Background
Toxoplasmosis is caused by infection with the protozoan Toxoplasma gondii, [1] an obligate intracellular parasite. The infection produces a wide range of clinical syndromes in humans, land and sea mammals, and various bird species. T gondii has been recovered from locations throughout the world, except Antarctica (see the image below). (See Etiology and Pathophysiology.)
Nicolle and Manceaux first described the organism in 1908, after they observed the parasites in the blood, spleen, and liver of a North African rodent, Ctenodactylus gondii. The parasite was named Toxoplasma (arclike form) gondii (after the rodent) in 1909. In 1923, Janku reported parasitic cysts in the retina of an infant who had hydrocephalus, seizures, and unilateral microphthalmia. Wolf, Cowan, and Paige (1937-1939) determined that these findings represented the syndrome of severe congenital T gondii infection.
There are 3 major genotypes (type I, type II, and type III) of T gondii. These genotypes differ in their pathogenicity and prevalence in people. In Europe and the United States, type II genotype is responsible for most cases of congenital toxoplasmosis. [2]
T gondii infects a large proportion of the world's population (perhaps one third) but uncommonly causes clinically significant disease. [3] However, certain individuals are at high risk for severe or life-threatening toxoplasmosis. Individuals at risk for toxoplasmosis include fetuses, newborns, and immunologically impaired patients. (See Etiology and Pathophysiology and Epidemiology.)
Congenital toxoplasmosis usually is a subclinical infection. Among immunodeficient individuals, toxoplasmosis most often occurs in those with defects of T-cell–mediated immunity, such as those with hematologic malignancies, bone marrow and solid organ transplants, or acquired immunodeficiency syndrome (AIDS).In most immunocompetent individuals, primary or chronic (latent) T gondii infection is asymptomatic. A small percentage of these patients eventually develop retinochoroiditis, lymphadenitis, or, rarely, myocarditis and polymyositis. (SeePresentation and Workup.)
Patient education
Primary prevention based on prenatal education could be an effective strategy to reduce congenital toxoplasmosis. Educate the public in toxoplasmosis-prevention methods, such as protecting children's play areas from cat litter. Mothers with toxoplasmosis must be completely informed of the disease’s potential consequences to the fetus. [4] (See Etiology.)
Etiology and Pathophysiology
Life cycle of Toxoplasma gondii
T gondii has 2 distinct life cycles. The sexual cycle occurs only in cats, the definitive host. The asexual cycle occurs in other mammals (including humans) and various strains of birds. It consists of 2 forms: tachyzoites (the rapidly dividing form observed in the acute phase of infection) and bradyzoites (the slowly growing form observed in tissue cysts).
A cat becomes infected with T gondii by eating contaminated raw meat, wild birds, or mice. [5] The organism’s sexual cycle then begins in the cat’s gastrointestinal (GI) tract. Macrogametocytes and microgametocytes develop from ingested bradyzoites and fuse to form zygotes. The zygotes then become encapsulated within a rigid wall and are shed as oocysts. The zygote sporulates and divides to form sporozoites within the oocyst. Sporozoites become infectious 24 hours or more after the cat sheds the oocyst via feces.
During a primary infection, the cat can excrete millions of oocysts daily for 1-3 weeks. The oocysts are very strong and may remain infectious for more than one year in warm humid environments.
T gondii oocysts, tachyzoites, and bradyzoites can cause infection in humans. Infection can occur by ingestion of oocysts following the handling of contaminated soil or cat litter or through the consumption of contaminated water or food sources (eg, unwashed garden vegetables). [5] Transmission of tachyzoites to the fetus can occur via the placenta following primary maternal infection.
Rarely, infection by tachyzoites occurs from ingestion of unpasteurized milk or by direct entry into the bloodstream through a blood transfusion or laboratory accident. Transmission can also occur via ingestion of tissue cysts (bradyzoites) in undercooked or uncooked meat or through transplantation of an organ that contains tissue cysts. (Slaughterhouse workers and butchers may be at increased risk of infection.) In Europe and the United States, pork is the major source of T gondii infection in humans.
