Background
An accurate diagnosis of pacing system malfunction(s) requires knowledge of different modes, timing cycles, and event markers, as well as newer algorithms, particularly as the number of pacemaker implants continues to grow because of newer indications. There are a few million pacemaker patients worldwide, with hundreds of thousands of new implants yearly.
Pathophysiology
The pacing system consists of a pulse generator and transvenous or epicardial lead(s) that connect the generator to the myocardium. Although true pulse generator failure is very rare, pacing system malfunction occurs occasionally. Pacing system malfunction can be due to malfunction of lead, electrode-tissue interface, or pulse generator. More complications with lead malfunction occur compared to pulse generator malfunctions. [1]
Most of these malfunctions can be corrected by simple reprogramming of the device. The majority of malfunctions are in fact due to normal programmed pacemaker function. A thorough understanding of the cause of malfunction is extremely important for accurate diagnosis and management.
Etiology
Causes of pacing system malfunction can be classified into the following groups:
-
Sensing (undersensing or oversensing)
-
Pacing (loss of capture, loss of output, failure to output)
-
Rate (inappropriate rate, pacemaker-mediated tachycardia)
-
Inappropriate lead position
-
Inappropriate mode
-
Extracardiac stimulation
-
True pulse generator failure
-
Pacemaker syndrome
-
Twiddler syndrome
A systematic review and meta-analysis comprising eight studies with a total of 14,579 leads found that leads associated with one specific manufacturer had an increased risk of abnormalities compared with leads from other manufacturers. [2] These anomalies were mostly lead noise with normal impedance, and there was a higher risk of lead reprogramming and lead revision or extraction. Leads from this manufacturer connected to generators from the same manufacturer had the highest rates of abnormalities, followed by leads from the manufacturer connected to other manufacturers' generators, and other manufacturers' leads connected to this manufacturer's generators. [2]
Undersensing
The pacing system's function of sensing is a complex process that allows the pacemaker to detect intrinsic atrial or ventricular cardiac activity based on which chamber the lead is located. True undersensing occurs when the pacemaker fails to detect native cardiac activity.
Causes of undersensing include the following:
-
Improper lead position: The lead has to be positioned at an ideal location for optimal function, otherwise it can cause undersensing.
-
Improper programming: Programming the lead sensitivity too high may cause undersensing.
-
Lead maturation or dislodgment (as shown in the image below): Lead maturation or dislodgment causes sensing and capture malfunction due to poor signal strength.
-
Lead insulation break: Insulation failure causes undersensing.
-
Loose connection at connector block (see the image below): Due to inadequate contact of the pin and connector, there is intermittent undersensing and loss of capture.
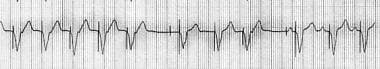
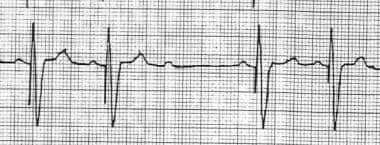
 Pacemaker Malfunction. This image shows an artifact due to monitor malfunction or a loose limb lead connection. An abrupt loss of a portion of the QRS complex followed by a flat line can be observed. If R-R intervals are matched, two QRS complexes are missing during the pause. If the artifact is due to a dislodged lead, a pacing artifact with no capture should be observed.
Pacemaker Malfunction. This image shows an artifact due to monitor malfunction or a loose limb lead connection. An abrupt loss of a portion of the QRS complex followed by a flat line can be observed. If R-R intervals are matched, two QRS complexes are missing during the pause. If the artifact is due to a dislodged lead, a pacing artifact with no capture should be observed.
-
Incompatible connector: An incompatible connector causes sensing and pacing malfunction.
-
Battery depletion: This can cause undersensing, loss of capture, or loss of output.
-
Magnet application: A magnet inhibits sensing of cardiac or noncardiac electrical events by the pacemaker; the pacemaker reverts to fixed-rate pacing function. Upon removal of the magnet, the pacemaker reverts back to the programmed routine.
