Practice Essentials
Thiamine deficiency, or beriberi, refers to a lack of thiamine pyrophosphate, the biologically active form of the vitamin known as thiamine (also spelled thiamin), or vitamin B-1 (see the image below). Thiamine pyrophosphate acts as a coenzyme in carbohydrate metabolism through the decarboxylation of alpha ketoacids. It also takes part in the formation of glucose by acting as a coenzyme for the transketolase in the pentose monophosphate pathway. In suspected cases of thiamine deficiency, prompt administration of parenteral thiamine is indicated. [1] (See Treatment and Medication.)
See 21 Hidden Clues to Diagnosing Nutritional Deficiencies, a Critical Images slideshow, to help identify clues to conditions associated with malnutrition.
Thiamine is a water-soluble vitamin that is absorbed in the jejunum by 2 processes. When the thiamine level in the small intestines is low, an active transport portal is responsible for absorption. When the thiamine concentration is high, a passive mucosal process takes place. Up to 5 mg of thiamine is absorbed through the small intestines. The small intestine is where phosphorylation of thiamine takes place. [2]
The body cannot produce thiamine and can only store up to 30 mg of it in tissues. Thiamine is mostly concentrated in the skeletal muscles. Other organs in which it is found are the brain, heart, liver, and kidneys. The half-life of thiamine is 9-18 days. It is excreted by the kidney. [3, 4, 5, 6]
Persons may become deficient in thiamine by not ingesting enough vitamin B-1 through the diet or may become deficient through excess use; the latter may result from hyperthyroidism, pregnancy, lactation, or fever. Prolonged diarrhea may impair the body's ability to absorb vitamin B-1, and severe liver disease impairs its use. (See Pathophysiology, Etiology, Presentation, and Workup.) [7, 8]
Dietary thiamine
Food that are rich in thiamine are as follows [2] (see Table 1, below):
-
Whole-grain foods
-
Meat/fish/poultry/eggs
-
Milk and milk products
-
Vegetables (ie, green, leafy vegetables; beets; potatoes)
-
Legumes (ie, lentils, soybeans, nuts, seeds)
-
Orange and tomato juices
Thiamine is not present in fats or highly refined sugars and is present sparingly in cassava. Foods containing thiaminases, such as milled rice, shrimp, mussels, clams, fresh fish, and raw animal tissues, decrease absorption. [9]
Cassava is a staple in many developing countries and has been used in a variety of high-energy diets. Although it contains thiamine (0.05-0.225 mg of thiamine per 100 g of cassava, depending on the crop), the high carbohydrate load of a diet rich in cassava actually consumes more thiamine than it offers the body. This can produce a thiamine deficiency through the same mechanism observed when dextrose is administered to a person with limited supplies of the vitamin.
Table. Nutritional Needs for Specific Age Groups [10] (Open Table in a new window)
Population |
Age |
Allowance, mg/day |
Recommended Dietary Allowances (RDAs) |
||
Boys |
9-13 years |
0.9 |
Men |
>14 years |
1.2 |
Girls |
9-13 years |
0.9 |
Women |
14-18 years |
1.0 |
Women |
>19 years |
1.1 |
Pregnant/lactating women |
. . . |
1.4 |
Children |
1-3 years |
0.5 |
Children |
4-8 years |
0.6 |
Adequate Intakes (AIs) |
||
Infant |
0-6 months |
0.2 |
Infant |
7-12 months |
0.3 |
Patient education
Include education regarding Korsakoff syndrome (which arises from thiamine deficiency) for patients being treated for alcohol dependency, one of the causes of thiamine deficiency. As with any substance abuse treatment program, education needs to be combined with a serious, multidisciplinary team approach to have any chance of success.
With other causes of beriberi, once the primary problem has been addressed, an appropriate diet providing more-than-adequate thiamine levels should be adopted by the patient.
Signs and symptoms of beriberi (thiamine deficiency)
High-output cardiac failure should prompt investigation of thiamine deficiency as a cause. The same applies to neuropathic symptoms, particularly in the distal extremities.
