Background
Tetanus is characterized by an acute onset of hypertonia, painful muscular contractions (usually of the muscles of the jaw and neck), and generalized muscle spasms without other apparent medical causes. Despite widespread immunization of infants and children since the 1940s, tetanus still occurs in the United States. [1] Tetanus primarily affects older adults because of their higher rate of being unvaccinated or of being inadequately vaccinated. [2] The image below illustrates tetanus cases in the United States from 1947-2021.
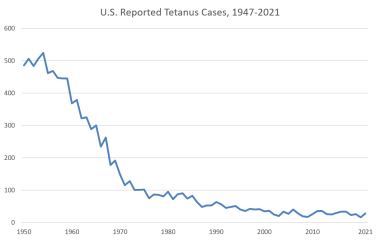 Reported number of tetanus cases in the United States from 1947-2021. Image from National Notifiable Disease Surveillance System (NNDSS), Centers for Disease Control and Prevention (CDC).
Reported number of tetanus cases in the United States from 1947-2021. Image from National Notifiable Disease Surveillance System (NNDSS), Centers for Disease Control and Prevention (CDC).
Tetanus may be categorized into the following 4 clinical types [3, 4] :
-
Generalized tetanus
-
Localized tetanus
-
Cephalic tetanus
-
Neonatal tetanus
Approximately 50-75% of patients with generalized tetanus present with trismus (“lockjaw”), which is the inability to open the mouth secondary to masseter muscle spasm. Nuchal rigidity and dysphagia also are early complaints that cause risus sardonicus, the scornful smile of tetanus, resulting from facial muscle involvement. [5, 6]
As the disease progresses, patients have generalized muscle rigidity with intermittent reflex spasms in response to stimuli (eg, noise, touch). Tonic contractions cause opisthotonos (ie, flexion and adduction of the arms, clenching of the fists, and extension of the lower extremities). During these episodes, patients have an intact sensorium and feel severe pain. The spasms can cause fractures, tendon ruptures, and acute respiratory failure.
Patients with localized tetanus present with persistent rigidity in the muscle group close to the injury site. [7] The muscular rigidity is caused by a dysfunction in the interneurons that inhibit the alpha motor neurons of the affected muscles. No further central nervous system (CNS) involvement occurs in this form, and mortality is very low.
Cephalic tetanus is uncommon and usually occurs after head trauma or otitis media. Patients with this form present with cranial nerve (CN) palsies. The infection may be localized or may become generalized. [8]
Neonatal tetanus (tetanus neonatorum) is a major cause of infant mortality in underdeveloped countries but is rare in the United States. Infection results from umbilical cord contamination during unsanitary delivery, coupled with a lack of maternal immunization. At the end of the first week of life, infected infants become irritable, feed poorly, and develop rigidity with spasms. Neonatal tetanus has a very poor prognosis. [9, 10]
While tetanus is at present quite rare, early diagnosis and intervention are lifesaving. Prevention is the ultimate management strategy for tetanus.
Pathophysiology
Clostridium tetani is an obligate, anaerobic, motile, gram-positive bacillus. [4] It is nonencapsulated and forms spores that are resistant to heat, desiccation, and disinfectants. Since the colorless spores are located at one end of the bacillus, they cause the organism to resemble a turkey leg. They are found in soil, house dust, animal intestines, and human feces. Spores can persist in normal tissue for months to years.
To germinate, the spores require specific anaerobic conditions, [11] such as wounds with low oxidation-reduction potential (eg, dead or devitalized tissue, foreign body, active infection). Under these conditions, upon germination, they may release their toxin. Infection by C tetani results in a benign appearance at the portal of entry because of the inability of the organism to evoke an inflammatory reaction unless coinfection with other organisms develops.
When the proper anaerobic conditions are present, the spores germinate and produce the following 2 toxins:
-
Tetanolysin – This substance is a hemolysin with no recognized pathologic activity
-
Tetanospasmin – This toxin is responsible for the clinical manifestations of tetanus [12] ; by weight, it is one of the most potent toxins known, with an estimated minimum lethal dose of 2.5 ng/kg body weight
Tetanospasmin is synthesized as a 150-kd protein consisting of a 100-kd heavy chain and a 50-kd light chain joined by a disulfide bond. [13] The heavy chain mediates binding of tetanospasmin to the presynaptic motor neuron and also creates a pore for the entry of the light chain into the cytosol. The light chain is a zinc-dependent protease that cleaves synaptobrevin. [14]
After the light chain enters the motor neuron, it travels by retrograde axonal transport from the contaminated site to the spinal cord in 2-14 days. When the toxin reaches the spinal cord, it enters central inhibitory neurons. The light chain cleaves the protein synaptobrevin, which is integral to the binding of neurotransmitter containing vesicles to the cell membrane.
