Practice Essentials
Malignant carcinoid syndrome is characterized by an array of signs and symptoms—in particular, hot, red flushing of the face; severe and debilitating diarrhea; and asthma attacks—caused by vasoactive hormones secreted by metastases from carcinoid tumors. [1, 2, 3] Carcinoid tumors are of neuroendocrine origin and derive from primitive stem cells, which can give rise to multiple cell lineages. Malignant carcinoid syndrome occurs in fewer than 10% of patients with a carcinoid tumor.
Carcinoid tumors arise from neuroendocrine cells, which are widespread in the human body, especially in the organs derived from the primitive intestine (see the image below). Carcinoid tumors and related syndromes may be a part of multiple endocrine neoplasia.
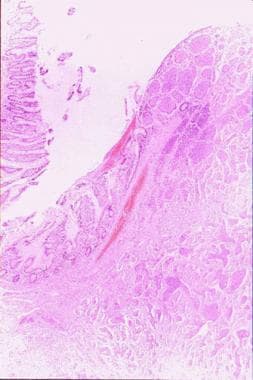 A section (on the right) of an intestinal carcinoid mass arising from the mucosa (150 X). Image courtesy of Professor Pantaleo Bufo, University of Foggia, Italy.
A section (on the right) of an intestinal carcinoid mass arising from the mucosa (150 X). Image courtesy of Professor Pantaleo Bufo, University of Foggia, Italy.
These intensely vascularized tumors follow the so-called rule of one third, which states as follows:
-
One third of these tumors are multiple
-
One third of those in the gastrointestinal (GI) tract are located in the small bowel
-
One third of patients have a second malignancy
-
One third of these tumors metastasize
Typically, 90% of carcinoid tumors originate from the distal ileum or appendix (the embryologic midgut. [4] ) Carcinoid tumors represent 90% of appendiceal tumors.
Tumors arising from the foregut and hindgut are considered atypical; however, tumors can originate from any cell of the amine precursor uptake and decarboxylation system and, therefore, produce several intestinal hormones. Most of these tumors produce 5-hydroxytryptamine, which, in physiologic conditions, is taken up and stored in the platelets while the excesses are inactivated in the liver and lung and transformed into 5-hydroxyindoleacetic acid (5-HIAA).
In order of frequency, carcinoids may occur in the appendix (35%), ileum (28%), rectum (13%), and bronchi (13%). Incidence is less than 1% in the pancreas, gallbladder, liver, larynx, testes, and ovaries; however, tumors in these locations frequently metastasize and spread through the mesenteric lymph nodes (see image below) and portal vein. After spreading to the liver, carcinoids can metastasize to the lungs, [5] bone, skin, or almost any organ.
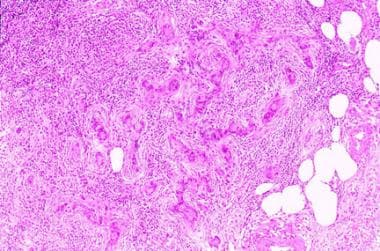 A section of a rare lymph node metastasis from adenocarcinoid tumor (250 X). Image courtesy of Professor Pantaleo Bufo, University of Foggia, Italy.
A section of a rare lymph node metastasis from adenocarcinoid tumor (250 X). Image courtesy of Professor Pantaleo Bufo, University of Foggia, Italy.
Carcinoids do not produce the malignant carcinoid syndrome until they are no longer confined to the small bowel or mesentery, perhaps because the liver breaks down the secretory products of tumors restricted to those locations. Ovarian carcinoids may be considered exceptions; a patient with ovarian teratomas, whose secretory products enter into the systemic circulation, may present with this syndrome without liver metastasis. [6, 7]
Diagnosis of carcinoid syndrome
If a patient is thought to have carcinoid syndrome, blood and urine tests must be performed to determine levels of bioactive substances secreted by carcinoid tumors. Bochemical diagnosis of carcinoid tumors is based on the measurement of the serotonin metabolite 5-HIAA in urine. Follow-up assays of other bioactive substances vary according to the location of the carcinoid tumor. See Workup.
Imaging studies also must be performed to detect the sites of either primary tumors or metastases. Recommended studies include multiphasic CT and MRI. Scintigraphy with indium-111 diethylenetriamine pentaacetic acid (DTPA) octreotide (In-111 DTPA Octr), or OctreoScan, localizes the primary carcinoid and eventual recurrences, as well as other neuroendocrine tumors, with high sensitivity and specificity. T
Treatment of carcinoid syndrome
Complete surgical removal of all tumor tissues, when feasible, is the best treatment. Systemic therapy should be used to control humorally mediated symptoms when the cancer spreads elsewhere. The somatostatin analogs (SSAs) octreotide and lanreotide are used to control carcinoid symptoms and tumor progression in advanced inoperable disease. Patients with diarrhea that is not controlled with somatostatin analog therapy can be treated with telostristat ethyl, a tryptophan hydroxylase inhibitor. Other options for second-line therapy include dose escalation of SSAs, interferon alpha, everolimus, radionuclide therapy, and liver-directed therapies. [8] See Treatment and Medication.
