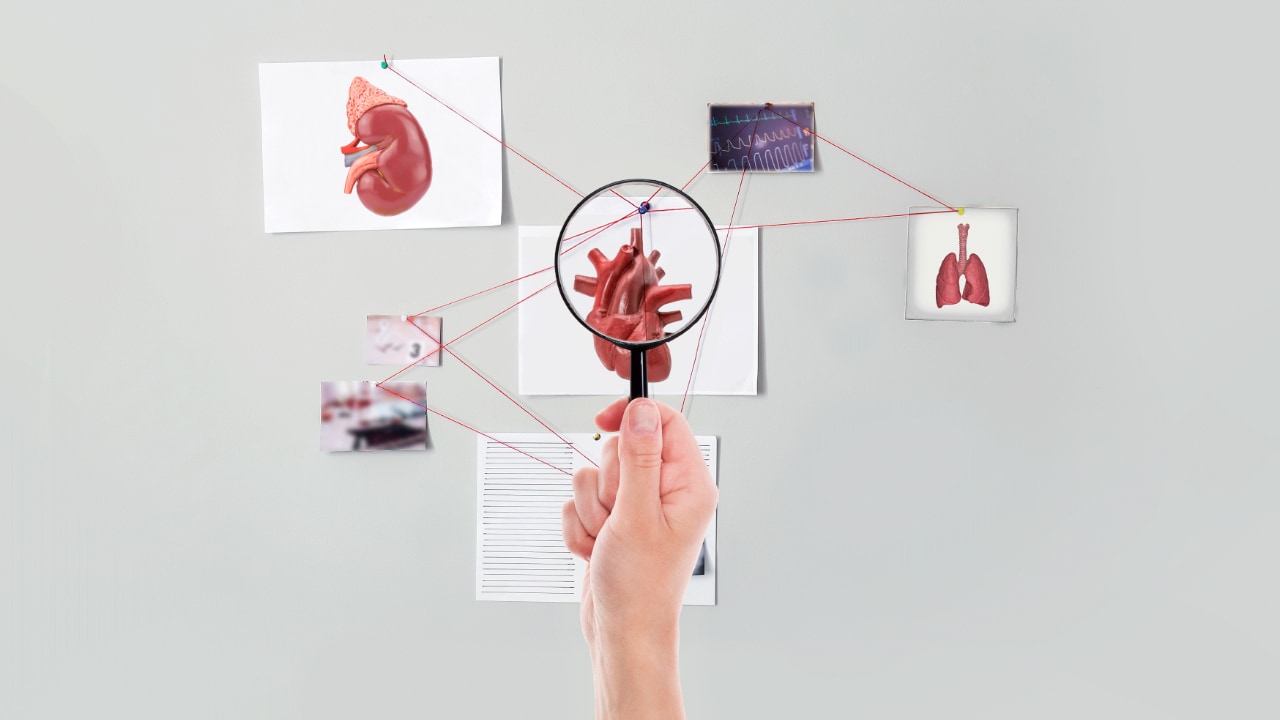
Practice Essentials
Mitral valve prolapse (MVP) is the most common valvular abnormality, affecting approximately 2-3% of the population in the United States. [1] MVP usually has a benign course, but it occasionally leads to serious complications, including clinically significant mitral regurgitation (MR), infective endocarditis, sudden cardiac death, and cerebrovascular ischemic events. [2]
Signs and Symptoms
Most patients with MVP are asymptomatic. Symptoms are related to one of the following:
-
Progression of MR
-
An associated complication (ie, stroke, endocarditis, or arrhythmia)
-
Autonomic dysfunction (The association between autonomic dysfunction and MVP remains unconfirmed.)
Symptoms related to the progression of MR include the following:
-
Fatigue
-
Dyspnea
-
Exercise intolerance
-
Orthopnea
-
Paroxysmal nocturnal dyspnea (PND)
-
Progressive signs of chronic heart failure (CHF)
-
Palpitations (from associated arrhythmias)
Symptoms related to autonomic dysfunction are usually associated with genetically inherited MVP and may include the following:
-
Anxiety
-
Panic attacks
-
Arrhythmias
-
Exercise intolerance
-
Palpitations
-
Atypical chest pain
-
Fatigue
-
Orthostasis
-
Syncope or presyncope
-
Neuropsychiatric symptoms
Common general physical features associated with MVP include the following:
-
Asthenic body habitus
-
Low body weight or BMI
-
Straight-back syndrome
-
Scoliosis or kyphosis
-
Pectus excavatum
-
Hypermobility of the joints
-
Arm span greater than height (which may be indicative of Marfan syndrome)
The classic auscultatory finding is a mid-to-late systolic click. It may or may not be followed by a high-pitched, mid-to-late systolic murmur at the cardiac apex. These can vary with the following maneuvers:
-
A Valsalva maneuver or having the patient stand result in an earlier click, closer to the first heart sound, and a prolonged murmur. It may even bring out a murmur when none is heard at rest.
