Overview
Biliary colic and cholecystitis are in the spectrum of biliary tract disease. This spectrum ranges from asymptomatic gallstones to biliary colic, cholecystitis, choledocholithiasis, and cholangitis. [1]
Gallstones can be divided into two categories: cholesterol stones (80%) and pigment stones (20%). Most patients with gallstones are asymptomatic. Stones may temporarily obstruct the cystic duct or pass through into the common bile duct, leading to symptomatic biliary colic, [2] which develops in 1-4% of patients with gallstones annually.
Cholecystitis occurs when obstruction at the cystic duct is prolonged (usually several hours) resulting in inflammation of the gallbladder wall. Acute cholecystitis develops in approximately 20% of patients with biliary colic if they are left untreated. [3] However, the incidence of acute cholecystitis is falling, likely due to increased acceptance by patients of laparoscopic cholecystectomy as a treatment of symptomatic gallstones. [4]
Choledocholithiasis occurs when the stone becomes lodged in the common bile duct, with the potential sequelae of cholangitis and ascending infections.
Biliary sludge is a reversible suspension of precipitated particulate matter in bile in a viscous mucous liquid phase. The most common precipitates are cholesterol monohydrate crystals and various calcium-based crystals, granules, and salts. [5] A portion of biliary sludge contains comparatively large particles (1-3 mm) called microliths, the formation of which is an intermediate step in the formation of gallstones (about 12.5%). [6]
For patient education information, see the Digestive Disorders Center and Gallstones.
Go to Cholecystitis for more information on this topic.
Risk Factors
Cholelithiasis, cholecystitis, and biliary colic
Risk factors for biliary colic and cholecystitis include pregnancy, elderly population, obesity, certain ethnic groups (Northern European and Hispanic), weight loss, and liver transplant patients. [7]
The phrase "fair, female, fat, and fertile" summarizes the major risk factors for development of gallstones. Although gallstones and cholecystitis are more common in women, men with gallstones are more likely to develop cholecystitis (and more severe cholecystitis) than women with gallstones. [8]
Some oral contraceptives or estrogen replacement therapy may increase the risk of gallstones. Drugs that have been associated with cholecystitis include octreotide and ceftriaxone. [9, 10] In addition, the incidence of sludge or stone formation during pregnancy is 5.1% in the second trimester, 7.9% in the third trimester, and 10.2% at 4-6 weeks postpartum. [11, 12]
Age increases rates of gallstones, cholecystitis, and common bile duct stones. Elderly patients are more likely to go from asymptomatic gallstones to serious complications of gallstones without gallbladder colic.
Acalculous cholecystitis
Risk factors for acalculous cholecystitis include diabetes, human immunodeficiency virus (HIV) infection, vascular disease, total parenteral nutrition, prolonged fasting, or being an intensive care unit (ICU) patient.
Children are more likely than adults to have acalculous gallstones. If stones exist, they are more likely pigmented stones from hemolytic diseases (eg, sickle cell diseases, spherocytosis, glucose-6-phosphate dehydrogenase [G-6-PD] deficiency) or chronic diseases (eg, total parenteral nutrition, burns, trauma).
Evaluation of Biliary Colic and Cholecystitis
Symptoms of biliary colic
Typical gallbladder colic generally includes 1-5 hours of constant pain, most commonly in the epigastrium or right upper quadrant. Peritoneal irritation by direct contact with the gallbladder localizes the pain to the right upper quadrant. The pain is severe, dull or boring, constant (not colicky), and may radiate to the right scapular region or back. Patients tend to move around to seek relief from the pain. The onset of pain develops hours after a meal, occurs frequently at night, and awakens the patient from sleep. Associated symptoms include nausea, vomiting, pleuritic pain, and fever.
Symptoms of cholecystitis
Persistence of biliary obstruction leads to cholecystitis and persistent right upper quadrant pain. The character of the pain is similar to gallbladder colic, except that it is prolonged and lasts hours (usually >6 h) or days. Nausea, vomiting, and low-grade fever are associated more commonly with cholecystitis. Up to 70% of patients with cholecystitis report having experienced similar episodes in the past that spontaneously resolved.
Symptoms of cholelithiasis
Most gallstones (60-80%) are asymptomatic at a given time. Smaller stones are more likely to be symptomatic than larger ones. However, almost all patients develop symptoms before complications, such as steady pain in the right hypochondrium or epigastrium, nausea, vomiting, and fever. An acute attack often is precipitated by a large or fatty meal. [2]
Indigestion, belching, bloating, and fatty food intolerance are thought to be typical symptoms of gallstones; however, these symptoms are just as common in people without gallstones and frequently are not cured by cholecystectomy.
Vital signs and appearance
Vital signs parallel the degree of illness. Patients with cholangitis are more likely to have fever, tachycardia, and/or hypotension. Patients with gallbladder colic have relatively normal vital signs. In a retrospective study, only 32% of patients with cholecystitis had fever. Fever may be absent, especially in elderly patients.
Patients with cholecystitis are usually more ill appearing than simple biliary colic patients, and they usually lie still on the examination table, as any movement may aggravate any peritoneal signs. In elderly patients and those with diabetes, occult cholecystitis or cholangitis may be the source of fever, sepsis, or mental status changes.
Jaundice is unusual in the early stages of acute cholecystitis and may be found in fewer than 20% of patients. Frank jaundice should raise suspicion of concomitant choledocholithiasis or Mirizzi syndrome (obstruction of the bile duct as a result of external compression of a stone in the gallbladder or cystic duct).
