corrected to prevent a dismal outcome.
Patients also present in a hyperfibrinolytic state, which exacerbates the coagulopathy associated with the lethal triad of trauma. [4]
Epidemiology
The incidence of abdominal vascular injuries in military conflicts is surprisingly low: generally less than 5% of all vascular injuries. In contrast, approximately 30% of all vascular injuries observed in civilians occur in the abdomen. This striking difference between combat and noncombat vascular trauma can be attributed to the low energy of missiles from civilian handguns and the short prehospital transit times in urban settings, which make it more likely that a civilian with penetrating abdominal vascular injury will survive long enough to reach surgical care.
The incidence of abdominal vessel injury in patients with blunt trauma is estimated at approximately 5-10%. A similar incidence of 10.3% is reported in patients with penetrating stab wounds to the abdomen. Patients with gunshot wounds (GSWs) to the abdomen will have major vessel injury in 20-25% of cases. In an analysis of a registry of 2949 European patients with abdominal trauma, Barbati et al reported that the leading cause of abdominal vascular injuries was traffic accidents, followed by falls from heights. [5]
Prognosis
Mortality
Mortality rates for abdominal vascular trauma vary depending on the vessel or vessels injured, as follows:
-
Suprarenal aorta - 60%
-
SMA - 40-80%
-
Superior mesenteric vein (SMV) - 20%
-
Combined injury to the suprarenal aorta and IVC – 100%
-
Infrarenal abdominal aorta - 50%
-
Infrarenal vena cava - 30%
-
Renal artery - 15%
-
Iliac artery - 40%
-
Iliac vein - 30%
Complications
Early complications of abdominal vascular injuries include ongoing bleeding, coagulopathy, and abdominal compartment syndrome. Late complications include, but are not limited to, intra-abdominal infections, wound dehiscence, acute respiratory distress syndrome (ARDS), and pneumonia.
-
Abdominal vascular injuries. Tangential gunshot injury to the inferior vena cava repaired by means of lateral venorrhaphy (arrow).