Background
The ancient Egyptians were the first civilization to have trained clinicians to treat physical aliments. Medical papyri, such as the Edwin Smith papyrus (circa 1600 BCE) and the Ebers papyrus (circa 1534 BCE), provided detailed information of management of disease, including wound management with the application of various potions and grease to assist healing. [1, 2]
See 5 Body Modifications and Piercing: Dermatologic Risks and Adverse Reactions, a Critical Images slideshow, to help recognize various body modifications and the related potential complications.
Hippocrates (Greek physician and surgeon, 460-377 BCE), known as the father of medicine, used vinegar to irrigate open wounds and wrapped dressings around wounds to prevent further injury. His teachings remained unchallenged for centuries.
Galen (Greek surgeon to Roman gladiators, 130-200 CE) was the first to recognize that pus from wounds inflicted by the gladiators heralded healing (pus bonum et laudabile ["good and commendable pus"]).
Unfortunately, Galen's observation was misinterpreted, and the concept of pus preempting wound healing persevered well into the 18th century. The link between pus formation and healing was emphasized so strongly that foreign material was introduced into wounds to promote pus formation-suppuration. The concept of wound healing remained a mystery, as highlighted by the famous saying by Ambroise Paré (French military surgeon, 1510-1590), "I dressed the wound. God healed it." [3]
The scale of wound infections was most evident in times of war. During the American Civil War, erysipelas (necrotizing infection of soft tissue) and tetanus accounted for over 17,000 deaths, according to an anonymous source in 1883. Because compound fractures at the time almost invariably were associated with infection, amputation was the only option, despite a 25-90% risk of amputation stump infection.
Koch (Professor of Hygiene and Microbiology, Berlin, 1843-1910) first recognized the cause of infective foci as secondary to microbial growth in his 19th century postulates. Semmelweis (Austrian obstetrician, 1818-1865) demonstrated a fivefold reduction in puerperal sepsis by hand washing between performing postmortem examinations and entering the delivery room.
Joseph Lister (Professor of Surgery, London, 1827-1912) and Louis Pasteur (French bacteriologist, 1822-1895) revolutionized the entire concept of wound infection. Lister recognized that antisepsis could prevent infection. [4] In 1867, he placed carbolic acid into open fractures to sterilize the wound and to prevent sepsis and hence the need for amputation. In 1871, Lister began to use carbolic spray in the operating room to reduce contamination. However, the concept of wound suppuration persevered even among eminent surgeons such as John Hunter. [5]
World War I resulted in new types of wounds from high-velocity bullet and shrapnel injuries coupled with contamination by the mud from the trenches. Antoine Depage (Belgian military surgeon, 1862-1925) reintroduced wound debridement and delayed wound closure and relied on microbiological assessment of wound brushings as guidance for the timing of secondary wound closure. [6] Alexander Fleming (microbiologist, London, 1881-1955) performed many of his bacteriologic studies during World War I and is credited with the discovery of penicillin.
As late as the 19th century, aseptic surgery was not routine practice. Sterilization of instruments began in the 1880s as did the wearing of gowns, masks, and gloves. Halsted (Professor of Surgery, Johns Hopkins University, United States, 1852-1922) introduced rubber gloves to his scrub nurse (and future wife) because she was developing skin irritation from the chemicals used to disinfect instruments. The routine use of gloves was introduced by Bloodgood, a student of Halsted.
Penicillin first was used clinically in 1940 by Howard Florey. With the use of antibiotics, a new era in the management of wound infections commenced. Unfortunately, eradication of the infective plague affecting surgical wounds has not ended because of the insurgence of antibiotic-resistant bacterial strains and the nature of more adventurous surgical intervention in immunocompromised patients and in implant surgery.
Pathophysiology
Wound healing is a continuum of complex interrelated biologic processes at the molecular level. For descriptive purposes, healing may be divided into the following three phases:
-
Inflammatory phase
-
Proliferative phase
-
Maturation phase
Inflammatory phase
The inflammatory phase commences as soon as tissue integrity is disrupted by injury; this begins the coagulation cascade to limit bleeding. Platelets are the first of the cellular components that aggregate to the wound, and, as a result of their degranulation (platelet reaction), they release several cytokines (or paracrine growth factors). These cytokines include platelet-derived growth factor (PDGF), insulinlike growth factor-1 (IGF-1), epidermal growth factor (EGF), and fibroblast growth factor (FGF).
Serotonin is also released, which, together with histamine (released by mast cells), induces a reversible opening of the junctions between the endothelial cells, allowing the passage of neutrophils and monocytes (which become macrophages) to the site of injury.