Abdominal assessment
As in all patients with abdominal pain, perform a complete physical examination, including rectal and pelvic examinations in women.
Abdominal examination in gallbladder colic and cholecystitis is remarkable for epigastric or right upper quadrant tenderness and abdominal guarding. The Murphy sign (an inspiratory pause on palpation of the right upper quadrant) on abdominal examination is widely used in the diagnosis of acute cholecystitis. [13] Singer et al noted that a positive Murphy sign was extremely sensitive (97%) and predictive (positive predictive value [PPV], 93%) for cholecystitis [14] ; however, some debate exists over the sensitivity of the Murphy sign, with some sources citing a very low sensitivity (20%) and others indicating a sensitivity range of 58%-71% (systematic review) and 48%-97% (evidence-based review). [15, 16] The sonographic Murphy sign, however, remains an important sign of cholecystitis. [13, 17, 18, 19, 20]
In elderly patients, sensitivity of the Murphy sign may be decreased. [21]
A palpable fullness in the RUQ may be appreciated in 20% of cases after 24 hours of symptoms, but this finding is rarely present early in the clinical course.
When observed, peritoneal signs should be taken seriously. Most uncomplicated cholecystitis does not have peritoneal signs; thus, search for complications (eg, perforation, gangrene) or other sources of pain.
Diagnosis
Differential diagnosis
When cholecystitis and biliary colic are suspected, the following conditions should also be considered:
Diagnostic Tests
Cholelithiasis and biliary colic
Laboratory studies in cases of cholelithiasis and gallbladder colic should be completely normal.
Cholecystitis
White blood cell (WBC) counts and measurements of aspirate aminotransferase (AST), alanine aminotransferase (ALT), bilirubin, and alkaline phosphate (ALP) may be helpful in the diagnosis of cholecystitis. However, because biliary obstruction is limited to the gallbladder in uncomplicated cholecystitis, elevation in the serum total bilirubin and ALP concentrations may not be present. Thus, the presence of normal values does not exclude cholecystitis.
A study by Singer et al examined the utility of laboratory values in acute cholecystitis diagnosed by hepatic 2,6-dimethyliminodiacetic acid (HIDA) scanning. [14] No difference was found in mean WBC counts and levels of AST, ALT, bilirubin, and ALP between patients diagnosed with cholecystitis and those without.
Mild elevation of amylase up to three times normal may be found in cholecystitis, especially when gangrene is present. A very high bilirubin should prompt the physician to pay special attention to the common bile duct and pancreatic region.
A comprehensive metabolic panel with bicarbonate may exhibit the following:
-
AST, ALT, and ALP levels may be elevated; however, as with other laboratory tests, these levels are not sensitive for excluding cholecystitis. When the AST and ALT levels are elevated significantly, a common bile duct stone is more likely.
-
An elevation of AST, ALT, or ALP measurements should raise the possibility of other biliary system pathology such as cholangitis, choledocholithiasis, or the Mirizzi syndrome.
-
Note the calcium level (Ranson criteria) if evidence of biliary pancreatitis exists.
-
Other abnormalities (eg, renal insufficiency) are not related to cholecystitis but may indicate a comorbid condition.
An elevated WBC is expected but not reliable. In a retrospective study, only 61% of patients with cholecystitis had a WBC count greater than 11,000 cells/µL. A WBC greater than 15,000 cells/µL may indicate perforation or gangrene.
Prothrombin time (PT) and activated partial thromboplastin time (aPTT) are not expected to be elevated unless sepsis or underlying cirrhosis is present. Coagulation profiles are helpful if the patient needs operative intervention.
For febrile patients, send two sets of blood cultures to attempt to isolate the organism in the presence of bacteremia from bacterial superinfection.
Although expected to be normal, urinalysis is essential in the workup of patients with abdominal pain to exclude pyelonephritis and renal calculi.
Conduct a pregnancy test for women of childbearing age.
Imaging Considerations
Ultrasonography and nuclear medicine studies are the best imaging studies for the diagnosis of both cholecystitis and cholelithiasis. Ultrasonography is usually favored as the initial test, whereas hepatobiliary scintigraphy is usually reserved for the 20% of patients in whom the diagnosis is unclear after ultrasonography has been performed.
Plain radiography, computed tomography (CT) scans, and endoscopic retrograde cholangiopancreatography (ERCP) are diagnostic adjuncts. [22] Diffusion-weighted (DW) magnetic resonance imaging (MRI) shows potential for differentiating between acute and chronic cholecystitis. [23] In a study comprising 83 patients with abdominal pain, Wang et al noted that increased signal on high b-value images were highly sensitive and moderately specific for acute cholecystitis. [23]
Ultrasonography
Ultrasonography is the most common test used in the emergency department for the diagnosis of biliary colic and acute cholecystitis (see the image below). This imaging modality may be diagnostic for biliary disease, help exclude biliary disease, or may reveal alternative causes of the patient's symptoms. Ultrasonography is 90-95% sensitive for cholecystitis and has a 78-80% specificity. [24] For simple cholelithiasis, it is 98% sensitive and specific.