The seroprevalence of T gondii antibodies in the human population varies geographically, with prevalence rates approaching 90% in some European countries, while seropositivity rates in the United States have been estimated to fall between 10% and 15%. [6, 7] Infection with the human immunodeficiency virus (HIV) does not seem to effect T gondii seropositivity, and there does not appear to be any difference in the rate of toxoplasmosis infection among patients with AIDS with and without cats. [7]
Cellular invasion
As previously stated, T gondii oocysts are ingested in material contaminated by feces from infected cats. Oocysts may also be transported to food by flies and cockroaches. When T gondii is ingested, bradyzoites are released from cysts or sporozoites are released from oocysts, and the organisms enter gastrointestinal cells. Host cell receptors consisting of laminin, lectin, and SAG1 are involved in T gondii tachyzoite attachment and penetration. Tachyzoites multiply, rupture cells, and infect contiguous cells. They are transported via the lymphatics and are disseminated hematogenously throughout the tissues.
The ability of T gondii to actively penetrate host cells results in formation of a parasitophorous vacuole that is derived from the plasma membrane, which is entirely distinct from a normal phagocytic or endocytic compartment. [8] Following apical attachment, the parasite rapidly enters the host cell in a process that is significantly faster than phagocytosis. The vacuole is formed primarily by invagination of the host cell plasma membrane, which is pulled over the parasite through the concerted action of the actin-myosin cytoskeleton of the parasite. During invasion, the host cell is essentially passive and no change is detected in membrane ruffling, the actin cytoskeleton, or phosphorylation of host cell proteins. (See the images below.)
Tachyzoites proliferate, producing necrotic foci surrounded by a cellular reaction. Upon the development of a normal immune response, tachyzoites disappear from tissues. In immunodeficient individuals and in some apparently immunologically healthy patients, the acute infection progresses, resulting in potentially lethal consequences such as pneumonitis, myocarditis, and necrotizing encephalitis.
Tissue cysts form as early as 7 days after infection and remain for the lifespan of the host. The tissue cysts are up to 60μm in diameter, each containing up to 60,000 organisms. They produce little or no inflammatory response but cause recrudescent disease in immunocompromised patients or retinochoroiditis in congenitally infected older children.
Changes in T-lymphocyte levels
Alterations in subpopulations of T lymphocytes are profound and prolonged during acute acquired T gondii infection. These have been correlated with disease syndromes but not with disease outcome. Some patients with prolonged fever and malaise have lymphocytosis, increased suppressor T-cell counts, and a decreased helper-to-suppressor T-cell ratio. These patients may have fewer helper cells even when they are asymptomatic.
In some patients with lymphadenopathy, helper-cell counts are diminished for more than 6 months after infection onset. Ratios of T-cell subpopulations may also be abnormal in asymptomatic patients. Some patients with disseminated toxoplasmosis have a very marked reduction in T cells and a marked depression in the ratio of helper to suppressor T lymphocytes. Depletion of inducer T lymphocytes in patients with AIDS may contribute to the severe manifestations of toxoplasmosis observed in these patients.
Retinochoroiditis
Retinochoroiditis usually results from reactivation of congenital infection, although cases have been recorded that were part of acute infection. [9, 10]
There are 5 hypotheses related to the inflammatory process of ocular toxoplasmosis, as follows [11] :
-
Infection and inflammatory response after spontaneous cyst rupture
-
Parasitic toxic mediators released from T gondii
-
Lytic effect of inflammatory mediators
-
Delayed-type hypersensitivity reaction to antigens of T gondii
-
Cell-mediated immunity against retinal antigens
When the organism reaches the eye through the bloodstream, depending on the host's immune status, a clinical or subclinical focus of infection begins in the retina. As the host's immune system responds and the tachyzoites convert themselves into bradyzoites, the cyst forms. The cyst is extremely resistant to the host's defenses, and a chronic, latent infection ensues. If a subclinical infection is present, no funduscopic changes are observed. The cyst remains in the normal-appearing retina. Whenever the host's immune function declines for any reason, the cyst wall may rupture, releasing organisms into the retina, and the inflammatory process restarts. If an active clinical lesion is present, healing occurs as a retinochoroidal scar. The cyst often remains inactive within or adjacent to the scar. (See the image below.)
Toxoplasma parasites are rarely identified in aqueous humor samples from patients with active ocular toxoplasmosis. [12] This suggests that parasite proliferation occurs only during the early phase of infection and that the retinal damages are probably caused by subsequent inflammatory responses.