This large cellular movement to the injury site is induced by cytokines secreted by the platelets (chemotaxis) and by further chemotactic cytokines secreted by the macrophages themselves once at the site of injury. These include transforming growth factor alpha (TGF-α) and transforming growth factor beta (TGF-β).
Consequently, an inflammatory exudate that contains red blood cells, neutrophils, macrophages, and plasma proteins, including coagulation cascade proteins and fibrin strands, fills the wound in a matter of hours. Macrophages not only scavenge but they also are central to the wound healing process because of their cytokine secretion.
Proliferative phase
The proliferative phase begins as the cells that migrate to the site of injury, such as fibroblasts, epithelial cells, and vascular endothelial cells, start to proliferate and the cellularity of the wound increases. The cytokines involved in this phase include FGFs, particularly FGF-2 (previously known as basic FGF), which stimulates angiogenesis and epithelial cell and fibroblast proliferation.
The marginal basal cells at the edge of the wound migrate across the wound, and, within 48 hours, the entire wound is epithelialized. In the depth of the wound, the number of inflammatory cells decreases with the increase in stromal cells, such as fibroblasts and endothelial cells, which, in turn, continue to secrete cytokines. Cellular proliferation continues with the formation of extracellular matrix proteins, including collagen and new capillaries (angiogenesis). This process is variable in length and may last several weeks.
Maturation phase
In the maturation phase, the dominant feature is collagen. The dense bundle of fibers, characteristic of collagen, is the predominant constituent of the scar. Wound contraction occurs to some degree in primary closed wounds but is a pronounced feature in wounds left to close by secondary intention. The cells responsible for wound contraction are called myofibroblasts, which resemble fibroblasts but have cytoplasmic actin filaments responsible for contraction.
The wound continuously undergoes remodeling to try to achieve a state similar to that prior to injury. The wound has 70-80% of its original tensile strength at 3-4 months after operation.
Etiology
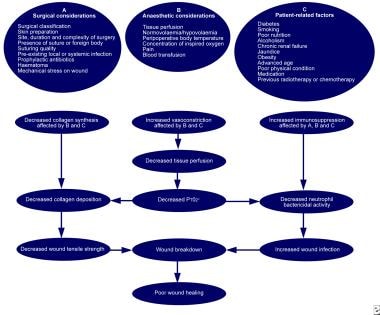
All surgical wounds are contaminated by microbes, but in most cases, infection does not develop because innate host defenses are quite efficient in the elimination of contaminants. A complex interplay between host, microbial, and surgical factors ultimately determines the prevention or establishment of a wound infection (see the image below).
Microbiology
Microbial factors that influence the establishment of a wound infection are the bacterial inoculum, virulence, and the effect of the microenvironment. When these microbial factors are conducive, impaired host defenses set the stage for enacting the chain of events that produce wound infection.
Most surgical-site infections (SSIs) are contaminated by the patient's own endogenous flora, which are present on the skin, mucous membranes, or hollow viscera. The traditional microbial concentration quoted as being highly associated with SSIs is that of bacterial counts higher than 10,000 organisms per gram of tissue (or in the case of burned sites, organisms per cm2 of wound). [7]
The usual pathogens on skin and mucosal surfaces are gram-positive cocci (notably staphylococci); however, gram-negative aerobes and anaerobic bacteria contaminate skin in the groin/perineal areas. The contaminating pathogens in gastrointestinal surgery are the multitude of intrinsic bowel flora, which include gram-negative bacilli (eg, Escherichia coli) and gram-positive microbes, including enterococci and anaerobic organisms. [8] (See Table 1 below.)
Table 1. Pathogens Commonly Associated with Wound Infections and Frequency of Occurrence [8] (Open Table in a new window)
Pathogen |
Frequency (%) |
Staphylococcus aureus |
20 |
Coagulase-negative staphylococci |
14 |
Enterococci |
12 |
Escherichia coli |
8 |
Pseudomonas aeruginosa |
8 |
Enterobacter species |
7 |
Proteus mirabilis |
3 |
Klebsiella pneumoniae |
3 |
Other streptococci |
3 |
Candida albicans |
3 |
Group D streptococci |
2 |
Other gram-positive aerobes |
2 |
Bacteroides fragilis |
2 |
Gram-positive organisms, particularly staphylococci and streptococci, account for most exogenous flora involved in SSIs. Sources of such pathogens include surgical/hospital personnel and intraoperative circumstances, including surgical instruments, articles brought into the operative field, and the operating room air.
The group of bacteria most commonly responsible for SSIs are Staphylococcus aureus strains. The emergence of resistant strains has considerably increased the burden of morbidity and mortality associated with wound infections.