For patient education information, see Carcinoid Syndrome.
Background
In 1888 Lubarsch first described a carcinoid tumor, [9] but Oberndorfer called a group of small, benign-appearing tumors karzinoide tumoren (carcinoid) for the first time in 1907. [10]
The name was chosen to separate these tumors from ordinary malignancies (carcinomas), but by the 1950s, the fact that carcinoids could be malignant was obvious, thanks to Erspamer and Asero (1952), who identified serotonin production by carcinoid tumors. [11] This finding, built on research conducted in the first half of the 20th century, is summarized as follows:
-
In 1914, Gosset and Masson demonstrated that carcinoid tumors might arise from enterochromaffin cells (Kulchitsky cells) within glands of Lieberkühn using silver impregnation techniques. [12]
-
In 1928, Masson established characterization of carcinoids as argentaffin cell tumors. [13]
-
In 1980, the World Health Organization (WHO) applied the term carcinoid to all tumors of the diffuse endocrine system (synonymous with amine precursor uptake and decarboxylation [APUD] and neuroendocrine cell system).
Pathophysiology
Pathophysiology is closely related to the sites of the primary tumors. When these tumors spread to the liver, patients usually begin to develop malignant carcinoid syndrome. In fact, this syndrome develops when vasoactive substances produced by a carcinoid tumor escape hepatic degradation and gain access to the systemic circulation.
Carcinoids arising in the stomach are usually associated with low gastric acid production, a condition termed hypochlorhydria or achlorhydria. These tumors rarely become malignant and never metastasize, but they sometimes produce histamine.
Carcinoid tumors arising in the lung generally produce serotonin, gastrin, adrenocorticotropic hormone (ACTH), and histamine. Carcinoids that develop outside the appendix are often malignant, while tumors developing in the appendix are usually benign if smaller than 2 cm in diameter. Rectal carcinoid tumors often produce polypeptides (PPs), polypeptide Y, neuropeptide Y, and other peptides, but none of the patients with this disease location have symptoms related to the production of such molecules. Few patients have liver metastases, but if they do have liver metastases, they do not have hormone-related symptoms.
Physiologically, serotonin causes vasodilation and can increase blood clotting by stimulating platelet aggregation, which may result in disseminated intravascular coagulation (DIC); however, serotonin is converted to 5-HIAA in the body. To date, it is well known that the carcinoids also may produce PPs and amines:
-
Acid phosphatase
-
α-glycoprotein
-
α1-antitrypsin
-
Amylin
-
Atrial natriuretic polypeptide
-
Calbindin-D28k
-
Catecholamines
-
Chromogranin A and B (CgA/CgB)
-
Dopamine
-
Fibroblast growth factor (FGF)
-
Gastrin
-
Gastrin-releasing peptide (bombesin)
-
Glucagon/glicentin
-
5-Hydroxyindoleacetic acid (5-HIAA)
-
5-Hydroxytryptamine (5-HT)
-
Histamine
-
Insulin
-
Kallikrein
-
Motilin
-
Neuron-specific enolase (NSE)
-
A-Neuropeptide
-
K-Neuropeptide
-
Neurotensin
-
Pancreastatin
-
Pancreatic polypeptide
-
Platelet-dermal growth factor (PDGF)
-
Prostaglandins
-
Pyroglutamyl-glutamyl-prolinamide
-
Secretin
-
Serotonin
-
Somatostatin
-
Substance P
-
Somatotropin release-inhibiting factor (SRIF)
-
Tachykinins
-
β-transforming growth factor (β-TGF)
-
Vasoactive intestinal polypeptide (VIP)
The molecules listed above are responsible for the extreme symptoms of this condition. For example, the reason some patients develop heart disease is not definitively known, [14] but the serotonin produced by the tumor is probably involved. Bronchial constriction, which accounts for the asthmalike attacks, seems related to the tumoral tachykinins. Carcinoid diarrhea has been correlated with circulating tachykinins. [15]
Symptoms may also relate to overproduction of PPs in the pro-opiomelanocortin family (eg, endorphin, enkephalin). Frequently, the enteric blood supply is impaired, which is caused by the desmoplastic reaction of mesenteric peritoneum and determines kinking and angulation of the loops of the small bowel, with result in bowel obstruction.
Serotonin is derived from the amino acid tryptophan, which also serves as a precursor to niacin and several proteins. Increased metabolism of tryptophan by the tumor has been linked to symptoms in patients with carcinoid. [16]
The main clinical characteristics of the carcinoids arising in the digestive tract that most often cause malignant carcinoid syndrome are as follows:
Gastric carcinoid tumors are sporadic in 15-25% of cases, usually solitary and larger than 1 cm, arising in normal-appearing mucosa from enterochromaffin-like cells in the gastric fundus. These tumors are generally located in the body or fundus of the stomach and identified endoscopically. A large number of patients have metastases at the time of presentation, and over 50% have pernicious anemia. Gastric carcinoid tumors are more common in women during their sixth or seventh decade of life. It may be associated with atypical carcinoid syndrome manifested by flushing and mediated by histamine.