-
The supine position, especially with the legs raised, results in a click later in systole and a shortened murmur.
See Presentation for more detail.
Diagnosis
Findings on echocardiography are as follows:
-
Classic MVP: The parasternal long-axis view shows greater than 2-mm superior displacement of the mitral leaflets into the left atrium during systole, with a leaflet thickness of at least 5 mm.
-
Nonclassic MVP: Displacement is more than 2 mm, with a maximal leaflet thickness of less than 5 mm.
Other echocardiographic findings that should be considered as criteria are leaflet thickening, redundancy, annular dilatation, and chordal elongation.
See Workup for more detail.
Management
For purposes of treatment, patients with MVP can be divided into the following categories:
-
Asymptomatic patients with minimal disease
-
Patients with symptoms of autonomic dysfunction
-
Patients with evidence of progression to severe MR
-
Patients with neurologic findings
Treatment measures for asymptomatic patients with minimal disease
-
Reassurance of the benign prognosis
-
Initial echocardiography for risk stratification: If no clinically significant mitral regurgitation and thin leaflets are observed, clinical examinations and echocardiographic studies can be scheduled every 3-5 years; otherwise, high-risk features warrant annual echocardiograms.
-
Encouragement to pursue a normal, unrestricted lifestyle with vigorous exercise
Treatment measures for patients with symptoms of autonomic dysfunction
-
Different measures that may be aimed at orthostatic intolerance
-
Abstinence from stimulants such as caffeine, alcohol, and cigarettes
-
An ambulatory 24-hour Holter monitor may be useful for detecting supraventricular and/or ventricular arrhythmias.
Treatment measures for patients with evidence of or progression to severe MR
-
Close follow-up and consideration for surgical referral weighing the reparability of the lesion and signs of ventricular dysfunction (eg, enlarged ventricular dimensions, presence of atrial fibrillation, or pulmonary hypertension)
-
Treadmill stress test for exercise tolerance if the physician is unsure the patient is asymptomatic
Treatment measures for patients with central neurologic findings
-
Atrial fibrillation should be actively sought (cryptogenic stroke evaluation). If not found, antiplatelet therapy with clopidogrel or aspirin may be considered for risk factor modification.
-
Cessation of smoking and oral contraceptive use
-
According to general atrial fibrillation guidelines, appropriate anticoagulant treatment should be considered for patients with atrial fibrillation and a history of stroke/transient ischemic attack (TIA).
See Treatment and Medication for more detail.
Background
Mitral valve prolapse (MVP) is the most common valvular abnormality, affecting approximately 2-3% of the population in the United States. [3, 4] It is generally defined as the systolic displacement of one or more abnormally thickened, redundant mitral leaflet(s) into the left atrium during systole. [5] It may be familial or sporadic, with the majority of data favoring an autosomal dominant inheritance pattern in a large proportion of individuals with MVP. [6, 7] It is also the most common cause of isolated mitral regurgitation (MR) requiring surgical repair. [8]
MVP usually results in a benign course. However, it occasionally leads to serious complications, including clinically significant MR, infective endocarditis, sudden cardiac death, and cerebrovascular ischemic events.
Pathophysiology
Mitral valve prolapse (MVP) is characterized primarily by myxomatous degeneration of the mitral valve leaflets. In younger populations, there is gross redundancy of both the anterior and posterior leaflets and chordal apparatus. This is the extreme form of myxomatous degeneration, known as Barlow syndrome. In older populations, however, MVP is characterized by fibroelastic deficiency, sometimes with superimposed chordal rupture due to a lack of connective tissue support. These anatomic abnormalities result in malcoaptation of mitral valve leaflets during systole, resulting in regurgitation. Mitral annular dilatation may also develop over time, resulting in further progression of mitral regurgitation (MR). Acute severe MR results in congestive heart failure symptoms without left ventricular dilatation. Conversely, chronic or progressively severe MR can lead to ventricular dilatation and dysfunction, neurohormonal activation, and heart failure. Elevation in left atrial pressures can result in left atrial enlargement, atrial fibrillation, pulmonary congestion, and pulmonary hypertension. [9]
Myxomatous proliferation is the most common pathologic basis for MVP, and it can lead to myxomatous degeneration of the loose spongiosa and fragmentation of the collagen fibrils. Disruption of the endothelium may predispose patients to infectious endocarditis and thromboembolic complications. However, most patients with MVP have only a minor derangement of the mitral valve structure that is usually clinically insignificant.