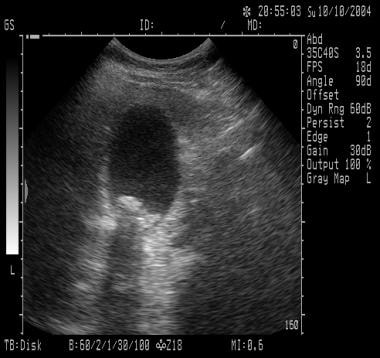 Acute Cholecystitis and Biliary Colic. The sonogram only shows gallstones within the gallbladder but no evidence of cholecystitis (ie, gallbladder wall thickening, pericholecystic fluid, common bile duct dilatation, sonographic Murphy sign).
Acute Cholecystitis and Biliary Colic. The sonogram only shows gallstones within the gallbladder but no evidence of cholecystitis (ie, gallbladder wall thickening, pericholecystic fluid, common bile duct dilatation, sonographic Murphy sign).
General ultrasonographic features
Findings include gallstones or sludge and one or more of the following conditions:
-
Gallbladder wall thickening (>2-4 mm): False-positive wall thickening found in hypoalbuminemia, ascites, congestive heart failure, and carcinoma
-
Gallbladder distention (diameter >4 cm, length >10 cm)
-
Pericholecystic fluid from perforation or exudate: May be seen as a hypoechoic or anechoic region seen along the anterior surface of the gallbladder within the hepatic parenchyma
-
Air in the gallbladder wall (indicating gangrenous cholecystitis)
-
Ultrasonographic Murphy sign: Pain elicited when the probe is pushed directly on the gallbladder (not related to breathing) [20]
Ultrasonographic Murphy sign and cholelithiasis
Some ultrasonographers recommend the diagnosis of cholecystitis if both a ultrasonographic Murphy sign and gallstones (without evidence of other pathology) are present. The combination of the Murphy sign and cholelithiasis has a high positive predictive value. [19, 20] In a study by Ralls et al involving 497 patients with suspected acute cholecystitis, the positive predictive value of the presence of stones and a positive ultrasonographic Murphy sign was 92% and that of stones and thickening of the gallbladder wall was 95%. The negative predictive value of the absence of stones combined with either a normal gallbladder wall or a negative Murphy sign was 95%. [25]
Findings with or without cholelithiasis
Additional findings in the presence or absence of gallstones may include a dilated common bile duct or dilated intrahepatic ducts of the biliary tree, which indicate common bile duct stones. In the absence of stones, a solitary stone may be lodged in the common bile duct, a location that is difficult to visualize ultrasonographically.
Advantages and disadvantages of ultrasonography
Advantages of ultrasonography include imaging of other structures (eg, aorta, pancreas, liver), identification of complications (eg, perforation, empyema, abscess), ability to be rapidly performed at the bedside and in the emergency department, and absence of radiation (important in pregnancy). (see)
Disadvantages of ultrasonography include the fact this imaging modality is operator and patient dependent, it is unable to image the cystic duct, and it has a decreased sensitivity for common bile duct stones. In addition, in the setting of concomitant acute pancreatitis, ultrasonographic findings alone are not adequate to accurately identify acute cholecystitis. [26]
Biliary Scintigraphy
Depending on the clinical setting, either ultrasonography or nuclear medicine testing is the test of choice for cholecystitis. Hepatic 2,6-dimethyliminodiacetic acid (HIDA) scans have sensitivity (94%) and specificity (65-85%) for acute cholecystitis, and they are sensitive (65%) and specific (6%) for chronic cholecystitis. Normal scans are characterized by normal visualization of gallbladder in 30 minutes. Oral cholecystography is not practical for in the emergency department setting.
HIDA and diisopropyl iminodiacetic acid (DISIDA) scans are functional studies of the gallbladder. Technetium-labeled analogues of iminodiacetic acid (IDA) or diisopropyl IDA-DISIDA are administered intravenously (IV) and secreted by hepatocytes into bile, enabling visualization of the liver and biliary tree.
With cystic duct obstruction (cholecystitis), the HIDA scan shows nonvisualization (ie, considered positive) of the gallbladder at 60 minutes and uptake in the intestine as the bile is excreted directly into the duodenum. This finding has a sensitivity of 80-90% for acute cholecystitis. Obstruction of the common bile duct causes nonvisualization of the small intestine.
The rim sign is a blush of increased pericholecystic radioactivity, tracer adjacent to the gallbladder, present in approximately 30% of patients with acute cholecystitis and in 60% with acute gangrenous cholecystitis.
Advantages and disadvantages of HIDA/DISIDA scanning
Advantages of HIDA/DISIDA scanning include assessment of function and simultaneous assessment of the bile ducts. In addition, although a gallbladder may appear normal by ultrasonography, a DISIDA scan can depict an obstructed cystic duct abnormality.
A high bilirubin (>4.4 mg/dL) can possibly decrease the sensitivity of HIDA/DISIDA scanning, and recent eating or fasting for 24 hours may possibly affects findings. In addition, these scans do not image other structures in the area.
False-negative and false-positive findings
False-negative results (filling in 30 min) are found in 0.5% of studies, and filling between 30-60 minutes is associated with false-negative rates of 15-20%.
