Background
Leprosy is a chronic infection caused by the acid-fast, rod-shaped bacillus Mycobacterium leprae. Leprosy can be considered 2 connected diseases that primarily affect superficial tissues, especially the skin and peripheral nerves. Leprosy is suspected to be transmitted via droplets from the nose and mouth after prolonged close contact with someone. [1] Initially, a mycobacterial infection causes a wide array of cellular immune responses. These immunologic events elicit the second part of the disease, peripheral neuropathy, with potentially long-term consequences.
The social and psychological effects of leprosy and its highly visible debilities and sequelae (as seen in the image below) have resulted in a historical stigma associated with leprosy. To minimize the prejudice against those with leprosy, the condition is also known as Hansen disease, named after G.A. Hansen, who is credited with the 1873 discovery of M leprae. This mycobacterium grows extremely slowly but has been successfully cultured in vitro using Dubos-Lowenstein-Jensen medium and thyroxine sodium. [2]
 Hands with Z-thumbs, clawing, contractures, and shortening of fingers due to repetitive injury and healing. Ho Chi Minh City, Vietnam. Courtesy of D. Scott Smith, MD.
Hands with Z-thumbs, clawing, contractures, and shortening of fingers due to repetitive injury and healing. Ho Chi Minh City, Vietnam. Courtesy of D. Scott Smith, MD.
In the 1990s, the World Health Organization (WHO) launched a campaign to eliminate leprosy as a public health problem by 2000. Elimination, as defined by the WHO, meant a reduction of patients with leprosy requiring multidrug therapy to fewer than 1 per 10,000 population. This goal was achieved in terms of global prevalence by 2002 and, as of 2015, had been maintained. As of 2015, none of the 122 countries where leprosy was endemic in 1985 still have prevalence rates of greater than 1 per 10,000 population. [3] However, in 2019, much of the disease burden of leprosy was concentrated in India, Brazil, and Indonesia, with India alone accounting for over 79% of cases worldwide as of 2018. [1]
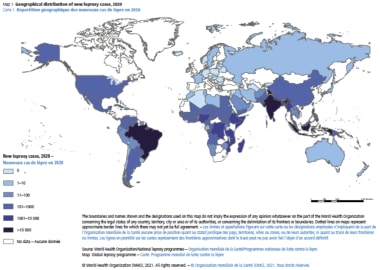
In April 2021, the WHO launched its 2021-2030 strategy, “Towards zero leprosy.” The goal of this strategy is the “elimination of leprosy.” Elimination is now defined as the interruption of transmission in a geographic zone. These goals are centered around four pillars: implement integrated, country-owned zero leprosy road maps in all endemic countries; scale up leprosy prevention alongside integrated active case detection; manage leprosy and its complications and prevent new disability; and combat stigma and ensure human rights are respected. [1] In 2019, the WHO reported 202,256 new leprosy cases, corresponding to a prevalence of 1.4 per million. [1] The case prevalence of leprosy (registered number of people on treatment) at the end of 2020 was 129,192, with a case rate of 16.6 per million. This reduction in cases is likely due to underreporting as a result of the pandemic. [4]
Although multidrug regimens had been used globally to cure nearly 18 million patients with leprosy since 1981, [1] the number of new leprosy cases remained relatively unchanged from 1980 to 2000, ranging from 500,000-700,000 worldwide per year. [5] Between 2001 and 2006, the global incidence of leprosy declined suddenly, largely owing to new case reductions in India.
The goal of the WHO by the end of 2015 was to reduce the rate of new cases with grade-2 disabilities(G2D) worldwide by at least 35%. This was done by enforcing activities to decrease the delay in diagnosing the disease and actuate treatment with multidrug therapy. This also reduced transmission of the disease in the community. [5] Now, the goal for 2030 is to reduce the rate of new cases with G2D by 90%. [1]
Access and delivery of antibiotics continue to be a problem in most endemic nations. With the precise transmission mechanism of leprosy still unknown and the lack of an effective vaccine, leprosy will probably continue to pose an ongoing public health problem in the coming decades.
Pathophysiology
Leprosy can manifest in different forms, depending on the host response to the organism.
