Practice Essentials
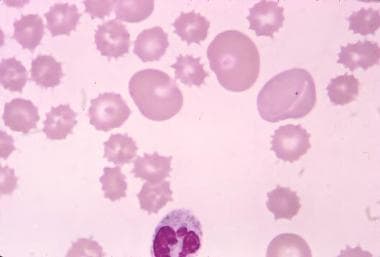
Spur cells, or acanthocytes (from the Greek word acantha, "thorn"), are erythrocytes covered with spikelike projections that vary in width, length, and distribution [1] (see image below). They are characterized by diminished deformability, which is responsible for their entrapment and destruction in the spleen. Spur cells are often confused with burr cells, or echinocytes (from the Greek word echinos, "sea urchin); however, the latter have multiple smaller projections that are uniformly distributed throughout the cell surface. A freshly prepared peripheral blood smear is essential in distinguishing between the two types of cells.
The presence of spur cells in peripheral blood (acanthocytosis) is a common feature of a heterogeneous variety of acquired and inherited disorders. Historically, spur cell anemia has been associated with advanced alcoholic liver cirrhosis, but it is also seen in other types of severe liver disease. [2] Acanthocytosis has also been associated with inherited neurologic disorders, aptly named neuroacanthocytosis syndromes. Other conditions associated with acanthocytosis include abetalipoproteinemia, McLeod phenotype, and treatment with the lung cancer drug alectinib. [3]
The diagnosis should be suspected when severe anemia requiring frequent red blood cell (RBC) transfusions occurs together with progressive liver failure, jaundice, coagulopathy, and encephalopathy. Rapid resolution of spur cell anemia has been observed after liver transplantation; therefore, early diagnosis is crucial. [2]
For discussion of this finding in pediatric patients, see Acanthocytosis. For patient education information, see Liver Disease.
Pathophysiology
The red blood cell membrane is composed of a lipid bilayer and proteins assembled in a complex manner that protects the red blood cell’s integrity and allows a bidirectional flux of electrolytes, energy, and information between the cell and its environment. [4] To preserve the red blood cell’s shape and regulate the cell’s deformability and mechanical stability, the plasma membrane is tethered to a filamentous network of proteins known as the membrane skeleton.
The lipid bilayer contains nearly equal quantities (molar ratio of 0.9-1) of unesterified cholesterol and phospholipids asymmetrically distributed between the outer and inner leaflets. Phosphatidylcholine (30% of phospholipids) and sphingomyelin (30%) are found mainly in the outer layer, whereas phosphatidylethanolamine (28%) and phosphatidylserine (14%) reside in the inner layer.
Although the cholesterol contents of the membrane are in equilibrium with the plasma free cholesterol, the uneven distribution of phospholipids is maintained by passive and active processes.
Acanthocytes can result from abnormalities in membrane lipids and proteins. Lipid alterations impact the deposition of cholesterols and phospholipids in the red cell membrane.
Acanthocytosis in severe liver disease
The formation of spur cells in severe liver disease is a two step process. First, free cholesterol in red blood cells equilibrates with abnormal lipoproteins containing a high ratio of free cholesterol to phospholipid, resulting in the preferential expansion of the outer leaflet and the development of the spur cell shape. Subsequently, remodeling by the spleen leads to the formation of acanthocytes with irregular bizarre projections. [5, 6, 7, 8, 9, 10]
A decrease occurs in polyunsaturated versus saturated and monounsaturated fatty acid content in red blood cells of patients with cirrhosis. This abnormality is more pronounced in patients with spur cell anemia, resulting in altered red blood cell shape and decreased cell fluidity.
An increase in the proteolytic activity of the erythrocyte membrane is also reported in spur cell anemia. The significance and role of this abnormality in changing the shape of the red blood cell and in hemolysis are unknown. [11]
The plasma of some patients exhibits decreased activity of lecithin cholesterol acyltransferase, resulting in increased free cholesterol in the outer layer of the red blood cell membrane as a direct consequence of its increased concentration in the plasma. After acquiring these abnormalities in the plasma, the red blood cells undergo a remodeling process in the spleen, which gives them the spheroidal shape with longer and more irregular projections.