False-positive results (10-20%) occur when the gallbladder is not visualized despite a nonobstructed cystic duct. Causes include fasting patients receiving total parenteral nutrition; severe liver disease, which leads to abnormal uptake of the tracer; cystic-duct obstruction induced by chronic inflammation; and biliary sphincterotomy, which decreases resistance to bile flow leading to excretion of the tracer into the duodenum. The specificity of the test can be improved by intravenous administration of morphine, known as morphine cholescintigraphy, which induces spasm of this sphincter, thus increasing back pressure to fill the gallbladder. [27]
Abdominal Radiography
The advantages of abdominal radiographs include their readily availability and low cost. However, abdominal radiographs have low sensitivity and specificity in evaluating biliary system pathology, but they can be helpful in excluding other abdominal pathology such as renal colic, bowel obstruction, perforation. Between 10% and 30% of stones have a ring of calcium and, therefore, are radiopaque. A porcelain gallbladder also may be observed on plain films.
Emphysematous cholecystitis, cholangitis, cholecystic-enteric fistula, or postendoscopic manipulation may show air in the biliary tree. Air in the gallbladder wall indicates emphysematous cholecystitis due to gas-forming organisms such as clostridial species and Escherichia coli.
CT Scanning
Computed tomography (CT) scanning is not the test of choice and is recommended only for the evaluation of abdominal pain if the diagnosis is uncertain. CT scans can demonstrate gallbladder wall edema, pericholecystic stranding and fluid, and high-attenuation bile. A helical CT scan with fine cuts through the biliary tract has not been well studied but may be useful.
Advantages and disadvantages of CT scanning
CT scanning not only provides better information of the surrounding structures than ultrasonography and hepatic 2,6-dimethyliminodiacetic acid (HIDA) scanning, but it is also noninvasive. For complications of cholecystitis and cholangitis, gallbladder perforation, pericholecystic fluid, and intrahepatic ductal dilation, CT scanning may be adequate.
However, CT scanning misses 20% of gallstones, because the stones may be of the same radiographic density as bile. In addition, CT scanning is also more expensive; takes longer because the patient usually has to drink oral contrast; and also, given the radiation dose, may not be ideal in the pregnant patient.
Electrocardiography
ST-segment elevations are an uncommon finding in acute cholecystitis. The pathophysiologic mechanism of these electrocardiographic changes is unclear but has been shown to be correctable with appropriate hepatobiliary management. Prompt recognition of cholecystitis will prevent the performance of unnecessary diagnostic and therapeutic cardiac interventions. [28]
Endoscopic Retrograde Cholangiopancreatography
Endoscopic retrograde cholangiopancreatography (ERCP) provides both endoscopic and radiographic visualization of the biliary tract. This modality can be diagnostic and therapeutic by direct removal of common bile duct stones.
Indications for ERCP
Ultrasonography is 50-75% sensitive for choledocholithiasis; computed tomography (CT) and hepatic 2,6-dimethyliminodiacetic acid (HIDA) scanning are not better. Therefore, when a dilated common bile duct is found or elevated liver function test results are present, suspicion should remain high for common bile duct stones, and an ERCP should be considered.
Debate exists as to when an ERCP should be performed. In general, because cholecystitis is caused by obstruction of the ducts, the risk of common bile duct stones is approximately 10%. Given its potential for complications, ERCP should be used when there is a high potential for intervention and it should not be used solely as a diagnostic modality.
Some studies have classified people as low risk for common bile duct stones based on (1) lack of jaundice, (2) elevated transaminase levels, and (3) a common bile duct diameter of less than 8 mm. In this population, the risk of common bile duct stones may be as low as 1%. In patients with any of the risk factors, the rate of stones was 39%. Therefore, in general, people with any of the risk factors for common bile duct stones should undergo operative or ERCP evaluation of the common bile duct.
Complications of ERCP
Major complications of ERCP include pancreatitis and cholangitis.
Prehospital Care of Cholecystitis
Patients with gallbladder colic or cholecystitis usually present in the prehospital setting with severe abdominal pain. Transport patients with minor symptoms to the hospital with an intravenous (IV) line in place and monitor. However, the diagnosis of cholecystitis is not a prehospital diagnosis.
In patients with severe pain (eg, differential diagnosis includes abdominal aortic aneurysm, myocardial infarction) and in patients with hypotension and/or fever who may have cholecystitis or cholangitis, prehospital care should include the following:
-
Prioritizing and immediately assessing airway, breathing, and circulation (ABCs), as with all emergencies
-
Monitoring (pulse oximetry, cardiac monitor, frequent blood pressure measurements, blood glucose measurement)
-
Stabilization (oxygen, placement of two large-bore IVs, administration of IV fluids to unstable patients)
-
Rapidly transporting
ED Management
The primary goal of emergency department care is stabilization of the patient and an expedient diagnosis.
Suspect gallbladder colic in patients with less than 4-6 hours of right upper quadrant pain that radiates to the back. Consider acute uncomplicated cholecystitis in patients with pain of longer duration and with or without low-grade fever. Severe cholecystitis can develop into sepsis or cholangitis, especially in patients with diabetes or elderly patients, in whom the diagnosis may be delayed.
After assessment of the patient's airway, breathing, and circulation (ABCs), perform the standard opening gambit of intravenous (IV) line placement, pulse oximetry measurement, oxygen administration, electrocardiography recording, and monitoring. Send for laboratory studies when the IV line is placed; include blood cultures if the patient is febrile.
Replace volume loss with normal saline, then maintenance fluids. Make patients nothing by mouth (NPO). Nasogastric suction may be needed in patients with persistent vomiting or abdominal distention.