Neurologic signs and symptoms of thiamine deficiency are as follows [11] :
-
Poor memory, irritability, sleep disturbance
-
Wernicke encephalopathy, [12] Korsakoff syndrome
-
Bilateral, symmetrical lower extremities paresthesias, burning pain
-
Muscle cramps
-
Decreased vibratory position sensation
-
Absent knee and ankle jerk
-
Muscle atrophy
-
Foot drop (late stage)
Cardiovascular signs and symptoms are as follows:
-
Tachycardia
-
Chest pain
-
Wide pulse pressure
-
Heart failure [13] (orthopnea with or without edema, warm skin due to vasodilation)
-
Hypotension, shock
-
Gastroenterologic symptoms are as follows:
-
Anorexia
-
Abdominal discomfort
-
Constipation
-
Dysphagia [14]
Infantile beriberisigns and symptoms are as follows [15] :
-
Congestive heart failure (CHF)
-
Aphonia
-
Absent deep tendon reflex
Diagnosis of beriberi (thiamine deficiency)
For practical reasons, replacing thiamine as an initial test may be most feasible. If the patient responds to treatment, it is safe to assume that a measure of thiamine deficiency was responsible for the condition.
If laboratory confirmation is needed, measure blood thiamine, pyruvate, alpha-ketoglutarate, lactate, and glyoxylate levels. Also, measure urinary excretion of thiamine and its metabolites. A scarcity of any of these chemicals strongly suggests thiamine deficiency. [16]
In conjunction with whole blood or erythrocyte transketolase activity preloading and postloading, a thiamine loading test is the best indicator of thiamine deficiency. An increase of more than 15% in enzyme activity is a definitive marker of deficiency. However, this test is expensive and time consuming; it is performed only for criterion-standard proof of deficiency.
Measure urinary methylglyoxal; also measure serum thyroid-stimulating hormone (TSH), to rule out thyrotoxicosis-induced high-output heart failure, if applicable.
Management
In suspected cases of thiamine deficiency, prompt administration of parenteral thiamine is indicated. The recommended dose is 50 mg given intramuscularly for several days. The duration of therapy depends on the symptoms, and therapy is indicated until all symptoms have disappeared. Maintenance is recommended at 2.5-5 mg per day orally unless a malabsorption syndrome is suspected.
Most outpatient care is targeted at delivering thiamine in a bioavailable form to rehabilitated patients. Clinical follow-up with measurement of thiamine diphosphate activity may be warranted if relapse or noncompliance is suspected.
Pathophysiology
When healthy individuals are deprived of thiamine, thiamine stores are depleted within 1 month. However, within a week after thiamine intake stops, healthy people develop a resting tachycardia, weakness, and decreased deep tendon reflexes; some people develop a peripheral neuropathy.
Dry beriberi
Thiamine deficiency with nervous system involvement is termed dry beriberi. [17] This presentation usually occurs when poor caloric intake and relative physical inactivity are present. The neurologic findings can be peripheral neuropathy characterized by symmetrical impairment of sensory, motor, and reflex functions of the extremities, especially in the distal lower limbs. Histologic analysis has shown that the lesions arise from a degeneration of the myelin in the muscular sheaths without inflammation.
Another presentation of neurologic involvement is Wernicke encephalopathy, [18] in which an orderly sequence of symptoms occurs, including vomiting, horizontal nystagmus, palsies of the eye movements, fever, ataxia, and progressive mental impairment leading to Korsakoff syndrome. [19, 12, 20, 21] Improvement can be achieved at any stage by the addition of thiamine, unless the patient is in frank Korsakoff syndrome. Only half of the patients treated at this stage recover significantly.
Wet beriberi
Wet beriberi is the term used for thiamine deficiency with cardiovascular involvement. The chronic form of wet beriberi consists of 3 stages. In the first stage, peripheral vasodilation occurs, leading to a high cardiac output state. This leads to salt and water retention mediated through the renin-angiotensin-aldosterone system in the kidneys. As the vasodilation progresses, the kidneys detect a relative loss of volume and respond by conserving salt. With the salt retention, fluid is also absorbed into the circulatory system. The resulting fluid overload leads to edema of the dependent extremities.