Methicillin-resistant Staphylococcus aureus (MRSA) is proving to be the scourge of modern-day surgery. Like other strains of S aureus, MRSA can colonize the skin and body of an individual without causing sickness, and, in this way, it can be passed on to other individuals unknowingly. Problems arise in the treatment of overt infections with MRSA because antibiotic choice is very limited. MRSA infections appear to be increasing in frequency and are displaying resistance to a wider range of antibiotics. [9]
Of particular concern are the vancomycin intermediate S aureus (VISA) strains of MRSA. These strains are beginning to develop resistance to vancomycin, which is currently the most effective antibiotic against MRSA. This new resistance has arisen because another species of bacteria, called enterococci, relatively commonly express vancomycin resistance.
Risk factors (other than microbiology)
Decreased host resistance can be due to systemic factors affecting the patient's healing response, local wound characteristics, or operative characteristics, as follows:
-
Systemic factors - Age, malnutrition, hypovolemia, poor tissue perfusion, obesity, diabetes, steroids, and other immunosuppressants
-
Wound characteristics - Nonviable tissue in wound, hematoma, foreign material (eg, drains and sutures, dead space, poor skin preparation (eg, shaving), and preexistent sepsis (local or distant)
-
Operative characteristics - Poor surgical technique; lengthy operation (>2 hours); intraoperative contamination (eg, from infected theater staff and instruments or inadequate theater ventilation), prolonged preoperative stay in the hospital, and hypothermia
The type of procedure is a risk factor. Certain procedures are associated with a higher risk of wound contamination than others. Surgical wounds have been classified as clean, clean-contaminated, contaminated, and dirty-infected (see Table 2 below). [8, 10]
Table 2: Surgical Wound Classification and Subsequent Risk of Infection (If No Antibiotics Used) [8, 10] (Open Table in a new window)
Classification |
Description |
Infective Risk (%) |
Clean (Class I) |
Uninfected operative wound No acute inflammation Closed primarily Respiratory, gastrointestinal, biliary, and urinary tracts not entered No break in aseptic technique Closed drainage used if necessary |
< 2 |
Clean-contaminated (Class II) |
Elective entry into respiratory, biliary, gastrointestinal, urinary tracts and with minimal spillage No evidence of infection or major break in aseptic technique Example: appendectomy |
< 10 |
Contaminated (Class III) |
Nonpurulent inflammation present Gross spillage from gastrointestinal tract Penetrating traumatic wounds < 4 hours Major break in aseptic technique |
About 20 |
Dirty-infected (Class IV) |
Purulent inflammation present Preoperative perforation of viscera Penetrating traumatic wounds >4 hours |
About 40 |
Epidemiology
United States statistics
SSIs are not an extinct entity; they account for 14-16% of the estimated 2 million nosocomial infections affecting hospitalized patients in the United States. [11]
International statistics
Internationally, the frequency of SSI is difficult to monitor because criteria for diagnosis might not be standardized. A survey sponsored by the World Health Organization (WHO) demonstrated a prevalence of nosocomial infections in the range of 3-21%, with wound infections accounting for 5-34% of the total. [12]
The 2002 survey report by the Nosocomial Infection National Surveillance Service (NINSS; now the Surgical Site Infection Surveillance Service [SSISS]), [13] which covered the period between October 1997 and September 2001, indicated that the incidence of hospital-acquired infection related to surgical wounds in the United Kingdom was as high as 10% and cost the country's National Health Service (NHS) approximately 1 billion pounds annually.
Collated data on the incidence of wound infections probably underestimate the true incidence because most wound infections occur when the patient is discharged, and these infections may be treated in the community without hospital notification.
Prognosis
SSIs are associated not only with increased morbidity but also with substantial mortality. In one study, 77% of the deaths of surgical patients were related to surgical wound infection. [14] Kirkland et al calculated a relative risk of death of 2.2 attributable to SSIs, in comparison with matched surgical patients without infection. [15]
-
Wound infection due to disturbed coagulopathy. This patient has a pacemaker (visible below right clavicular space) and had previous cardiac surgery (median sternotomy wound visible) for a rheumatic mitral valve disorder, which was replaced. The patient was taking anticoagulants preoperatively. Despite converting to low-molecular weight subcutaneous heparin treatment and establishing normal coagulation studies, she developed a postoperative hematoma with subsequent wound infection. She had the hematoma evacuated and was administered antibiotic treatment as guided by microbiological results, and the wound was left to heal by secondary intention.
-
Abscess secondary to a subclavian line.
-
Definitions of surgical site infection (SSI).
-
Factors that affect surgical wound healing.
-
Large ulceration in a tattoo. A 33-year-old man presented with a superficial ulceration about 4 weeks after a red tattoo on his forearm. Microbial swabs remained negative. His medical history was uneventful and he was in good general health. No reason for this uncommon reaction could be identified. Image courtesy of the National Institutes of Health.