Overview
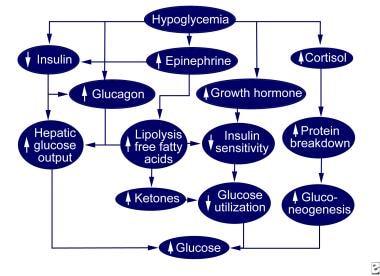
In the 1930s, Dr. Michael Somogyi speculated that hypoglycemia during the late evening induced by insulin could cause a counterregulatory hormone response (see the image below) that produces hyperglycemia in the early morning. [1]
This phenomenon is actually less common than the dawn phenomenon, which is an abnormal early morning increase in the blood glucose level because of natural changes in hormone levels. [2, 3, 4] Debate continues in the scientific community as to the actual presence of this reaction to hypoglycemia. Shanik et al, for example, suggested that the hyperglycemia attributed to the Somogyi phenomenon actually is caused by an insulin-induced insulin resistance. [5] Other proposed mechanisms of morning hyperglycemia include nocturnal growth hormone secretion and insulin resistance associated with the metabolic syndrome. [6]
The causes of Somogyi phenomenon include excess or ill-timed insulin, missed meals or snacks, and inadvertent insulin administration. [7, 8, 9] Unrecognized posthypoglycemic hyperglycemia can lead to declining metabolic control and hypoglycemic complications.
Although no data on frequency are available, Somogyi phenomenon is probably rare. It occurs in diabetes mellitus type 1 and is less common in diabetes mellitus type 2. With proper identification and management, the prognosis for Somogyi phenomenon is excellent, and there is no evidence of long-term sequelae.
Instruct patients in proper identification of symptoms of hypoglycemia, insulin dose, timing of meals, and insulin administration. For patient education information, see Insulin Reaction.
Pathophysiology
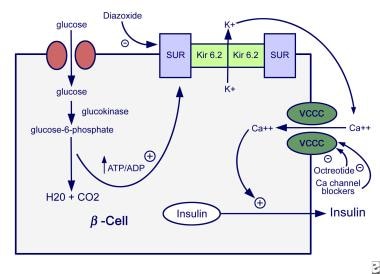
The ability to suppress insulin release is an important physiologic response that people with insulin-requiring diabetes cannot carry out, as displayed in the image below.
Defense against hypoglycemia involves counterregulatory hormones, which stimulate gluconeogenesis and glycogenolysis and counteract the anabolic effects of insulin. [5] This mechanism is dependent on an intact glucose sensor system in the CNS, pancreas, and afferent nerves. [10] Counterregulatory hormones include the following:
-
Glucagon acts on the liver to stimulate glycogenolysis and gluconeogenesis and is probably the earliest and most important hormone in the Somogyi phenomenon
-
Epinephrine increases the delivery of substrates from the periphery, decreases insulin release, stimulates glucagon release, inhibits glucose utilization by several tissues, and stimulates a warning system with sweating, anxiety, and tachycardia
-
Cortisol may aid in prolonged and severe cases of Somogyi phenomenon by blocking glucose use and stimulating hepatic glucose output
-
Growth hormones are similar to those of cortisol
Studies have cast doubt on the importance of counterregulatory hormones in mediating glycemic rebound. Hypoinsulinemia (waning of the insulin dose), insulin resistance, and hypersensitivity to the effects of the counterhormones also may play a role.
Choudhary and associates have cast further doubt on the frequency of the Somogyi effect by studying nocturnal hypoglycemia with continuous glucose monitoring. Eighty-nine patients with type 1 diabetes were studied. They compared fasting capillary glucose levels following nights with nocturnal hypoglycemia. They found that capillary fasting glucose was more likely to be lower following nocturnal hypoglycemia with only 2 instances of fasting glucose greater than 180 mgm%. They concluded that the Somogyi effect was rare and the finding of a low fasting glucose was a better indicator of nocturnal hypoglycemia. [11]
Patient History
Patients with Somogyi phenomenon present with morning hyperglycemia out of proportion to their usual glucose control. Nocturnal hypoglycemia is missed or asymptomatic, and posthypoglycemic hyperglycemia is not considered or is confused with the dawn phenomenon.
The most common cause of morning hyperglycemia is hypoinsulinemia. Patients have an increased need for insulin in the early morning primarily due to the release of growth hormone, which antagonizes insulin action. Cortisol may play a supporting role.
Patients may experience falling insulin levels due to absorption or dose issues from the previous evening. This occurs as the insulin requirement is rising (dawn phenomenon) and results in a rapid rise of blood sugar at 4-8 AM. This occurrence is common in people with either type 1 or type 2 diabetes mellitus.
Laboratory Studies
Laboratory studies for identifying Somogyi phenomenon include fasting blood glucose, nocturnal blood glucose, hemoglobin A1C (Hgb A1C), and frequent glucose sampling.
The fasting blood glucose level is expected to be inappropriately elevated due to hormonally induced rebound. A glucose reading in the middle of the night will disclose hypoglycemia as a result of insulin therapy. This will establish the diagnosis.
Obtaining an Hgb A1C level may be helpful if it is within the reference range or low despite an elevated fasting glucose level. It supports the concept of a rebound fasting hyperglycemia in the face of normal glucose control. An elevated Hgb A1C does not rule out Somogyi phenomenon.
Frequent glucose monitoring may be necessary to confirm the diagnosis and look for other periods of hypoglycemia that may lead to rebound hyperglycemia. Frequent hypoglycemia is responsible for hypoglycemic unawareness, which may cause the typical symptoms of hypoglycemia to be missed.
Treatment and Management
Somogyi phenomenon should be suspected in patients presenting with atypical hyperglycemia in the early morning that resists treatment with increased insulin doses.
If nocturnal blood sugar is confirmatory or if suspicion is high, reduce evening or bedtime insulin. Clinical signs, including weight gain, normal daytime blood sugar levels, and relatively low Hgb A1C, suggest overtreatment.
Substitution of regular insulin with an immediate-acting insulin analog, such as Humulin lispro, [12, 13] may be of some help, but this has not been firmly established.
Consider endocrine or diabetes consultation for difficult or unusual cases.
Follow-up
Continue glucose monitoring with special attention to hypoglycemia in patients with Somogyi phenomenon. Monitor weight, Hgb A1C, and fasting blood glucose levels.
-
Normal hypoglycemic counterregulation.
-
Mechanisms of insulin secretion.