-
Electromagnetic interference (EMI): EMI has several effects on pacemakers. Direct current (DC) shock causes reversion to back-up mode, transient increases in capture threshold and loss of capture, and damage to the pulse generator and circuitry. Electrocautery can inhibit the pacing stimuli or trigger ventricular pacing due to atrial oversensing. Radiotherapy can cause sensing malfunction, failure of telemetry function, and runaway pacemaker. Cellular phones may cause asynchronous pacing.
-
Reed switch malfunction: This causes pacemakers to revert to an asynchronous pacing mode with loss of sensing.
-
Dry (air) pocket in unipolar pacers: In unipolar pacers, the lead has a single stimulating electrode, the cathode, with the anode connected to an indifferent electrode, usually the outer surface of the pulse generator that has to be in constant contact with the subcutaneous tissue of the person. In dry pocket situations, there is inadequate contact between the pulse generator and the tissue, causing inappropriate sensing and pacing.
-
Circuit failure and partial open circuit: Although rare, this can cause inappropriate sensing and pacing.
-
Change in signal morphology or amplitude of the intrinsic event: This can cause either undersensing or oversensing due to signal deterioration.
-
Post defibrillation or cardioversion: DC shock causes pacemaker reversion to back-up mode, transient increases in capture threshold and loss of capture, and damage to the pulse generator and circuitry. There is also an unusual case report of cardiac resynchronization with defibrillator malfunction in which a head assembly separation occurred. [3]
-
Electrolyte abnormality such as hyperkalemia: Hyperkalemia causes both sensing and pacing malfunction due to a reduction of the electronegativity of the resting myocardial potential. There are also reports of endless loop tachycardia due to atrial channel far-field sensing of ventricular activation.
The images below illustrate undersensing.
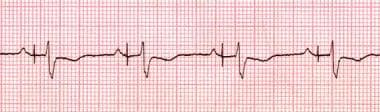 Pacemaker Malfunction. Atrial undersensing. The rhythm strip shows an atrial pacing artifact after the intrinsic P wave.
Pacemaker Malfunction. Atrial undersensing. The rhythm strip shows an atrial pacing artifact after the intrinsic P wave.
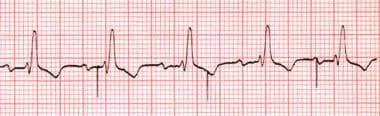 Pacemaker Malfunction. Ventricular undersensing. The rhythm strip shows ventricular pacing artifacts despite normal underlying ventricular activity.
Pacemaker Malfunction. Ventricular undersensing. The rhythm strip shows ventricular pacing artifacts despite normal underlying ventricular activity.
Oversensing
Oversensing occurs when the pacemaker detects inappropriate electrical activity as appropriate intrinsic cardiac activity.
Causes of oversensing are discussed below.
Pacemaker crosstalk: Pacemaker generated electrical event in one chamber is sensed by the lead in another chamber, which results in inappropriate inhibition of pacing artifact in the second chamber. Crosstalk is only seen in dual chamber or biventricular pacemakers. Also called crosstalk inhibition, far-field sensing, or self-inhibition. Note the following:
-
Crosstalk is more common in unipolar systems due to a larger pacing spike.
-
Crosstalk can occur in the pulse generator circuit itself.
-
Crosstalk is seen rarely with the current dual chamber pacemakers due to the ventricular blanking period, which coincides with the atrial stimulus to prevent ventricular channel oversensing of atrial output, bipolar leads with smaller pacing spikes, and steroid eluting leads with lower pacing thresholds.
-
Causes of crosstalk include atrial lead dislodgment into the ventricle, ventricular lead dislodgment into the atrium, high atrial output current, high ventricular sensitivity, and short ventricular blanking period.