Etiology
Mitral valve prolapse (MVP) usually occurs as an isolated entity. It also commonly occurs with heritable disorders of connective tissue, including Marfan syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta, and pseudoxanthoma elasticum. [1, 10] MVP has also been described in association with a secundum atrial septal defect and hypertrophic cardiomyopathy. (Also see Presentation.)
Epidemiology
United States data
Mitral valve prolapse (MVP) is thought to be inherited with increased gene expression in female individuals (2:1). The most common form of inheritance is autosomal dominant, but X-linked inheritance has been described. [11]
MVP commonly occurs with heritable connective tissue disorders, [2] including Marfan syndrome, Ehlers-Danlos syndrome, osteogenesis imperfecta, and pseudoxanthoma elasticum. In fact, 75% of patients with Marfan syndrome have MVP due to the increased redundancy of the mitral leaflets and apparatus that occurs due to myxomatous degeneration.
MVP was overdiagnosed in the 1970s and 1980s because of the absence of rigorous echocardiographic criteria, with a reported prevalence of 5-15%. Subsequently, Levine et al reported that the two-dimensional echocardiographic characterizations of prolapse, especially on the parasternal long-axis view, are most specific for diagnosing MVP. The use of these criteria prevents overdiagnosis.
Data from the community-based Framingham Heart Study demonstrated that MVP syndrome occurred in only 2.4% of the population.
Age- and sex-related demographics
MVP has been observed in individuals of all ages.
The prevalence of MVP was similar for men and women in the Framingham Heart Study. [3] However, in the Olmsted County population, women were diagnosed more often than men and at a younger age. [12] Complications related to MVP, however, are reported more frequently in men. [13] In a study from the Mayo Clinic, women presented more commonly with anterior and bileaflet prolapse, fewer flail leaflets, and less mitral regurgitation than men. [14] They also undergo mitral surgery less often than men and exhibit excess long-term mortality but equivalent survival after valve surgery compared to men. [14]
Prognosis
Mitral valve prolapse (MVP) has a widely varying prognostic spectrum, although most patients with MVP remain asymptomatic and have a near-normal life expectancy. Approximately 5-10% of patients with MVP progress to severe mitral regurgitation (MR). [15, 16] Overall, young patients (age < 50 years) with normal left ventricular function and no symptoms tend to have excellent survival with medical treatment, even those with severe MR. [12, 17]
Morbidity/mortality
Most patients with MVP are asymptomatic and have a benign prognosis, with survival rates similar to those of the general population. Nonetheless, high-risk patients (ie, those with moderate-to-severe MR and reduced left ventricular systolic function) have increased cardiac morbidity and mortality rates.
In a community-based study of 833 individuals diagnosed with asymptomatic MVP who had longitudinal follow-up in Olmsted County, Minnesota, the best predictors for cardiac mortality were the presence of MR and left ventricular dysfunction at the time of diagnosis. [18] The study also identified certain risk factors for cardiac morbidity (defined as the occurrence of heart failure, thromboembolic events, atrial fibrillation, or need for cardiac surgery), including age older than 50 years, left atrial enlargement, the degree of regurgitation, the presence of a flail leaflet, and the presence of atrial fibrillation at the time of the baseline echocardiogram. [18]
Complications
Complications of mitral valve prolapse include the following:
-
MR, most concerning being severe MR
-
Infective endocarditis
-
Cerebrovascular ischemic events
-
Sudden cardiac death and arrhythmias
Mitral regurgitation (MR)
MR is the most common complication of MVP and the leading cause of isolated MR requiring mitral valve surgery in the United States. Acute severe MR is most frequently due to rupture of the chordae tendineae.
The risk of MR increases with the following factors: age older than 50 years, male sex, history of hypertension, increased body mass index (BMI), increased mitral valve thickness or redundancy, and left atrial and left ventricular dilatation.