By the time significant edema occurs, the heart has been exposed to a severely high workload in order to pump the required cardiac output needed to satisfy end organ requirements. Parts of the heart muscle undergo overuse injury, which results in the physical symptoms of tachycardia, edema, and high arterial and venous pressures. These changes can lead to myocardial injury, expressed as chest pain.
A more rapid form of wet beriberi is termed acute fulminant cardiovascular beriberi, or Shoshin beriberi. The predominant injury is to the heart, and rapid deterioration follows the inability of the heart muscle to satisfy the body's demands because of its own injury. In this case, edema may not be present. Instead, cyanosis of the hands and feet, tachycardia, distended neck veins, restlessness, and anxiety occur. Treatment with thiamine causes low-output cardiac failure, because systemic vasoconstriction is reinstated before the heart muscle recovers. Support of heart function is an added requirement at this stage, and recovery is usually fairly quick and complete if treatment is initiated promptly. However, if no treatment is available, death occurs just as rapidly (within hours or days).
Etiology
Lack of thiamine intake
Lack of thiamine intake can occur via diets consisting mainly of the following:
-
Food containing a high level of thiaminases, including milled rice, raw freshwater fish, raw shellfish, and ferns
-
Food high in anti-thiamine factor, such as tea, coffee, and betel nuts
-
Processed food with a content high in sulfite, which destroys thiamine
The following diet-related factors can also cause reduced thiamine intake:
-
Alcoholic state
-
Starvation state
-
Parental nutrition without adequate thiamine supplementation [25]
Increased consumption states
Increased metabolic consumption of thiamine can result from the following:
-
Diets high in carbohydrate or saturated fat intake
-
Pregnancy
-
Hyperthyroidism [26]
-
Lactation
-
Fever - Severe infection/sepsis [27]
-
Increased physical exercise
-
Refeeding syndrome (carbohydrate metabolism is increased) [27]
Increased depletion
Increased thiamine depletion can result from the following [28] :
-
Diarrhea
-
Diuretic therapies
-
Peritoneal dialysis
-
Hemodialysis/continuous renal replacement therapy [29]
-
Hyperemesis gravidarum [19]
Loss of thiamine through renal excretion can occur with most, if not all, diuretics. It has been seen with the use of such diuretics as mannitol, acetazolamide, chlorothiazide, amiloride, and loop diuretics. [30] Thiamine loss is associated with the increase in urine flow rate, but it is not related to sodium excretion. This suggests that patients with polyuria, even if the condition is unrelated to diuretics, may benefit from thiamine supplementation.
One cross-sectional observational study showed that up to 33% of patients admitted with a diagnosis of congestive heart failure (CHF) had a thiamine deficiency due to chronic loop diuretic use, usually for more than 1 month. [31] (However, thiamine deficiency found in patients with heart failure has been present in up to 98% of patients in other studies. [2] )
Risk factors for the development of thiamine deficiency in the study's patients consisted of the following:
-
Normal renal function
-
Lack of thiamine supplementation (as little as 1.5 mg thiamine/day has been effective in the prevention thiamine deficiency)
-
Preadmission spironolactone therapy (indicating more advanced disease)
Repletion of thiamine in patients with CHF has been shown to improve left ventricular function.
Decreased absorption
The following factors can result in decreased thiamine absorption:
-
Chronic intestinal disease
-
Alcoholism
-
Malnutrition
-
Gastric bypass surgery
-
Malabsorption syndrome - Celiac and tropical sprue
-
Folate deficiency - For example, in patients undergoing chemotherapy with high-dose methotrexate
Bariatric weight-loss surgery
In a study of 59 superobese patients who underwent bariatric weight-loss surgery, Aasheim et al concluded that the risk of thiamine deficiency in the first months following a duodenal switch procedure may be higher than it is after a gastric bypass, while the risk of vitamin A and D deficiencies following duodenal switch surgery may be greater in the first year than it is after gastric bypass.
The investigators compared the vitamin status of individuals who underwent laparoscopic Roux-en-Y gastric bypass to that of patients in whom laparoscopic biliopancreatic diversion with duodenal switch was performed. [32] The investigators found that following surgery, a steeper drop in thiamine levels occurred in the duodenal switch patients than in the patients who underwent gastric bypass. In addition, mean concentrations of vitamin A and 25-hydroxyvitamin D were lower in the duodenal switch group. Follow-up examinations were conducted at 6 weeks, 6 months, and 1 year after surgery.