When human retinal pigment epithelium (RPE) cells are infected with Toxoplasma gondii, there is an increased production of several cytokines, including interleukin 1beta (IL-1ß), interleukin 6 (IL-6), granulocyte-macrophage colony-stimulating factor, and intercellular adhesion molecule (ICAM). [13] Patients with acquired toxoplasmic retinochoroiditis exhibit higher levels of IL-1 than asymptomatic patients. [14]
It appears that IL-1 gene polymorphisms, in particular genotypes that are related with a high production of IL-1a, may be associated with recurrence of toxoplasmic retinochoroiditis. [15] IL-10 polymorphisms associated with a low production of IL-10 also appear to be associated with the occurrence of toxoplasmic retinochoroiditis. [16] In contrast, tumor necrosis factor (TNF)–alpha gene polymorphism has not been found to be associated with the occurrence or recurrence of toxoplasmic retinochoroiditis. [17]
Congenital toxoplasmosis
Approximately 10-20% of pregnant women infected with T gondii become symptomatic. [18] The most common signs of infection are lymphadenopathy and fever. If the mother was infected prior to pregnancy, there is virtually no risk of fetal infection, as long as she remains immunocompetent. [18]
When a mother is infected with T gondii during gestation, the parasite may be disseminated hematogenously to the placenta. When this occurs, infection may be transmitted to the fetus transplacentally or during vaginal delivery. [19, 20]
If the mother acquires the infection in the first trimester and it goes untreated, the risk of infection to the fetus is approximately 14-17%, and toxoplasmosis in the infant is usually severe. If the mother is infected in the third trimester and it goes untreated, the risk of fetal infection is approximately 59-65%, and involvement is mild or not apparent at birth. These different rates of transmission are most likely related to placental blood flow, the virulence and amount of T gondii acquired, and the immunologic ability of the mother to restrict parasitemia.
The most significant manifestation of toxoplasmosis in the fetus is encephalomyelitis, which may have severe results. Approximately 10% of prenatal T gondii infections result in abortion or neonatal death. In approximately 67-80% of prenatally infected infants, the infection is subclinical and can be diagnosed using only serological and other laboratory methods. Although these infants appear healthy at birth, they may develop clinical symptoms and deficiencies later in life.
Congenital toxoplasmosis caused by atypical genotypes is more severe than that caused by typical genotypes. [2]
Some infants with more severe congenital infection appear to have Toxoplasma antigen–specific lymphocytic anergy, which may be important in the pathogenesis of their disease. Monoclonal gammopathy of the immunoglobulin G (IgG) class has been described in congenitally infected infants, and IgM levels may be elevated in newborns with congenital toxoplasmosis. Glomerulonephritis with deposits of IgM, fibrinogen, and Toxoplasma antigen has been reported in congenitally infected individuals.
Circulating immune complexes have been detected in sera from an infant with congenital toxoplasmosis and in older individuals with systemic, febrile, and lymphadenopathic forms of toxoplasmosis. However, these complexes did not persist after signs and symptoms resolved. Total serum levels of IgA may be diminished in congenitally infected babies, but no predilection toward associated infections has been noted. The predilection toward predominant involvement of the central nervous system (CNS) and retina in this congenital infection has not been fully explained.
Infection in immunocompromised patients
Most cases of toxoplasmosis in immunocompromised patients are a consequence of latent infection and reactivation. In patients with AIDS, T gondii tissue cysts can reactivate with CD4 counts of less than 200 cells/μL; with counts of less than 100 cells/μL, clinical disease becomes more likely. [21] Without adequate prophylaxis or restoration of immune function, patients with CD4 counts of less than 100 cells/μL who are T gondii IgG-antibody positive have a 30% risk of eventually developing reactivation disease. [22]
Although toxoplasmosis in immunocompromised patients may manifest as retinochoroiditis, reactivation disease in these individuals typically is in the CNS, with brain involvement being common.