-
Treatment includes decreasing atrial pacing output, decreasing atrial pulse width, decreasing ventricular sensitivity, increasing the ventricular blanking period, activating ventricular safety pacing, and implanting a new atrial lead if insulation failure mandates unipolar programming.
Electromagnetic interference (EMI): (See the discussion above in the Undersensing section.)
Improper programming: Programming the lead sensitivity too low may cause oversensing.
Myopotential inhibition: Oversensing of the skeletal muscle electrical activity causes temporary inhibition of the pacemaker with no pacing current.
Noise from pacemaker lead fracture: Due to oversensing of the lead noise, there is inappropriate inhibition of the pacemaker.
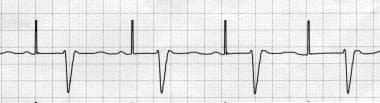
The following image illustrates oversensing.
 Pacemaker Malfunction. This is a typical example of ventricular oversensing with inhibition of ventricular pacing. In ventricular noncapture, a ventricular pacing artifact should be present after the third P wave.
Pacemaker Malfunction. This is a typical example of ventricular oversensing with inhibition of ventricular pacing. In ventricular noncapture, a ventricular pacing artifact should be present after the third P wave.
Loss of capture (noncapture)
Loss of capture, also known as noncapture, occurs when there is failure of the pacing system to produce electrical activation and myocardial contraction. Diagnosis is made when the presence of an electrical stimulus is not followed by the expected P wave or QRS complex.
Causes of loss of capture include the following:
-
Dry (air) pocket in unipolar pacer
-
Circuit failure
-
Impending battery depletion
-
Inadequate programmed output with higher threshold
-
Insulation break
-
Partial conductor coil fracture
-
Lead maturation, dislodgment, or perforation
-
Poor or incompatible connection at the connector block
-
Conditions that increase the capture threshold (eg, metabolic and electrolyte abnormalities, medications, myocardial infarction) [4]
The images below illustrate loss of capture.
 Pacemaker Malfunction. Ventricular noncapture. The rhythm strip shows atrial (P wave) sensing followed by a ventricular spike, which failed to capture the ventricle.
Pacemaker Malfunction. Ventricular noncapture. The rhythm strip shows atrial (P wave) sensing followed by a ventricular spike, which failed to capture the ventricle.
 Pacemaker Malfunction. Loss of atrial capture. The rhythm strip shows intermittent loss of atrial capture.
Pacemaker Malfunction. Loss of atrial capture. The rhythm strip shows intermittent loss of atrial capture.
Loss of output (no pacer artifact and no QRS)
Causes of loss of output include the following:
-
Dry (air) pocket in unipolar pacer
-
Circuit failure
-
Impending battery depletion
-
Inadequate programmed output with higher threshold
-
Insulation break
-
Partial conductor coil fracture
-
Lead maturation, dislodgment, or perforation
-
Poor or incompatible connection at connector block
Failure to output
Causes of failure to output include the following:
-
Crosstalk inhibition due to oversensing
-
Total battery depletion
-
Conductor coil fracture
-
Lead fracture
-
Loose set screw
-
Incompatible lead or header
-
Open circuit (characterized as the lack of a complete circuit due to lead fracture or inadequate lead attachment to the generator)
-
Internal insulation break in bipolar lead
-
Myopotential inhibition or far-field sensing
Inappropriate rate
Causes of inappropriate rate include the following:
-
Battery depletion
-
Oversensing
-
Runaway pacemaker (a rare but life-threatening condition characterized by tachycardia, sometimes above physiologic rates, most commonly due to battery depletion)
-
Undersensing
-
Pacer reset (reprogramming of the pacemaker to an asynchronous or inhibited mode, which can be caused by an external magnet, magnetic resonance imaging [MRI], ionic radiation, electrocautery, or cardioversion)
Inappropriate lead position
Causes of inappropriate position include the following:
-
Left ventricle (LV) position of the transvenous lead through an atrial septal defect (ASD), patent foramen ovale (PFO), or interventricular septal perforation, or an inadvertent position through the arterial system
-