The term bariatric beriberi is coined from this etiology. [27]
Folate deficiency
Thiamine serves as a coenzyme (in the form of thiamine pyrophosphate) in a variety of metabolic processes. In these processes, thiamine pyrophosphate is regenerated via the donation of a proton from the reduced form of nicotinamide adenine dinucleotide (NADH).
Folic acid is essential to having enough dihydrofolate reductase to regenerate NADH from its oxidative form. This regeneration allows NADH to continue to be present to regenerate thiamine pyrophosphate without being consumed in the process.
If folic acid is deficient in cells, it causes an indirect thiamine deficiency, because thiamine is present but cannot be activated.
Infantile beriberi
Infantile beriberi occurs in infants aged 2-4 months who are fed only breast milk and whose mothers are thiamine deficient. [15, 33]
Other
A retrospective study by Nath et al indicated that obesity is a risk factor for clinical thiamine deficiency, with such deficiency found in 66 out of 400 patients with a body mass index of 35 kg/m2 or above (16.5%). [34]
Epidemiology
Occurrence in the United States
Beriberi is observed in developed nations in persons with alcoholism, people on fad diets, persons on long-term peritoneal dialysis without thiamine replacement, persons undergoing long-term starvation, or persons receiving intravenous fluids with high glucose concentration. No accurate statistics are available on the incidence of this condition.
International occurrence
Developing countries are known to have more vitamin deficiency problems in general, but there has been a lack of accurate statistics for thiamine deficiency. Beriberi has been reported among refugees who are relying on emergency food aid. [35] This is due to the lack of available micronutrition supplementation.
A study by Whitfield et al found a high incidence of thiamine deficiency in Cambodia among mothers and their young children. Using a nationally representative population sample of women of childbearing age and their young offspring, as well as an erythrocyte thiamine diphosphate concentration cutoff of under 120 nmol/L as a designation of thiamine deficiency, the investigators found such deficiency in 27% of mothers and 15% of children. Using a cutoff of under 180 nmol/L, thiamine deficiency rates reached 78% in mothers and 58% in their children. A particularly high prevalence of thiamine deficiency (38%) was found in infants aged 6-12 months (38%), as measured using the cutoff of less than 120 nmol/L. [36]
Prognosis
Beriberi can be quickly fatal or can slowly rob an individual of almost all energy for even the simplest of daily activities. However, it is one of the most easily treatable conditions, with a remarkable recovery being possible even in severe cases. Thus, the patient prognosis for beriberi is usually good, unless patients have established Korsakoff syndrome. When patients have progressed to this stage, the degree of damage is only minimally reversible.
In cases of wet beriberi, clinical improvement can be observed within 12 hours of treatment, with normalization of heart function and size occurring in 1 or 2 days. The recovery is so dramatic that treatment with thiamine is a diagnostic test, which can be used in cases of acute heart failure and insidious peripheral neuropathy.
A retrospective study by Harel et al indicated that thiamine deficiency in infancy can lead to long-term motor function problems. The study looked at children aged 5-6 years who, during the first 2 years of life, had been fed a faulty milk substitute that was deficient in thiamine, comparing them with age-matched controls. The Movement Assessment Battery for Children and the Zuk Assessment indicated that motor function difficulties existed in 56% and 59%, respectively, of the thiamine-deficient formula group, compared with 10% and 3%, respectively, of the control group. The results suggested that infantile thiamine deficiency affects gross and fine motor function, as well as balance skills. [37]
-
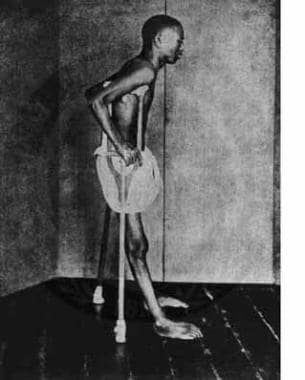
Beriberi in an adult patient.