As a result, gamma-aminobutyric acid (GABA)-containing and glycine-containing vesicles are not released, and there is a loss of inhibitory action on motor and autonomic neurons. [14] With this loss of central inhibition, there is autonomic hyperactivity as well as uncontrolled muscle contractions (spasms) in response to normal stimuli such as noises or lights.
Once the toxin becomes fixed to neurons, it cannot be neutralized with antitoxin. Recovery of nerve function from tetanus toxins requires sprouting of new nerve terminals and formation of new synapses.
Localized tetanus develops when only the nerves supplying the affected muscle are involved. Generalized tetanus develops when the toxin released at the wound spreads through the lymphatics and blood to multiple nerve terminals. The blood-brain barrier prevents direct entry of toxin to the CNS.
Etiology
Tetanus is caused by the active toxin-producing bacillus form of Clostridium tetani. Spores of C tetani are ubiquitous in the environment and can survive for years. [15] These spores are resistant to many forms of decontamination, but can convert to tetanus bacilli under the appropriate anaerobic conditions, at which point they produce tetanus toxins. Infection most commonly occurs due to wound contamination with spores, even from wounds where medical attention was not deemed necessary. [12] Cases have been documented without obvious wounds of sites for infection. Childbirth is a significant cause of tetanus infection in the developing world. [15] Moreover, injection drug use has been linked to disease clusters in the United States. [16] Chronic wounds, such as venous or diabetic foot ulcers, also have been associated with cases of tetanus. [17]
Underimmunization is an important cause of tetanus. [2] Tetanus affects nonimmunized persons, partially immunized persons, or fully immunized individuals who do not maintain adequate immunity with periodic booster doses. Only 12-14% of patients with tetanus in the United States have received a primary series of tetanus toxoid. During 2001-2008, 10% of all patients with tetanus were known to be current with tetanus immunization, with only one death among this group. Surveillance data from 1998-2000 revealed the following [16] :
-
In 73% of patients with tetanus in the United States, tetanus occurred after an acute injury, including puncture wounds (50%), lacerations (33%), and abrasions (9%)
-
Stepping on a nail accounted for 32% of the puncture wounds
-
Tetanus was found to occur in burn victims; in patients receiving intramuscular injections; in persons obtaining a tattoo; and in persons with frostbite, dental infections (eg, periodontal abscesses), penetrating eye injuries, and umbilical stump infections
-
Other reported risk factors included diabetes, chronic wounds (eg, skin ulcers, abscesses, or gangrene), parenteral drug abuse, and recent surgery (4% of US cases)
-
During 1998-2000, 12% of patients with tetanus in the United States had diabetes (with mortality, 31%), compared with 2% during 1995-1997; of these patients, 69% had acute injuries and 25% had gangrene or a diabetic ulcer
-
The median time interval between surgery and onset of tetanus was 7 days
-
Tetanus was reported after tooth extractions, root canal therapy, and intraoral soft tissue trauma
Worldwide risk factors for neonatal tetanus include the following [15] :
-
Use of inadequately-sterilized instruments or contaminated dressings
-
Unvaccinated mother
-
Lack of hand cleansing by provider prior to delivery
Immunity from tetanus decreases with advancing age. [18] Serologic testing for immunity has revealed a low level among elderly individuals in the United States. Approximately 50% of adults older than 50 years are nonimmune because they never were vaccinated or do not receive appropriate booster doses. The prevalence of immunity to tetanus in the United States exceeds 80% for persons aged 6-39 years but is only 28% for those older than 70 years.
Epidemiology
United States statistics
Because of the widespread use of tetanus immunizations, the reported incidence of tetanus in the United States has declined substantially since the mid 1940s. [19]
From 2001-2008, 233 cases of tetanus were reported in the United States, a 95% reduction since 1947. Deaths from the disease had decreased by 99% since that year. The case mortality rate was 13.2%. Tetanus cases among Hispanics were approximately twice that among non-Hispanics, attributed to an increased rate of injection drug use among Hispanic patients. In the group of patients with known vaccination status, 40.2% had received no doses of tetanus toxoid; 15.4% of 195 patients had diabetes, and 15.3% of 176 were intravenous drug users. In the 51 individuals with an acute wound in whom adequate information was available, 96.1% had not received appropriate prophylaxis. [2]
In 2022, 22 tetanus cases were reported in the United States via the National Notifiable Diseases Surveillance System (NNDSS). [20]
All 50 states require that children be vaccinated before being admitted to public schools. More than 96% of children have received 3 or more diphtheria and tetanus toxoids plus pertussis (DTP) vaccinations by the time they begin school.