Chorea-acanthocytosis
Alteration of band 3, the anion exchange protein, is thought to play a role in forming acanthocytes in chorea-acanthocytosis. [12] According to this hypothesis, the red blood cell shape is controlled by the ratio of the outward-facing (band 3o) and inward-facing (band 3i) conformations of band 3. Depending on this ratio, there will be contraction (leading to echinocytosis) or relaxation (leading to stomatocytosis) of the membrane skeleton. [12] Most acanthocytic disorders are associated with acquired abnormalities of the outer leaflet of the lipid bilayer. However, some rare conditions feature normal lipids and abnormal membrane proteins.
Abetalipoproteinemia
In abetalipoproteinemia, B-apoprotein–containing lipoproteins (chylomicrons, very low-density lipoproteins [VLDL], low-density lipoproteins [LDL]) are nearly absent in the plasma. Plasma cholesterol and phospholipids are decreased, with a relative increase of sphingomyelin at the expanse of lecithin. At equilibrium, the sphingomyelin concentration in the outer leaflet increases, resulting in its expansion and acanthocytosis.
McLeod phenotype
The expression of the Kell antigen (the product of a single gene on band 7q23) on red blood cells, white blood cells, and monocytes is under the control of the Kx antigen encoded for by the XK gene on band Xp21. [13] Both antigens are transmembrane proteins bound by a single disulfide bond. In the McLeod phenotype, the XK gene is deleted and the Kell antigen cannot be expressed, whereas in the Kell null phenotype, the Kell antigen is missing, and the Kx antigen is present at a normal level. The Kell null phenotype is not associated with hematologic disorders. [13]
The close proximity on the short arm of band Xp21 of the genes responsible for chronic granulomatous disease (CGD) of childhood, retinitis pigmentosa (RP), and Duchenne muscular dystrophy (DMD) explains the variable association of the McLeod phenotype with these diseases. Red blood cells from patients with chorea-acanthocytosis syndrome and McLeod phenotype do not show measurable abnormalities of the lipid bilayer. [14]
Focal membrane skeleton heterogeneity has been described as characterized by decreased compactness of the filamentous meshwork in the areas underlying the spikes. This focal weakness allows limited detachment of the lipid bilayer that does not result in membrane loss. The nature of the membrane skeleton abnormality is not known.
Etiology
Acquired acanthocytosis is associated with advanced liver disease, regardless of the primary cause. Although alcohol abuse is the most common cause of chronic liver disease in Western societies, other entities have been recognized, including nonalcoholic steatohepatitis (NASH), which may progress to cirrhosis. [15] Anorexia nervosa, hypothyroidism, and myelodysplasia are rare causes of this disorder.
Neuroacanthocytosis is the term used for acanthocytosis associated with inherited disorders. The autosomal recessive disorders abetalipoproteinemia/aprebetalipoproteinemia (chromosome 2) and chorea-acanthocytosis syndrome (band 9q21), and the X-linked McLeod phenotype are among the conditions linked to neuroacanthocytosis.
More recently, alectinib, an anaplastic lymphokinase (ALK) inhibitor used for the treatment of non–small cell lung cancer, has been associated with spheroacanthocytosis without causing significant hemolytic anemia. A notable increase in the membrane cholesterol content was observed, but no significant abnormalities were present on liver function tests. The specific abnormality induced by alectinib is unknown; it is suggested that the drug affects the cytoskeleton during erythropoiesis. [16]
Epidemiology
Spur cell anemia develops in 5% of all patients with severe liver disease. Abetalipoproteinemia is an uncommon disorder, inherited in autosomal-recessive pattern, that manifests in the first few months of life. Chorea-acanthocytosis syndrome and McLeod phenotypes are rare; only a few dozen cases have been published in the literature. Neurologic symptoms appear in patients aged 5-10 years and may progress to death in the second or third decade of life. In chorea-acanthocytosis syndrome, the median age at onset of symptoms is 32 years.
Prognosis
Spur cell hemolytic anemia in advanced liver disease indicates a poor prognosis; frequently, the condition precedes death by a few weeks to months. [17] Most patients die of gastrointestinal bleeding, hepatic encephalopathy, or sepsis.
Patients with abetalipoproteinemia develop functional deterioration early in life and do not survive beyond the third decade.
The course of chorea-acanthocytosis syndrome is slowly progressive, irreversible and, unrelenting. Death occurs within 8 -14 years of symptom onset.
-
Acanthocytes with target cells in a patient with advanced liver disease.