Practice Essentials
Anaplastic carcinoma of the thyroid (ATC) is the most aggressive thyroid gland malignancy. Although ATC accounts for less than 2% of all thyroid cancers, it causes up to 40% of deaths from thyroid cancer. The aggressive nature of ATC makes treatment studies difficult to perform. The overall 5-year survival rate is reportedly less than 10%, and most patients do not live longer than a few months after diagnosis.
See the figure below.
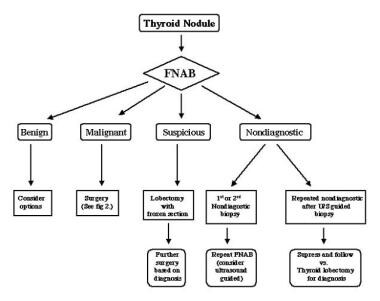 Algorithm for the management of a solitary thyroid nodule. FNAB = fine needle aspiration biopsy; US = ultrasonography.
Algorithm for the management of a solitary thyroid nodule. FNAB = fine needle aspiration biopsy; US = ultrasonography.
Patients with ATC typically present with a rapidly growing neck mass. Metastases, particularly in the lung, are likely to be present at diagnosis more than 50% of the time. Treatment is mostly palliative. Surgical resection with adjuvant radiation therapy and chemotherapy may prolong survival somewhat and improve quality of life.
For patient education resources, see the Endocrine System Center, as well as Thyroid Problems.
Pathophysiology
Anaplastic carcinoma of the thyroid (ATC) generally occurs in people in iodine-deficient areas and in a setting of previous thyroid pathology (eg, pre-existing goiter, follicular thyroid cancer, papillary thyroid cancer). Local invasion of adjacent structures (eg, trachea, esophagus) commonly occurs.
The Global Anaplastic Thyroid Cancer Initiative (GATCI) studied the mutational landscape of 329 thyroid cancer regions from 292 patients, including 213 regions from patients with ATC and 115 regions from patients with papillary thyroid cancer. The GATCI demonstrated that ATC arises in the context of differentiated thyroid cancers but acquires additional characteristic clonal driver mutations. Sequencing studies showed that ATCs have a higher burden of mutations than other thyroid cancers, with distinct mutational signatures and molecular subtypes. In addition to genes commonly altered in cancer or previously linked to ATC, such as BRAF, RAS, TP53, PIK3CA, BRCA1, BRCA2, and USH2A, the GACTI identified tens of novel alterations enriched in ATC, including recurrent non-synonymous single-nucleotide variants in the pathways related to MAPK signaling, DNA damage repair, cell division, and cell adhesion. [1]
ATC has a genetic association with oncogenes C-myc, H-ras, and Nm23. Mutations in genes that code for BRAF, RAS, catenin (cadherin-associated protein), beta 1, PIK3CA, TP53, AXIN1, PTEN, and APC have been found in ATC, and chromosomal abnormalities are common. [2, 3] TJonker and collegues performed functional genomic RNA profiling on 25 ATCs and 80 normal thyroid samples and identified 301 significantly upregulated genes, of which the following were seen as potential therapeutic targets [4] :
-
MTOR
-
MET
-
WEE1
-
PSMD1
-
MERTK
-
FGFR3
-
RARG
-
ESR2
Epidemiology
Anaplastic carcinoma of the thyroid (ATC) constitutes less than 2% of all thyroid malignancies in the United States, which equates to slightly more than 1000 new cases annually. [5, 6] Fortunately, the incidence of thyroid cancer appears to be declining. Worldwide frequency likely approximates that in the United States.
Although papillary thyroid cancer shows a strong female predominance, with a female-to-male ratio of approximately 3:1, ATC affects females and males relatively equally. [1] Peak incidence occurs during the sixth to seventh decades of life. The age range of affected patients reportedly is 15-90 years.
Although ATC remains deadly, in recent years the prognosis for patients with ATC appears to have improved. A review of the Surveillance, Epidemiology, and End Results (SEER) database found that estimated 1-year survival rose from 15% for patients diagnosed from 2011 to 2016, to 25% for patients diagnosed from 2017 to 2020. [7]
Prognosis
ATC has a rapidly progressive course and early dissemination. In 80%-90% of patients, the disease has already spread beyond the thyroid gland at presentation. [5] The most common sites of distant spread include, in descending order, the lung, bone, and brain. Metastases, particularly in the lung, are likely to be present at diagnosis in more than 50% of cases. The overall 5-year survival rate is reportedly less than 10%, and most patients do not live longer than a few months after diagnosis. [8]
One study has shown that patients younger than 60 years who have ATC confined to the thyroid have a better prognosis than patients who are older and have distant metastases. [9] A retrospective study from Korea found that age less than 60 years, tumor size less than 7 cm, and lesser extent of disease were independent predictors of lower disease-specific mortality. [10]
While some studies have suggested that postoperative radiotherapy may be of benefit in terms of survival, definitive prospective trials are lacking.
Akaishi et al conducted a review of 100 patients with ATC in a single hospital (Ito Hospital) from 1993-2009. [11] The 1-year survival rates were as follows:
-
Stage IVA - 72.7%
-
Stable IVB- 24.8%
-
Stable IVC - 8.2%
Multivariate analysis demonstrated worse prognosis with age older than 70 years, white blood cell count of 10,000/μL or more, extrathyroidal invasion, and distant metastases at the time of diagnosis. Survival was significantly better if the patient received complete resection, external radiation at doses of 40 Gy or more, or both. [11]
Orita et al developed a prognostic index that can predict prognosis and assist in the early treatment of ATC. [12]
-
Algorithm for the management of a solitary thyroid nodule. FNAB = fine needle aspiration biopsy; US = ultrasonography.