In patients who are unstable or have severe pain, consider a bedside ultrasonographic study to exclude an abdominal aortic aneurysm and assist in the diagnosis of cholecystitis. Signs on ultrasonograms include the presence of gallstones, an ultrasonographic Murphy sign, gallbladder wall thickening, and pericholecystic fluid. Competent emergency physician-performed bedside ultrasonography for the detection of acute cholecystitis has been shown to have a negative predictive value (NPV) of 95%, which is not markedly different from radiologist-performed formal ultrasonography. [29]
Tokyo guidelines for acute cholecystitis
The Tokyo guidelines were published in 2007 and updated in 2013. They are a set of clinical and radiologic diagnostic criteria for acute cholecystitis created to address the controversy regarding the optimal criteria for clinical diagnosis. [30] Patients exhibiting one of the local signs of inflammation, such as Murphy sign (specificity, 79-96%; sensitivity, 50-60% [30] ), or a mass/pain/tenderness in the right upper quadrant, as well as one of the systemic signs of inflammation, such as fever, elevated white blood cell (WBC) count, and elevated C-reactive protein level, are diagnosed as having acute cholecystitis. [31] Imaging findings characteristic of acute cholecystitis confirm the diagnosis. [30]
Once the diagnosis of acute cholecystitis is made, it usually is treated by hospitalization. This may include medical and/or surgical therapy. Some patients may be treated as outpatients.
Medical Care
Although surgical therapy is the treatment of choice for acute cholecystitis, many patients require hospitalization for stabilization and "cooling off" of the gallbladder before surgery. However, surgical consultation is appropriate, and depending on the institution, either medicine or surgery may admit the patient for conservative care. In addition, obtain an urgent gastroenterology consultation for endoscopic retrograde cholangiopancreatography (ERCP) in patients with evidence of choledocholithiasis (ie, common bile duct stones seen on ultrasonography, dilated common bile ducts, elevated liver function test results, pancreatitis).
Medical therapy of gallbladder colic includes antiemetics and pain control. In mild cholecystitis, in which inflammation is the primary process, antibiotics are prophylactic but are usually used. In acute cholecystitis, broad-spectrum antibiotic coverage is used.
Antimicrobial therapy
Guidelines from the Surgical Infection Society and the Infectious Diseases Society of America on the management of intra-abdominal infection recommend that antimicrobial therapy be instituted when infection is suspected and the patient has either acute cholecystitis or cholangitis. The guidelines also state that in patients undergoing cholecystectomy for acute cholecystitis, antimicrobial therapy should be discontinued within 24 hours of surgery unless infection outside the gallbladder wall is suspected. [32, 33]
Antibiotics are also recommended for routine use in patients who are elderly or have diabetes or immunodeficiency and for prophylaxis in patients undergoing cholecystectomy to reduce septic complications even when infection is not suspected. [3]
Analgesia
Several studies have shown that early pain control in the emergency department in patients with abdominal pain does not hinder the diagnosis. Therefore, administer pain control early, without waiting for the diagnosis or surgical consultation. However, a courtesy call to the surgical consultant before the administration of narcotics offers the expedient opportunity to examine the patients without narcotics, which occasionally diminishes surgical resistance to prediagnosis narcotic use.
Pain control should be achieved with opiate analgesics. [34, 35, 36] In the past, morphine was generally not recommended due to concerns that it may increase the tone of the sphincter of Oddi. This has not been shown to be clinically significant. Anticholinergic antispasmodics, such as dicyclomine (Bentyl), may also be recommended in the initial management of acute biliary colic and cholecystitis for spasm.
Anti-inflammatory and antiemetic agents
Anti-inflammatory medications such as ketorolac or indomethacin have been reported to be effective in relieving pain from gallbladder distention. Because the release of prostaglandins results in gallbladder distention, inhibition of these prostaglandins may help alleviate some of the symptoms. However, these agents may not be as effective when biliary colic is complicated by infection.
In a study that evaluated the effectiveness of oral analgesics on biliary colic pain and explored the prescribing habits of community doctors, Johnson et al that little evidence exists for the extensive range of medications prescribed. [37] Of the available data, the investigators noted that nonsteroidal anti-inflammatories were the most effective for severe pain.
Antiemetics such as metoclopramide or prochlorperazine can also be used.
Surgical Management of Cholecystitis
Historically, cholecystitis was operated on emergently, resulting in increased mortality. The current practice is to cool off the gallbladder and perform a cholecystectomy after several days or to readmit the patient at a later date.
Indications for urgent surgical intervention include patients with complications such as empyema, emphysematous cholecystitis, or perforation. Emergent cholecystectomy is usually performed in 20% of such cases.
Cholecystectomy
In approximately 30% of patients with uncomplicated cholecystitis, medical therapy is not sufficient and these patients usually need cholecystectomy within 24-72 hours. Cholecystectomy may be performed after the first 48 hours or after the inflammation has subsided. Unstable patients may need more urgent intervention with endoscopic retrograde cholangiopancreatography (ERCP), percutaneous drainage, or cholecystectomy.