Toxoplasmic encephalitis and brain abscess present most commonly as headache, but focal neurologic deficits and seizures are as common. With significant disease, patients may also demonstrate the signs and symptoms of elevated intracranial pressure. Cerebral toxoplasmosis is generally identified on computed tomography (CT) scan as multiple ring-enhancing lesions; however, solitary lesions may be seen, and negative CT or magnetic resonance imaging (MRI) scans should not rule out the diagnosis of CNS toxoplasmosis. [23]
Aside from CNS toxoplasmosis, other conditions commonly identified in immunocompromised patients include toxoplasmic pneumonitis, myocarditis, and disseminated toxoplasmosis. Toxoplasmic pneumonitis typically presents with symptoms typical for an infectious pulmonary process, including fever, dyspnea, and cough. Chest radiography is often nonspecific, but findings may have an appearance similar to that of Pneumocystis (carinii) jiroveci pneumonia. Diagnosis is established via bronchoalveolar lavage. Most patients with extra-CNS manifestations of toxoplasmosis will also be noted to have CNS lesions when appropriate radiographic studies have been performed. [24]
Effects of toxoplasmosis on mental disorders
Recent investigations have suggested that chronic toxoplasmosis may play several roles in the etiology of different mental disorders. [25]
Numerous clinical studies have evaluated the prevalence of anti-Toxoplasma antibodies in patients with schizophrenia and other forms of severe psychiatric disorders. The most probable mechanism by which T gondii could cause schizophrenia is by affecting neurotransmitters in brain areas known to be involved in schizophrenia. [26, 27] According to these studies, bradyzoites of T gondii affect dopamine and other neurotransmitters in rodents and humans. A few studies have also investigated the association between T gondii infection and Parkinson and Alzheimer diseases. [28, 29] T. gondii may play a role in the progression of Alzheimer's disease using mechanisms such as induction of host immune responses, inflammation of the central nervous system (CNS), alteration in neurotransmitter levels, and activation of indoleamine-2,3-dyoxygenase. [30] T. gondii may account for approximately 17% of traffic accidents (6–29%) and 10% of suicide attempts (3–19%). [31]
Epidemiology
Occurrence in the United States
Approximately 225,000 cases of toxoplasmosis are reported each year, resulting in 5000 hospitalizations and 750 deaths, making T gondii the third most common cause of lethal foodborne disease in the United States.
Seropositivity rates in the United States have been reported to be between 10% and 15%, although sources vary, and higher infection rates have been estimated. [6, 7] In general, the incidence of the infection varies by population group and geographic locale. For example, the cultural habits of a population may affect the acquisition of T gondii infection from ingested tissue cysts in undercooked or uncooked meat.
The prevalence of T gondii antibodies in US military recruits decreased by one third from 1965-1989; the crude seropositivity rate among recruits from 49 states was 9.5% in 1989, compared with 14.4% in 1965. T gondii infection affects more than 3500 newborns in the United States each year. T gondii seropositivity rates among patients with HIV infection vary from 10-45%.
Toxoplasmosis is more common in southern states, in African Americans, and in populations with lower socioeconomic status. [32]
Intraocular toxoplasmosis manifested by necrotizing retinochoroiditis has been reported in 1-21% of patients with acquired systemic infections. In a population study, 0.6% residents of Maryland were found to have scars consistent with ocular toxoplasmosis. [33]
Toxoplasmic encephalitis has been reported in 1-5% of patients with AIDS. Within the United States, significant differences are recognized in the incidence of toxoplasmic encephalitis by geographic region and by ethnic group. Toxoplasmosis in patients with AIDS is reported to occur 3 times more frequently in Florida than in other areas of the United States; in patients of Haitian origin with AIDS who live in Florida, 12-40% develop toxoplasmic encephalitis.
Toxoplasmic encephalitis has been reported to be the index AIDS diagnosis in 44-58% of patients with HIV infection who have toxoplasmic encephalitis.
International occurrence
In many populations, such as those in El Salvador and France, the seropositivity rate to T gondii is as high as 75% by the fourth decade of life. As many as 90% of adults in Paris are seropositive. Approximately 50% of the adult population in Germany is infected. Women of childbearing age in much of Western Europe, Africa, and South and Central America have seroprevalence rates of greater than 50%. [34]
Based on serologic studies, estimates suggest the incidence of primary maternal T gondii infection during pregnancy ranges from about 1-310 cases per 10,000 pregnancies in different populations in Europe, Asia, Australia, and the Americas. The incidence of prenatal T gondii infection within the same or similar populations has been estimated to range from about 1-120 cases per 10,000 births. [35, 36, 37, 38, 39]
The prevalence of immunocompromised patients is higher in some nations as a function of HIV/AIDS infection and also organ transplantation and immunomodulatory medication prescribing. In individuals with HIV infection, the seropositivity rate to T gondii is approximately 50-78% in certain areas of Western Europe and Africa.