In 2022, vaccination uptake by age 14 years among adolescents born in 2008 continued to fall behind that of earlier birth cohorts and differed according to sociodemographic factors and access to healthcare compared with that among earlier birth cohorts. [21]
Vaccination uptake by age 13 years among those born in 2009 was similar to coverage estimates reported before the COVID-19 pandemic.
Among individuals aged 13-17 years, 2022 vaccination coverage levels were similar to 2021 levels; however, initiation of the HPV vaccination series fell among Medicaid beneficiaries. Coverage with at least 1 dose of tetanus, diphtheria, and acellular pertussis vaccine and at least 1 dose meningococcal conjugate vaccine was high and stable (around 90%). Healthcare providers should review adolescent vaccination records, especially those of adolescents born in 2008 as well as children and adolescents who are eligible for the Vaccines for Children program, to ensure all recommended vaccines are current.
Heroin users, particularly those who inject themselves subcutaneously, appear to be at high risk for tetanus. Quinine is used to dilute heroin and may support the growth of C tetani. [22] The incidence of tetanus in people who use injection drugs increased 7.4% between 1991 and 1997, from 3.6% of all cases in 1991-1994 to 11% in 1995-1997. Injection drug users accounted for 15% of US tetanus cases from 1998 to 2000 (see the image below). [16] Of the 19 people who used injection drugs and contracted tetanus in 1998-2000, only 1 reported an acute injury.
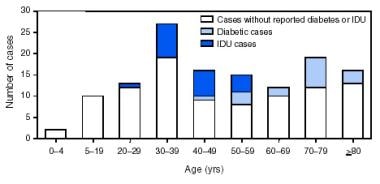 Image from "Number of Tetanus Cases Reported Among Persons With Diabetes or Injection-Drug Use (IDU), by Age Group." Pascual FB, McGinley EL, Zanardi LR, et al: Tetanus surveillance—United States, 1998−2000. MMWR Surveill Summ. 2003 Jun 20;52(3):1-8.
Image from "Number of Tetanus Cases Reported Among Persons With Diabetes or Injection-Drug Use (IDU), by Age Group." Pascual FB, McGinley EL, Zanardi LR, et al: Tetanus surveillance—United States, 1998−2000. MMWR Surveill Summ. 2003 Jun 20;52(3):1-8.
From 1998-2000, 81% of cases in the United States were generalized tetanus, 17% were localized, and 2% were cephalic; 1 case of neonatal tetanus was reported.
International statistics
C tetani is found worldwide in soil, on inanimate objects, in animal feces, and, occasionally, in human feces. Tetanus is predominantly a disease of underdeveloped countries. It is common in areas where soil is cultivated, in rural areas, in warm climates, during summer months, and among males. In countries without a comprehensive immunization program, tetanus predominantly develops in neonates and young children. [23, 24]
From 1990 to 2019, the incidence and death rate of tetanus fell significantly globally. [25]
Developed nations have incidences of tetanus similar to those observed in the United States. For instance, only 126 cases of tetanus were reported in England and Wales from 1984-1992. [26] More recently, the UK reported only 4 cases of tetanus in England during 2022, down from 11 cases the previous year. [27]
Although tetanus affects all ages, the highest prevalence is in newborns and young people. [28] The global burden of disease has fallen significantly since approximately 1990. [25] Incidence has decreased from an estimated 615,000 cases globally in 1990 to about 74,000 in 2019. Additionally, annual deaths from tetanus fell from 275,000 to 35,000 in this same time period. Neonatal tetanus accounted for half of all cases of tetanus and in some areas was the predominant cause of neonatal mortality, with close to 100% case fatality rates depending on regional access to care.
Age-related demographics
Neonatal tetanus is rare in developed countries while accounting for a large burden of disease in resource-poor areas. [25]
The risk for development of tetanus and for the most severe form of the disease in developed countries is highest in the elderly population. In the United States from 2001-2008, the incidence rate among patients aged 65 years or older was approximately 0.23 cases per 1 million population vs 0.08 cases per 1 million population for those younger than 65 years. [2] Moreover, the relative risk for fatal disease was about five times higher in patients older than 65 compared with those under 65 years. Patient older than 65 years accounted for 77% of deaths during this period.
Sex-related demographics
Tetanus affects both sexes. No overall gender predilection has been reported, except to the extent that males may have more soil exposure in some cultures. In the United States from 1998 to 2000, the incidence of tetanus was 2.8 times higher in males aged 59 years and younger than in females in the same age range. [16]
A difference in the levels of tetanus immunity exists between the sexes, with men being twice as likely to possess protective levels of antibodies compared with women. [18] This is speculated to be because of additional vaccinations administered during military service or professional activities.