Laparoscopic cholecystectomy is very effective and has few complications. Approximately 5% of cases must be converted to an open cholecystectomy; in acute cholecystectomy, the conversion rate can be as high as 30%. The rate of conversion is higher for acute cholecystitis compared with uncomplicated cholelithiasis, in both acute or delayed intervention. [38, 39, 40, 41] Predictors of the need for open conversion include a white blood cell (WBC) count of more than 18,000 cells/µL at the time of presentation, a duration of symptoms longer than 72-96 hours, and an age older than 60 years. [42]
Immediate laparoscopic cholecystectomy (within 24 hours) has been increasingly performed by surgeons, because it has been shown to be safe, is not more difficult than laparoscopic cholecystectomy performed later, and shortens the hospital length of stay. [1, 43, 44, 45] Similarly, Zafar et al reported the best outcomes and lowest costs were achieved when laparoscopic cholecystectomy was performed within 2 days of presentation of acute cholecystitis. [46]
In a large randomized trial by Gutt et al, laparoscopic cholecystectomy performed within 24 hours of hospital admission was found to be superior to conservative management followed a week or more later by surgery in terms of morbidity and costs. In the study, 304 patients underwent laparoscopic cholecystectomy within 24 hours of hospital admission, while 314 patients underwent antibiotic treatment initially, with laparoscopic cholecystectomy performed after 7-45 days. The morbidity rate in the group of patients receiving immediate surgery was 11.8%, compared with 34.4% in the delayed-surgery group. [47]
High-risk patients
Patients who are not good surgical risks but who are toxic may benefit from percutaneous gallbladder drainage and placement of a cholecystostomy or T-tube if common bile duct stones are suspected. (Note that a propensity score analysis of 1996-2010 Medicare data of 8818 elderly patients [age ≥66 years] with grade III acute cholecystitis revealed an association between those who underwent cholecystostomy tube placement [n = 565; 6.4%] with lower rates of definitive treatment with cholecystectomy and higher rates of mortality and readmissions. [48] ) The alternative is ERCP to attempt endoscopic opening of the common bile duct or cystic duct.
Delayed surgical intervention can be used for patients who have high-risk medical conditions and are unstable for surgery and in patients in whom the diagnosis in doubt. Mortality may be up to 15% in patients with acute cholecystitis who were at high risk (as per Acute Physiology and Chronic Health Evaluation [APACHE] criteria). [49]
In patients younger than 60 years, the mortality rate for emergent cholecystectomy is approximately 3%, whereas mortality in early or elective cholecystectomy approaches 0.5%.
Outpatient Care
Acute cholecystitis
For some patients with acute cholecystitis to be treated on an outpatient basis, the following patient criteria must be met:
-
Afebrile and normal vital signs
-
Minimal amount of pain and tenderness
-
No markedly abnormal laboratory results, normal common bile duct on ultrasonography, and no pericholecystic fluid or biliary air
-
No underlying medical problems (eg, diabetes, cirrhosis, vascular condition, steroids), advanced age, or pregnancy
-
Next day follow-up visit
Discharge on oral antibiotics and a small number of pain medications. In pregnancy, because symptoms may be recurrent, refer women to their obstetrician/gynecologist as well as a surgeon. Second trimester cholecystectomy is the safest time period, because the risk of premature labor is lower, and the uterus does not push on the gallbladder. [50]
Biliary colic
For simple gallbladder colic, other therapies are rarely performed, because they require long-term therapy (oral dissolution), cause complications (shock-wave therapy), and ultimately do not prevent the recurrence of gallstones.
Oral dissolution therapy consists of bile acid therapy with ursodeoxycholic acid sometimes in combination with chenodeoxycholic acid. With this treatment, cholesterol saturation of bile is decreased, and dissolution of small gallstones (< 5 mm) is possible with 6-12 months of therapy; however, over 50% recur. Oral dissolution has several disadvantages, including the time frame of up to 2 years. Fewer than 10% of patients with symptomatic gallstones are candidates for this therapy. The doses are not listed, because this treatment option is chosen rarely.
Extracorporeal shock-wave lithotripsy is another little-used therapy due to the recurrence of stones. This treatment is not popular, because only small (< 2 cm) stones can be fragmented, and also a recurrence of gallstones occurs in up 30% of patients within 5 years.
Percutaneous contact dissolution therapy by injection of methyl tert-butyl ether (MTBE) into the gallbladder to dissolve stones is rarely used.
There is evidence to support early laparoscopic cholecystectomy (< 24 h of diagnosis of biliary colic) decreasing the morbidity during the waiting period for laparoscopic cholecystectomy, in addition to decreasing the rate of conversion to open cholecystectomy and the hospital length of stay. [51]
Prevention of Biliary Colic
Some literature supports dietary modification of decreased fat intake to decrease occurrence of biliary colic. Advise patients with biliary colic to refrain from eating fatty or spicy foods. They should contact their physician for persistent recurrence of pain or fever.
Complications
Gallbladder gangrene can be a complication in up to 20% of cases of cholecystitis and usually occurs in diabetics, the elderly, or immunocompromised persons.
Complications of cholecystitis and/or biliary colic may also include cholangitis, sepsis, pancreatitis, hepatitis, and choledocholithiasis (10%). In addition, gallbladder perforation occurs in 10% of patients with cholecystitis. When perforation is localized, it may be seen as pericholecystic fluid by ultrasonography. Abscess formation is common. Free perforation also can occur, releasing bile and inflammatory matter intraperitoneally, causing peritonitis.
When perforation occurs next to a hollow viscus, a gallbladder enteric fistula can be formed; fistulas into the duodenum are most common. When gallstones are passed directly through the fistula into the small bowel, if they are greater than 2.5 cm, they can obstruct the ileocecal valve, which causes gallstone ileus. Mortality in these cases can be up to 20%, because the diagnosis is difficult. Treatment includes cholecystectomy, common bile duct exploration, and closure of the fistulous tract.