Coronary sinus or gastric vein position instead of the right ventricle (RV)
-
Left atrial position of atrial lead through an ASD or PFO
Inappropriate mode
Causes of inappropriate mode include the following:
-
Magnet application
-
Battery depletion
-
Power-on reset
-
Noise reversion
-
Programmed mode switch such as VVIR or DDIR during supraventricular tachycardia
Extracardiac stimulation
Causes of extracardiac stimulation include the following:
-
Phrenic nerve stimulation from an atrial lead or a dislodged ventricular lead
-
Diaphragmatic stimulation from an RV lead perforation or high output
-
Pocket stimulation from insulation break or upside down pacer in a pocket
True pulse generator failure
Causes of true pulse generator failure include the following:
-
Battery depletion
-
Direct trauma
-
Circuit or component failure
-
Electromagnetic interference (EMI) because of cardioversion, defibrillation, electrocautery, lithotripsy, radiofrequency ablation, MRI, electroconvulsive therapy, therapeutic radiation, or lightning
Pacemaker-mediated tachycardia (PMT)
PMT (see image below) is observed in dual-chamber pacemakers with DDD, VDD, and DDDR modes. Causes of PMT include endless-loop tachycardia, maximum tracking rate during atrial arrhythmias, sensor-driven tachycardia, myopotential tracking, and runaway pacemaker.
 Pacemaker Malfunction. Pacemaker-mediated tachycardia. The rhythm strip shows ventricular pacing at 110 beats per minute (programmed maximal track rate).
Pacemaker Malfunction. Pacemaker-mediated tachycardia. The rhythm strip shows ventricular pacing at 110 beats per minute (programmed maximal track rate).
Note the following:
-
The classic form of PMT is endless-loop tachycardia (ELT). Usually, ELT is initiated by a premature ventricular beat. The atrial channel senses the retrograde atrial activation from the premature ventricular contraction (PVC), and the ventricular channel paces the ventricle after the programmed atrioventricular (AV) delay, which again is sensed by the atrial channel after retrograde ventriculoatrial (VA) conduction and results in ELT.
-
Conditions that initiate ELT include any condition that can result in AV dissociation, such as atrial noncapture, atrial oversensing, atrial undersensing, long AV interval, and magnet application and removal.
-
Measures to prevent PMT include a long postventricular atrial refractory period (PVARP), short AV delay, post-PVC PVARP extension, and a high maximum tracking rate.
-
Termination of PMT (see the image below): Magnet application results in loss of sensing and termination of the tachycardia. PVARP extension and withholding ventricular channel output also terminate PMT.
Pacemaker syndrome (PS)
PS is usually observed with ventricular pacing (eg, usually VOO, VVI, VVIR modes and, sometimes, VDD mode) because of atrial contraction against the closed AV valves during ventricular pacing. Note the following:
-
PS can occur in any other pacing mode where AV dyssynchrony occurs.
-
The reported incidence of PS varies from 5% to 20%, depending on the severity of symptoms.
-
Most common symptoms include pulsation and fullness in the neck, dizziness, palpitations, and near syncope.
-
Treatment involves upgrading the pacemaker to a dual-chamber pacing system.
Twiddler syndrome
Twiddler syndrome refers to patient manipulation of the pulse generator within the pocket, resulting in coiling of the lead, lead dislodgment, or rotation and/or reversal of the anterior and posterior surfaces of the pulse generator. Note the following:
-
Treatment includes uncoiling the lead, a new lead implant, and repositioning of the pulse generator.
-
Educate patients not to manipulate the pacing system.
Epidemiology
Maisel reported a pacemaker generator failure rate of 0.46% based on US Food and Drug Administration reports, [5] as well as 1.3 malfunctions per 1000 person-years based on device registries. [6] The actual incidence of pacemaker malfunction, however, is estimated to be higher as these numbers are exclusive of lead failure. Hauser et al reported a 2% device electronic failure rate at their center. [7]
The global incidence of pacemaker malfunction is unknown and difficult to determine given inconsistent definitions and the absence of a comprehensive reporting system.