Toxoplasmic encephalitis is the AIDS-defining diagnosis in 16% of patients with AIDS. In France, 37% of patients with AIDS have evidence of toxoplasmic encephalitis at autopsy.
Age-related demographics
With the exception of T gondii retinochoroiditis, older individuals are more likely to manifest clinically evident reactivation of Tgondii infection. Congenitally acquired Tgondii retinochoroiditis is more likely to recur in persons older than 40 years. [40]
Prognosis
Immunocompetent patients have an excellent prognosis, and lymphadenopathy and other symptoms generally resolve within weeks of infection.
Toxoplasmosis in immunodeficient patients often relapses if treatment is stopped. Suppressive therapy and immune reconstitution significantly reduce the risk for recurrent infection.
Multiple complications may occur in persons with congenital toxoplasmosis, including intellectual disability, seizures, deafness, and blindness. Treatment may prevent the development of untoward sequelae in symptomatic and asymptomatic infants with congenital toxoplasmosis. Infants with congenitally acquired toxoplasmosis generally have a good prognosis and are on average developmentally identical to noninfected infants by the fourth year of life.
Toxoplasmic encephalitis and brain abscess can result in permanent neurologic sequelae, depending on the location of the lesion and the extent of local damage and inflammation. Basal ganglia seem to be preferentially involved. Seizure disorder or focal neurologic deficits may occur in persons with CNS toxoplasmosis.
Ophthalmic complications
Toxoplasmosis is the most common cause of intraocular inflammation and posterior uveitis in immunocompetent patients throughout the world. Toxoplasmosis is responsible for approximately 30-50% of all posterior uveitis cases in the United States.
Retinochoroiditis is a relatively common manifestation of T gondii infection. Ocular toxoplasmosis occurs when cysts deposited in or near the retina become active, producing tachyzoites. Focal necrotizing retinitis is the characteristic lesion, but retinal scars from prior reactivation typically are present. Presentation usually involves eye pain and decreased visual acuity. Adults who acquired disease in infancy usually present with bilateral eye involvement. Adults with acute infection generally present with unilateral ocular involvement. [40, 41, 42, 43]
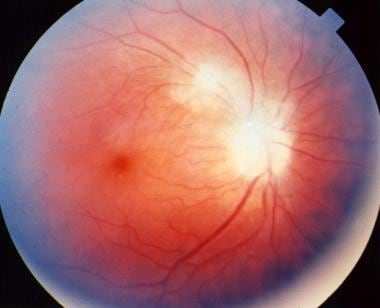
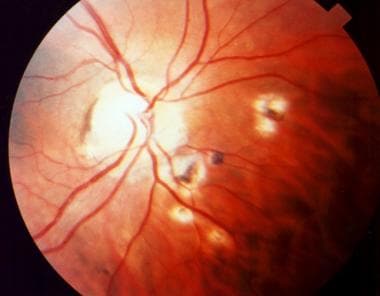
Depending on the location and severity of toxoplasmic retinochoroiditis, infection can result in permanent retinal scarring and loss of visual acuity. Recurrent episodes are common, resulting in multiple areas of retinal scarring and functional loss. (See the images below.)
 Ophthalmic toxoplasmosis. Used with permission of Anton Drew, ophthalmic photographer, Adelaide, South Australia.
Ophthalmic toxoplasmosis. Used with permission of Anton Drew, ophthalmic photographer, Adelaide, South Australia.
 Acute macular retinitis associated with primary acquired toxoplasmosis, requiring immediate systemic therapy.
Acute macular retinitis associated with primary acquired toxoplasmosis, requiring immediate systemic therapy.
Vascular endothelial growth factor (VEGF) has been shown to be a key molecular player in the pathogenesis of choroidal neovascular membrane (CNV). In the current era of anti-VEGF therapy, the extraordinary results obtained in CNV secondary to age-related macular degeneration have been extrapolated to other causes of CNV with apparent good results. [44, 45] Currently available anti-VEGF agents include bevacizumab, ranibizumab, and pegaptanib sodium.
Secondary glaucoma may occur with anterior uveitis that is secondary to the obstruction of the outflow channels by the inflammatory cells. This condition may or may not be reversible.
Destruction of the trabecula by chronic inflammation and anterior synechiae may also create a chronic pharmacologically nonresponsive glaucoma.
