Practice Essentials
Parathyroid carcinoma is an extremely rare but aggressive and life-threatening form of primary hyperparathyroidism (pHPT). Most hyperparathyroidism is caused by a single benign adenoma (approximately 85%) or by parathyroid hyperplasia or multiple adenomas. Parathyroid carcinoma accounts for less than 1% of cases of hyperparathyroidism. [1]
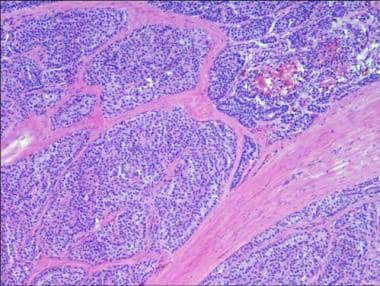 Photomicrograph of parathyroid carcinoma showing typical fibrotic septae. Histologic diagnosis can be difficult.
Photomicrograph of parathyroid carcinoma showing typical fibrotic septae. Histologic diagnosis can be difficult.
Hyperparathyroidism–jaw tumor (HPT-JT) is a rare autosomal dominant familial cancer syndrome caused by inactivating germline mutation of the Cell Division Cycle 73 (CDC73) gene. Patients with HPT-JT also have an increased risk of developing parathyroid carcinoma, ranging from 15% to 37.5% in different case series. Somatic inactivating CDC73 mutations are also strongly implicated in sporadic parathyroid carcinoma and have been found in up to 70% of such cancers. [2]
Untreated, parathyroid carcinoma leads to severe hyperparathyroidism, with signs and symptoms including hypercalcemia, bone pain, osteoporosis, fractures, and kidney stones or other kidney damage. The diagnosis is often not made prior to parathyroidectomy. This results in inadequate tumor excision and a propensity to local recurrence. Regional lymph node involvement and distant metastases are usually not present at initial diagnosis.
Recurrences may be treated by local excision or ablative (eg, radiofrequency) treatments. Death is usually caused by medically refractory hypercalcemia and seldom by tumor burden alone.
Background
The parathyroids are small endocrine glands in the neck that regulate the circulating calcium level by producing and secreting parathyroid hormone (PTH), which acts to maintain homeostasis by regulating bone mineral turnover, calcium reabsorption by the kidneys, and dietary calcium absorption from the gut. PTH production is inhibited through a feedback loop when calcium binds to calcium-sensing receptors on the parathyroid cell membrane.
Hyperparathyroidism is a state of overactive parathyroid function with excessive circulating PTH. The hyperparathyroidism seen in parathyroid carcinoma is usually severe, with high serum calcium levels, severe bone disease, and renal stones. Rarely, parathyroid cancer can be nonfunctional, that is, the tumor may not produce parathyroid hormone and the sequelae of hyperparathyroidism.
Pathophysiology
Mutations of the gene encoding CDC73 (HRPT2, 1q31.2) cause hyperparathyroidism–jaw tumor syndrome, and a high proportion (15%-37.5%) of these patients develop parathyroid cancer. Many sporadic parathyroid carcinomas also exhibit defects in this gene. [3, 4]
HRPT2 encodes a protein called parafibromin. It is thought that most parathyroid carcinomas exhibit loss of parafibromin expression. [5] Parafibromin is thought to act as a tumor suppressor gene but may have several other effects, including histone modification and activation of signaling pathways. [6] HRPT2 mutations can also be seen in benign parathyroid adenomas, but carcinomas more frequently exhibit alterations in gene copy number and have large-scale chromosomal deletions. [6]
Cyclin D1 overexpression has been associated with parathyroid carcinoma. [7] Parafibromin can negatively regulate cyclin D1 and may be responsible at least in part for this. [8]
Allelic loss of the retinoblastoma protein has been shown to be associated with parathyroid carcinoma. [9]
Mutations of the MEN1 gene can occasionally be seen in parathyroid carcinomas. [10]
Etiology
The etiology is unknown in most cases. Parathyroid cancer is associated with the genetic diseases hyperparathyroidism–jaw tumor (HPT-JT) and familial isolated hyperparathyroidism. [2, 11]
Epidemiology
Parathyroid cancer is a rare disease. Data from the National Cancer Institute’s Surveillance, Epidemiology, and End Results (SEER) program show an increasing annual incidence until approximately 2001. More recently the annual incidence has stabilized to a rate of approximately 11 cases per 10,000,000 persons. [12] Parathyroid cancer occurs in 0.5-1% of all cases of hyperparathyroidism. [1]
A large European study also demonstrated the rarity of parathyroid carcinoma, with an estimated incidence of 2 cases per 10,000,000 persons/year. [13] A nationwide Korean study found that the age-standardized incidence rose from 3.8 cases per 10,000,000 persons/year in 2003 to 6.6 cases per 10,000,000 persons/year in 2016. [14]
No known racial predilection exists. Parathyroid cancer occurs equally in males and females. [15] Males fare slightly worse in prognosis. [15, 16] Parathyroid cancer usually occurs in patients older than 30 years. Beyond that, no predominant age association has been noted.
Prognosis
Survival has varied widely in the literature, with 5-year survival ranging from 20-85% and 10-year survival from approximately 15-80%. [17, 18, 19, 20, 21, 22, 23, 15, 24, 25, 26] Data from the US National Cancer Data Base showed a 5-year survival of 82% and a 10-year survival of 66%. [27] Mortality continues after 10 years however and falls below 50% by 15 years.
Median overall survival of HPT-JT ranges from 8.9 years to 14.3 years after the date of diagnosis. Risk factors associated with shorter survival include large tumor size, older age at diagnosis, and male gender. In contrast, lymph node status or performance of radical parathyroid surgery was not found to be significant in predicting survival. [2]
Hypercalcemia is found in patients with untreated or inadequately treated parathyroid carcinoma. It is often the mechanism of death in patients with metastatic disease. Postoperative hypocalcemia can be severe because of bone hunger syndrome. In patients with severe bone disease, falling presents a serious hazard due to pathologic fractures.
Patient Education
The prognosis associated with the disease and its relationship to hypercalcemia should be discussed with the patient. The difficulty of diagnosis should be emphasized. Discuss the long-term nature of the disease even with metastases. Make patients aware that surgery is the only effective treatment against the tumor itself even though medical therapy may alleviate the hypercalcemia.
Educate the patient and family about fall prevention. This becomes increasingly important with bone disease of increasing severity.
-
Photomicrograph of parathyroid carcinoma showing typical fibrotic septae. Histologic diagnosis can be difficult.