Carcinoid tumors of the small bowel arise from intraepithelial endocrine cells producing 5-HT and account for one third or fewer of small-bowel tumors. Often located in the distal ileum, these tumors are frequently multicentric, and most patients present with metastases to the lymph nodes or liver. Although tumor size is an unreliable predictor of metastatic disease, the 5-year survival rate closely correlates with the stage of disease at presentation (35% of patients survive if one or more distant metastases are present; 65% for localized or regional disease). Patients usually present in the sixth or seventh decade of life, and 5-7% present with carcinoid syndrome.
Appendiceal carcinoids are the most common cancers of the appendix and arise from the subepithelial endocrine cells from the lamina propria and submucosa. In 75% of cases, appendiceal carcinoids are located at the tip. Fewer than 10% of appendiceal carcinoids are located at the base. Appendiceal carcinoids are most frequently diagnosed in women in the fourth or fifth decade of life, and 10% or more are symptomatic. Patients may often be misdiagnosed as having appendicitis. The tumor size is the best prognostic predictor, with a 5-year survival rate of 94% for patients with local disease, 85% if there are regional metastases, and 34% if the patient has one or more distal metastases. It is noteworthy that more than 95% of appendiceal carcinoids are 2 cm or less, with rare metastases, while one third of tumors 2 cm or larger have either nodal or distant metastases. Carcinoid syndrome has been reported in patients with liver metastases.
Carcinoid tumors of the colon account for 1% or fewer of colon tumors and usually arise from serotonin-producing epithelial endocrine cells present in the colon mucosa. Most of the affected patients are in the seventh decade of life and present with abdominal pain, anorexia, and weight loss. At the time of diagnosis, the average tumor diameter is approximately 5 cm, and more than two thirds of patients have either nodal or distant disease. The 5-year survival rate is reported to be near 70% for local disease, 44% if regional metastases exist, and 20% in cases with distant metastases. The 5% of patients with metastatic disease show a malignant carcinoid syndrome.
Rectal carcinoid tumors are responsible for up to 2% of all rectal tumors. The disease usually affects persons in the sixth decade of life and most commonly presents as rectal bleeding, pain, or constipation, while 50% of patients are asymptomatic, with tumors found during routine endoscopy. Generally, the tumor cells contain glucagon and glicentin-related peptides rather than serotonin. The 5-year survival rate is 81% with local disease, 47% for regional disease, and 18% for distant metastases. Note that patients rarely present with carcinoid syndrome, and the syndrome is closely related to tumor size.
Etiology
As with many other cancers, the exact cause is unknown. Malignant carcinoid syndrome does not generally appear to be hereditary.
A study of genetic alterations in small bowel carcinoid tumors found that loss of all or most of chromosome 18 was the most common finding. Heterozygosity was also lost on chromosome arms 9p and 16q. Although the amplitude of observed gains was modest in comparison with those reported in some other tumor types, one focal region of recurrent gain on 14q mapped to the locus of the gene encoding the antiapoptotic protein DAD1. [17]
Epidemiology
Frequency
United States
The incidence of clinical carcinoid tumors is estimated to be 1.5-1.9 cases per 100,000 population; the actual frequency is almost certainly higher, because many carcinoid tumors never produce the related syndrome. It is estimated that about 8,000 gastrointestinal (GI) tract–related carcinoid tumors are diagnosed each year in the United States. [18]
International
Epidemiologic studies have reported incidences of carcinoid tumors ranging from 0.79 to 1.88 per 100,000 population; a study from the Netherlands found an incidence of 1.95 per 100,000 population. [19] These numbers are probably underestimates, because a large number of affected individuals do not develop the related syndrome. A Swedish autopsy study reported an incidence of 8.4 cases per 100,000 population. [20] Carcinoid tumors are discovered in approximately 1-2 appendectomy cases per 200-300 per year.
Mortality/morbidity
Tumors that are smaller than 1 cm in diameter rarely metastasize, while lesions larger than 2 cm often metastasize. The presence of a few small metastases to the liver is associated with a longer life expectancy. Morbidity is related to vasoactive amine production. The survival rate usually correlates inversely with the levels of daily urinary 5-HIAA excretion. Death is usually caused by cardiac or hepatic failure and by complications associated with tumor growth. Factors associated with higher mortality are high plasma levels of neuropeptide K and chromogranin A, location of the tumor in the large bowel, advanced disease, and a concomitant second malignancy. Mucus-producing tumors developing in the appendix also have some malignant characteristics.
Sex- and age-related demographics
Carcinoid syndrome affects men and women equally. Carcinoids occur most frequently in patients aged 50-70 years. Age at diagnosis ranges from 10-93 years (mean age 55 y). No racial prevalence is known.
-
A section (on the right) of an intestinal carcinoid mass arising from the mucosa (150 X). Image courtesy of Professor Pantaleo Bufo, University of Foggia, Italy.
-
A section of a carcinoid mass (350 X). Image courtesy of Professor Pantaleo Bufo, University of Foggia, Italy.
-
A section of a rare lymph node metastasis from adenocarcinoid tumor (250 X). Image courtesy of Professor Pantaleo Bufo, University of Foggia, Italy.