Outcomes
In patients with diabetes who have biliary colic, acute cholecystitis occurs more frequently compared with the nondiabetic population. Furthermore, diabetic patients with cholecystitis are more likely experience complications. [52]
Uncomplicated cholecystitis has a low mortality; however, mortality can be as high as 15% in immunocompromised patients. In addition, complicated cholecystitis has up to a 25% mortality rate: Emphysematous gallbladder of infection by gas-forming organisms (eg, Clostridium species) is more common in patients with diabetes and men, with a 15% mortality, and gangrenous or empyema of the gallbladder carries 25% mortality. Perforation of the gallbladder occurs in 3-15% of patients with cholecystitis and is associated with a 60% mortality rate.
Special Considerations
Delay in diagnosis of acute cholecystitis can result in complications, such as gangrene and perforation, and eventually, increased morbidity and mortality. Clinicians should consider this in patient populations that may have atypical presentations, such as diabetics, the elderly, and children. Generally, all patients with a diagnosis of acute cholecystitis should be admitted to the hospital for intravenous antibiotics and scheduled for cholecystectomy within 24-72 hours.
Gallstones are more likely to be symptomatic in pregnancy. For gallbladder colic in pregnancy, because symptoms may be recurrent, women should be referred to their obstetrician as well as a surgeon. Second trimester cholecystectomy is the safest time period, because the risk of premature labor is lower, and the uterus does not push on the gallbladder.
It is uncommon for gallstone formation in children; affected children are more likely to have congenital anomalies, biliary anomalies, or hemolytic (pigment) stones.
The incidence of gallstone increases with age. Elderly patients are more likely to go from asymptomatic gallstones to serious complications of gallstones without gallbladder colic. Delays in diagnosis are common, as symptoms may be limited to change in mental status or decreased food intake. Physical examination and laboratory indexes may be normal. [21, 53]
A systematic review and meta-analysis of 8 studies comprising 592 geriatric patients (age ≥70 years) indicates that early cholecystectomy is feasible for acute cholecystitis in this population. [54] In 316 patients who underwent early laparoscopic cholecystectomy, there was a 23% conversion rate to the open procedure, 24% perioperative morbidity, and 3.5% mortality.
Acalculous cholecystitis occurs in critically ill patients and localized pain and tenderness can sometimes not be present. Patients with burns or sepsis and postoperative and trauma patients are all at risk for acalculous cholecystitis.
Clinical Practice Guidelines on the Diagnosis and Treatment of Acute Calculus Cholecystitis (WSES, 2020)
Clinical practice guidelines on the diagnosis and treatment of acute calculus cholecystitis (ACC) were updated in November 2020 by the World Society of Emergency Surgery. [55] Highlights are below. For more information, go directly to the guidelines.
Diagnosis
The suggested combination for diagnosis is a detailed history, complete clinical examination, laboratory testing, and imaging investigations. It is recommended to not rely on a single diagnostic test or clinical or laboratory finding, as none has sufficient diagnostic power to establish or exclude the diagnosis of ACC. The best combination of diagnostic investigations is not known.
The preferred initial imaging technique is abdominal ultrasonography (US). It is cost-effective, noninvasive, widely available, and accurate.
Other suggested imaging studies in select patients may include hepatobiliary iminodiacetic acid scanning, which has the highest sensitivity and specificity for ACC diagnosis compared with other imaging modalities. The accuracy of MRI is comparable to abdominal US. The accuracy of CT scanning for the diagnosis of ACC is considered poor.
Surgical Treatment
The recommended first-line treatment for ACC is laparoscopic cholecystectomy.
Laparoscopic cholecystectomy should be avoided in patients with septic shock or absolute anesthesiology contraindications.
Laparoscopic cholecystectomy is suggested to be safe and feasible in patients who have Child-Pugh A or B cirrhosis, those of advanced age (>80 years), or women who are pregnant.
If there is difficulty with anatomic identification of structures during cholecystectomy, the recommended procedure is laparoscopic or open subtotal cholecystectomy.
Conversion from laparoscopic to open cholecystectomy is recommended in patients with severe local inflammation, adhesions, bleeding from the cystohepatic (Calot) triangle, or suspected injury to the bile duct.
Timing of Cholecystectomy in ACC
If adequate surgical expertise is available, the recommended timing for early laparoscopic cholecystectomy is that it should be performed as soon as possible, within 7 days from admission to the hospital and within 10 days from symptom onset.
If early laparoscopic cholecystectomy cannot be performed in the recommended time parameters, delayed laparoscopic cholecystectomy should be performed after 6 weeks from first clinical presentation.
Alternative Treatments & Gall Bladder Drainage in Patients Not Suitable for Surgery
For patients who refuse surgery or those who are not suitable to undergo surgery, nonoperative management with best medical therapy (ie, antibiotics, observation) is suggested.
Alternative treatment options can be considered in patients in whom nonoperative management fails, those who still refuse surgery, and those who are not suitable for surgery.
Gallbladder drainage is recommended in patients with ACC who are not suitable for surgery; this procedure converts a septic patient with ACC into a nonseptic patient.
Delayed laparoscopic cholecystectomy can be offered to patients after perioperative risk is reduced; this decreases the re-admission rate for ACC relapse or gallstone-related disease.
In patients with ACC who are not suitable for surgery, alternatives to percutaneous transhepatic gallbladder drainage include endoscopic transpapillary gallbladder drainage or US-guided transmural gallbladder drainage; both are considered safe and effective alternatives if performed at a high-volume center by a skilled endoscopist.