Race-related demographics
Tetanus affects all races. From 2001-2008, the incidence of tetanus in the United States was almost twice as high among Hispanic individuals compared with non-Hispanic persons (0.13 vs 0.07 cases per million population). Exclusion of patients with injection drug use showed nearly equal incidences at 0.08 vs 0.07 cases per million populations among Hispanics and non-Hispanics, respectively. Incidence was also similar among other identified racial groups including White Americans (0.08 per million population), African Americans (0.07), American Indian/Alaska native (0.09), and Asian/Pacific Islander (0.07). [2]
Prognosis
The prognosis is dependent on incubation period, the time from spore inoculation to first symptom, and the time from first symptom to first tetanic spasm. [7] The following statements typically hold true [3] :
-
In general, shorter intervals indicate more severe tetanus and a poorer prognosis
-
Patients usually survive tetanus and return to their predisease state of health
-
Recovery is slow and usually occurs over 2-4 months
-
Some patients remain hypotonic
-
Clinical tetanus does not produce a state of immunity; therefore, patients who survive the disease require active immunization with tetanus toxoid to prevent a recurrence
A rating scale has been developed for assessing the severity of tetanus and determining the prognosis. On this scale, 1 point is given for each of the following [3] :
-
Incubation period shorter than 7 days
-
Period of onset shorter than 48 hours
-
Tetanus acquired from burns, surgical wounds, compound fractures, septic abortion, umbilical stump, or intramuscular injection
-
Narcotic addiction
-
Generalized tetanus
-
Temperature higher than 104°F (40°C)
-
Tachycardia exceeding 120 beats/min (150 beats/min in neonates)
The total score indicates disease severity and prognosis as follows:
-
0 or 1 – Mild tetanus; mortality below 10%
-
2 or 3 – Moderate tetanus; mortality of 10-20%
-
4 – Severe tetanus; mortality of 20-40%
-
5 or 6 – Very severe tetanus; mortality above 50%
Cephalic tetanus always is severe or very severe. Neonatal tetanus always is very severe.
The case-fatality ratio in the United States was 91% in 1947, 21-31% from 1982 to 1990, 11% from 1995 to 1997, 18% from 1998 to 2000, and 13.2% from 2001-2008. [16, 2] Mortality in mild and moderate tetanus is approximately 6%; for severe tetanus, it may be as high as 60%. Mortality in the United States resulting from generalized tetanus is 30% overall, 52% in patients older than 60 years, and 13% in patients younger than 60 years.
Mortality is substantially higher for people older than 65 years, with approximately five times the relative risk for death compared to cases in patients younger than 65. [2] From 1998 to 2000, 75% of the deaths in the United States were in patients older than 60 years. [16] In addition, mortality is notably higher for people who require mechanical ventilation (30%) than for those who do not (4%).
Clinical tetanus is less severe among patients who have received a primary series of tetanus toxoid sometime during their life than among patients who are inadequately vaccinated or unvaccinated. [16] Mortality in the United States is 7% for individuals who had previously received at least one dose of tetanus vaccine versus 31% of those who were unvaccinated. [2]
Patient Education
The importance of childhood immunizations and boosters in adulthood must be stressed. Midwives and birth attendants in developing and underdeveloped countries should be given training in aseptic birthing procedures. The basics of wound care and first aid should be widely taught. Early recognition of symptoms and signs of localized tetanus and timely access to medical care are essential.
For patient education resources, see the CDC article on Tetanus as well as the CDC Immunization Schedule, Adults, and Immunization Schedule, Children.
-
Image from "Number of Tetanus Cases Reported and Average Annual Incidence Rates, by State." Pascual FB, McGinley EL, Zanardi LR, et al: Tetanus surveillance—United States, 1998−2000. MMWR Surveill Summ. 2003 Jun 20;52(3):1-8.
-
Image from "Number of Tetanus Cases Reported, Average Annual Incidence Rates, and Survival Status of Patients, by Age Group." Pascual FB, McGinley EL, Zanardi LR, et al: Tetanus surveillance—United States, 1998−2000. MMWR Surveill Summ. 2003 Jun 20;52(3):1-8.
-
Image from "Number of Tetanus Cases Reported Among Persons With Diabetes or Injection-Drug Use (IDU), by Age Group." Pascual FB, McGinley EL, Zanardi LR, et al: Tetanus surveillance—United States, 1998−2000. MMWR Surveill Summ. 2003 Jun 20;52(3):1-8.
-
Reported number of tetanus cases in the United States from 1947-2021. Image from National Notifiable Disease Surveillance System (NNDSS), Centers for Disease Control and Prevention (CDC).