In a Mayo clinic series, MR volume increased by more than 8 mL in 51% of 74 patients with MVP over a follow-up period of 1.5 years. [19] Progression of the valvular lesions and an increase in mitral annular diameter were the two independent predictors of regurgitant volume over time. [19] MR diagnosed on the basis of the presence of a systolic murmur is associated with an increased risk of adverse events, including progressive valve dysfunction, [20, 21, 22] infective endocarditis, [20, 23] and sudden death. [24, 25]
Infective endocarditis
The main mechanism for an increased risk of infective endocarditis is a turbulent flow state due to leaflet thickness or redundancy and MR. The risk of endocarditis increases 3- to 8-fold with MVP. The risk of developing infective endocarditis is higher if a systolic murmur of MR is present. [26]
The main predictors of infective endocarditis are age older than 50, male sex, history of hypertension, increased BMI, left atrial and ventricular enlargement, and increased mitral valve thickness or redundancy.
In a systematic review of 287 patients undergoing surgery for native valve endocarditis at the Mayo Clinic, MVP was present in 43% of patients and was an independent risk factor for the development of endocarditis. [27]
Cerebrovascular ischemic events
There is only a weak relationship between MVP and stroke. In a study of 777 patients with MVP who were followed for a mean period of 5.5 years, ischemic neurologic events occurred in 4% (n = 30). [28] The risk was significantly increased compared to the expected rate in the community. However, the risk was nondetectable in patients with MVP without leaflet thickening but high after either atrial fibrillation or cardiac surgery. [28] Other studies on MVP have found no relationship between MVP and cerebral events. [3] Gilon et al described the lack of an association between MVP and stroke in 213 young patients. [29]
The potential mechanisms for stroke in patients with MVP are related to the prevalence of other risk factors, primarily atrial fibrillation, which may be paroxysmal or asymptomatic. Other hypothesized mechanisms include the formation of platelet fibrin thrombi on the denuded, damaged myxomatous valves resulting in embolization. Data suggest that the prevalence of this mechanism is based on the degree of MR. Abnormal platelet function has also been reported in some studies, [30] although this has been questioned as platelet aggregates on pathology are uncommon.
The major risk factors for cerebrovascular events include age older than 50 years, thickened mitral valve leaflets, atrial fibrillation, and a need for mitral valve surgery.
Sudden cardiac death (SCD) and arrhythmias
There is a 50-60% increased risk of atrial and ventricular arrhythmias in patients with myxomatous MVP; the risk of sudden death is 0.4-2% in these patients. [31, 32, 33] The SCD risk is increased when patients have evidence of left ventricular dilatation and dysfunction, severe MR, or increased mitral leaflet thickness or redundancy.
A clinical syndrome of bileaflet MVP syndrome has been described as a clinical syndrome characterized by myxomatous bileaflet MVP, T-wave inversion in the inferolateral electrocardiograph (ECG) leads, and complex ventricular ectopy (arising from one or both of the papillary muscles), most often observed in young women. [34] In a registry study of 650 adults younger than 40 years with SCD, 43 patients were identified with MVP, comprising 7% of all patients with SCD. [35] Bileaflet involvement was seen in 70%. All patients had left ventricular fibrosis at the level of the papillary muscle on histology, and 88% had inferobasal fibrosis. ECGs for 12 of those patients showed a right bundle-branch block. [35] Factors cited as increasing the risk for life-threatening ventricular arrhythmias include bileaflet MVP, female sex, and frequent ventricular ectopy. [34]
In the presence of QT prolongation and frequent ventricular ectopy, especially nonsustained ventricular or sustained ventricular tachycardia, an electrophysiologic study may be indicated to quantitate the risk of inducible ventricular tachycardia and/or ventricular fibrillation and sudden arrhythmic death.
Patient Education
Patients with mitral valve prolapse (MVP) should receive education regarding their prognosis and the signs and symptoms of disease progression.
Of emphasis, most patients with MVP have a benign course. Still, the risk of ruptured chordae tendinae and/or clinically significant mitral regurgitation, infective endocarditis, embolic transient ischemic attack or stroke, and rare sudden death must also be discussed.
-
Mitral Valve Prolapse. Three-dimensional (3D) transesophageal echocardiogram (TEE) image (surgeon's view) of the mitral valve demonstrating prolapse of the P1 and P2 scallop (annotated in red). Ruptured chords are also visualized.