In this select group of patients, endoscopic transmural US-guided gallbladder drainage with lumen-apposing self-expandable metal stents is preferred over endoscopic transpapillary gallbladder drainage.
Antibiotics in ACC
The routine use of postoperative antibiotics is not recommended in uncomplicated ACC when the focus of infection is controlled by cholecystectomy.
In complicated ACC, it is recommended that an antimicrobial regimen is prescribed; it should be based on the presumed pathogens involved and major resistance patterns.
In the case of complicated ACC with a high risk for antimicrobial resistance, it is recommended that the antibiotic regimen be targeted based on the results of a microbiological analysis, which ensures adequate antimicrobial coverage.
For more information, see Laparoscopic Cholecystectomy, Pediatric Cholecystitis, and Acute Cholecystitis Imaging.
For more Clinical Practice Guidelines, go to Guidelines.
Questions & Answers
Overview
What is the spectrum of biliary tract disease?
What are risk factors for biliary colic and cholecystitis?
What are risk factors for acalculous cholecystitis?
What are symptoms of biliary colic?
What are symptoms of cholecystitis?
What are symptoms of cholelithiasis?
Which physical findings suggest biliary colic and cholecystitis?
What should be included in abdominal assessment of biliary colic and acute cholecystitis?
What is the role of lab studies in the diagnosis of biliary colic and cholelithiasis?
What is the role of lab studies in the diagnosis of cholecystitis?
What is the role of imaging studies in the diagnosis of biliary colic and acute cholecystitis?
What is the role of ultrasonography in the diagnosis of biliary colic and acute cholecystitis?
Which ultrasound findings are characteristic of biliary colic and acute cholecystitis?
Which ultrasound findings are diagnostic of cholecystitis?
Which ultrasound bile duct findings suggest biliary colic and acute cholecystitis?
What is the role of HIDA/DISIDA scans in the evaluation of biliary colic and acute cholecystitis?
How often do false results occur from HIDA/DISIDA scanning in the evaluation of cholecystitis?
What is the role of abdominal radiography in the diagnosis of biliary colic and acute cholecystitis?
What is the role of CT in the diagnosis of biliary colic and acute cholecystitis?
What is the role of electrocardiography in the diagnosis of cholecystitis?
What is included in prehospital care for biliary colic or acute cholecystitis?
What are the Tokyo Guidelines for diagnosis of acute cholecystitis?
What is included in emergency department (ED) care of biliary colic or acute cholecystitis?
What is the role of medical therapy in the management of biliary colic or acute cholecystitis?
What is included in pain management in biliary colic and acute cholecystitis?
What is the role of cholecystectomy in the treatment of cholecystitis?
Which patients may be treated for acute cholecystitis in an outpatient setting?
What are treatment options for biliary colic?
How is biliary colic prevented?
What are possible complications of biliary colic and acute cholecystitis?
What is the prognosis of biliary colic and acute cholecystitis?
Which complications are more likely to occur if diagnosis of acute cholecystitis is delayed?
How are acute cholecystitis and biliary colic managed during pregnancy?
What causes biliary colic and acute cholecystitis in children?
How should biliary colic and acute cholecystitis be managed in elderly patients?
Which patients are at highest risk for acalculous cholecystitis?
-
Acute Cholecystitis and Biliary Colic. The sonogram only shows gallstones within the gallbladder but no evidence of cholecystitis (ie, gallbladder wall thickening, pericholecystic fluid, common bile duct dilatation, sonographic Murphy sign).
-
Acute Cholecystitis and Biliary Colic. Acute cholecystitis: sonogram findings. Multiple gallstones associated with gallbladder wall thickened are depicted in both longitudinal (a) and axial (b) images. Courtesy of Critical Ultrasound Journal, BioMed Central Ltd, Springer Nature (Mazzei MA, et al. The role of US examination in the management of acute abdomen. Crit Ultrasound J. 2013; 5(suppl 1): S6.)
-
Acute Cholecystitis and Biliary Colic. Admission abdominal sonogram in a patient with acute gallbladder perforation and gallstones spillage. The mass (P) surrounding the gallbladder (GB) was considered to be blood, pus or, less likely, tumorous soft tissue, not ascites. The transparent arrow indicates a stone. Courtesy of World Journal of Emergency Surgery, BioMed Central Ltd, Springer Nature (Chiapponi C, et al. Acute gallbladder perforation with gallstones spillage in a cirrhotic patient. World J Emerg Surg. 2010; 5: 11.)
Tables
What would you like to print?
- Overview
- Risk Factors
- Evaluation of Biliary Colic and Cholecystitis
- Diagnosis
- Diagnostic Tests
- Imaging Considerations
- Ultrasonography
- Biliary Scintigraphy
- Abdominal Radiography
- CT Scanning
- Electrocardiography
- Endoscopic Retrograde Cholangiopancreatography
- Prehospital Care of Cholecystitis
- ED Management
- Medical Care
- Surgical Management of Cholecystitis
- Outpatient Care
- Prevention of Biliary Colic
- Complications
- Outcomes
- Special Considerations
- Clinical Practice Guidelines on the Diagnosis and Treatment of Acute Calculus Cholecystitis (WSES, 2020)
- Questions & Answers
- Show All
- Media Gallery
- References