Prognosis
Prognosis of pacemaker malfunction depends on the underlying cause of the pacemaker failure. Most of the pacing system malfunctions are benign and can be corrected with appropriate reprogramming.
Morbidity/mortality
Overall morbidity and mortality depend on the underlying cause of the pacemaker malfunction as well as the patient's dependency on the pacemaker. Most pacing system malfunctions are benign, although conditions such as crosstalk inhibition or runaway pacemaker can be life threatening. Maisel reported a 1 in 75,000 death rate among pacer implants. [6]
Complications
Complications during pulse generator change and lead insertion or extraction include the following:
-
Vascular injury
-
Venous thrombosis
-
Cardiac tamponade
-
Hemothorax
-
Pneumothorax
-
Cardiac perforation
-
Right ventricular avulsion
-
Bleeding
-
Infection: The rate of infection has been widely debated. Johansen et al studied the incidence of pacemaker infection and its associated risk factors and found the overall risk of infection after pacemaker implantation was low. [8] However, the rate of infection is higher as more operations are performed, and this should be taken into consideration.
Patient Education
At the time of device implantation, educate patients regarding postimplantation care. Additionally, periodically remind patients about signs and symptoms that may be related to pacing system malfunction and would warrant medical attention.
Patient education is needed for optimal pacemaker function and early diagnosis of malfunction and includes the following:
-
Advise patients not to manipulate the pulse generator to prevent twiddler syndrome.
-
Advise patients not to operate digital cellular phones close to the pulse generator to avoid inappropriate inhibition from oversensing.
-
Advise patients to seek medical attention for any unusual symptoms, such as dizziness, palpitations, and syncope, as well as for any pain, swelling, or drainage from the pacemaker area.
-
Pacemaker Malfunction. Atrial undersensing. The rhythm strip shows an atrial pacing artifact after the intrinsic P wave.
-
Pacemaker Malfunction. Ventricular undersensing. The rhythm strip shows ventricular pacing artifacts despite normal underlying ventricular activity.
-
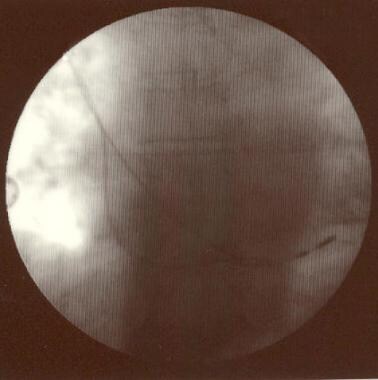
Pacemaker Malfunction. Atrial lead dislodgment. The chest radiograph film detail shows a dislodged atrial lead with the tip in the right ventricular cavity.
-
Pacemaker Malfunction. Ventricular noncapture. The rhythm strip shows atrial (P wave) sensing followed by a ventricular spike, which failed to capture the ventricle.
-
Pacemaker Malfunction. Loss of atrial capture. The rhythm strip shows intermittent loss of atrial capture.
-
Pacemaker Malfunction. Pacemaker-mediated tachycardia. The rhythm strip shows ventricular pacing at 110 beats per minute (programmed maximal track rate).
-
Pacemaker Malfunction. Termination of pacemaker-mediated tachycardia (PMT). Automatic postventricular atrial refractory period (PVARP) extension terminated the PMT.
-
Pacemaker Malfunction. This image shows an artifact due to monitor malfunction or a loose limb lead connection. An abrupt loss of a portion of the QRS complex followed by a flat line can be observed. If R-R intervals are matched, two QRS complexes are missing during the pause. If the artifact is due to a dislodged lead, a pacing artifact with no capture should be observed.
-
Pacemaker Malfunction. This is a typical example of ventricular oversensing with inhibition of ventricular pacing. In ventricular noncapture, a ventricular pacing artifact should be present after the third P wave.