Other ocular complications include:
-
Cataract
-
Posterior synechiae
-
Cystoid macular edema
-
Retinal perivasculitis
-
Optic atrophy
-
Epiretinal membrane
-
Persistent vitreous opacities
Morbidity and mortality
Acute toxoplasmosis is asymptomatic in 80-90% of healthy hosts. In some apparently immunologically healthy patients, however, the acute infection progresses and may have lethal consequences.
Although a relatively small percentage of toxoplasmosis cases are congenital, they tend to account for most acute and fatal infections.
In immunosuppressed patients, T gondii infection, like other opportunistic infections, can lead to rapidly progressive, fatal disease. Indeed, toxoplasmosis is recognized as a major cause of neurologic morbidity and mortality among patients with advanced HIV disease.
However, the incidence of toxoplasmosis (including CNS disease) in patients with AIDS has declined dramatically, likely due to the evolution of highly active antiretroviral therapy (HAART) and the routine use of prophylaxis against P (carinii) jiroveci and T gondii. The incidence of CNS toxoplasmosis decreased from 5.4 cases per 1000 person-years between 1990 and 1992 to 2.2 cases per 1000 persons-years between 1996 and 1998. [46] The routine use of cotrimoxazole prophylaxis in the United States and internationally has also likely significantly decreased the incidence of CNS toxoplasmosis.
Pathophysiology
Chronic infection occurs 2 to 3 weeks after infection, when the production of cytokines and antibodies against many T gondii proteins begins. Extracellular tachyzoites are cleared from host tissues and intracellular parasites differentiate into occult bradyzoite forms surrounded by a parasitophore vacuole enclosed in a cyst wall. In this clinical phase, the cysts are preferentially located in the neural and muscle tissues and rupture periodically. However, since the released bradyzoites normally are destroyed by the host's immune response, the majority remain in the brain and muscles indefinitely and develop lifelong protective immunity against re-infection. The ability of bradyzoites to evade the host immune response and remain in a quiescent form within the host is another status in the T gondii life cycle.
If parasite proliferation is not controlled by the immune system, it causes a generalized toxoplasmosis, which always is fatal. Host T-cell-mediated immune responses play an important role in suppressing tachyzoite replication and resistance to T gondii, resulting in chronic infection or possibly clearance of parasites. Although the infection usually is asymptomatic in immunocompetent individuals, the multiple clinical manifestations of chronic infection are usually defined as inflammation followed by necrosis. About 10-20% of infected immunocompetent individuals react with rupture of a tissue cyst in the eye, brain, or muscles during chronic infection, causing local necrosis accompanied by inflammation. Hypersensitivity plays an important role in such reactions. [47, 48, 49]
-
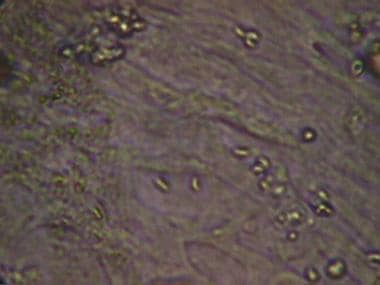
Toxoplasma gondii tachyzoites (Giemsa stain).
-
Toxoplasma gondii tachyzoites in cell line.
-
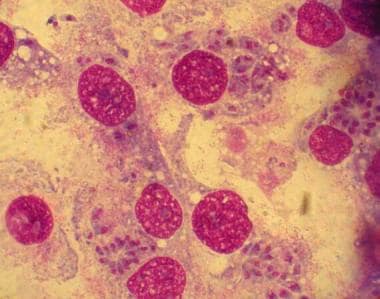
Toxoplasma gondii in infected monolayers of HeLa cells (Giemsa stain).
-
Ophthalmic toxoplasmosis. Used with permission of Anton Drew, ophthalmic photographer, Adelaide, South Australia.
-
Macular scar secondary to congenital toxoplasmosis. Visual acuity of the patient is 20/400.
-
Papillitis secondary to toxoplasmosis, necessitating immediate systemic therapy.
-
Acute macular retinitis associated with primary acquired toxoplasmosis, requiring immediate systemic therapy.
-
Peripapillary scars secondary to toxoplasmosis.
-
Perimacular scars secondary to toxoplasmosis.
-
Inactive retinochoroidal scar secondary to toxoplasmosis.