Individuals who have a vigorous cellular immune response to M leprae have the tuberculoid form of the disease that usually involves the skin and peripheral nerves. The reaction types include type 1 reaction (T1R). The number of skin lesions is limited, and they tend to be dry and hypoesthetic. Nerve involvement is usually asymmetric. This form of the disease is also referred to as paucibacillary leprosy because of the low number of bacteria in the skin lesions (ie, < 5 skin lesions, with the absence of organisms on smear). Results of skin tests with antigen from killed organisms are positive in these individuals.
Individuals with minimal cellular immune response have the lepromatous form of the disease, which is characterized by extensive skin involvement. Skin lesions are often described as infiltrated nodules and plaques, and nerve involvement tends to be symmetric in distribution. The organism grows best at 27-30°C; therefore, skin lesions tend to develop in the cooler areas of the body, with sparing of the groin, axilla, and scalp. This form of the disease is also referred to as multibacillary leprosy because of the large number of bacteria found in the lesions (ie, >6 lesions, with possible visualization of bacilli on smear). Results of skin tests with antigen from killed organisms are nonreactive.
Patients may also present with features of both categories (indeterminate or borderline leprosy); however, over time, they usually evolve to 1 or the other. Interestingly, most individuals who are exposed to leprosy never develop the disease, likely because over 95% of people have natural immunity to it. [6]
Classification of leprosy
Leprosy has 2 classification schemas: the 5-category Ridley-Jopling system and the simpler and more commonly used WHO standard. [7]
Ridley-Jopling: Depending on the host response to the organism, leprosy can manifest clinically along a spectrum bounded by the tuberculoid and lepromatous forms of the disease. Most patients fall into the intermediate classifications, which include borderline tuberculoid (BT) leprosy, midborderline (BB) leprosy, and borderline lepromatous (BL) leprosy. The classification of the disease typically changes as it evolves during its progression or management. The Ridley-Jopling system is used globally and forms the basis of clinical studies of leprosy. It also may be more useful in guiding treatment regimens and assessing risk for acute complications. Physical findings in each subtype are presented in the Clinical section.
According to the WHO, in an endemic area, an individual is considered to have leprosy if they show either of the 2 following signs [7] :
-
A skin lesion consistent with leprosy and definite sensory loss, with or without thickened nerves
-
Positive skin smears
Epidemiology
Frequency
United States
In 2015, according to the Centers for Disease Control and Prevention (CDC), 178 new cases of leprosy were reported in the United States. [8]
Eighty-five percent of leprosy cases in the United States are found in immigrants, [9] although endemic foci exist in parts of Louisiana, Florida, and Texas along the Gulf of Mexico; in Mexican and Asian California populations; and in Spanish Americans in New York City.
Some cases among native US citizens can be accounted for by exposure to leprosy overseas. Some cases can be attributed to a contact with a known case of leprosy or exposure to infected armadillos, especially in the southern United States, where wild armadillos and many patients with leprosy in the United States are infected with the same strain of M leprae. [8] Leprosy may be a zoonosis in the southern United States because armadillos are a large reservoir for this disease.
Nonetheless, history of exposure cannot be verified in many patients. [10]
International
According to WHO figures based on reports from 159 countries, 208,619 new leprosy cases were reported globally in 2018. The worldwide prevalence reported at the end of 2018 was 184,212 cases (rate, 0.2/10,000). In 2018, Brazil, India, and Indonesia accounted for 79.6% of all new leprosy cases. [11] In addition, 23 priority countries accounted for 96% of cases worldwide in 2018.
{file 306392}
Mortality/Morbidity
Leprosy is rarely fatal, and the primary consequences of infection are nerve impairment and debilitating sequelae. According to one study, 33-56% of newly diagnosed patients already displayed signs of impaired nerve function. [12] According to estimates, 3 million people who have completed multidrug therapy for leprosy have sustained disability due to nerve damage. Although both lepromatous leprosy and tuberculoid leprosy involve the skin and peripheral nerves, tuberculoid leprosy has more severe manifestations. Nerve involvement results in sensory and motor function loss, which may lead to frequent trauma and amputation. The ulnar nerve most commonly is involved.
Damage in the following nerves is associated with characteristic impairments in leprosy:
-
Ulnar and median - Clawed hand
-
Posterior tibial - Plantar insensitivity and clawed toes
-
Common peroneal - Foot drop
-
Radial cutaneous, facial, and greater auricular nerves (may also be involved, as seen in the image below)
Infiltration by bacteria may lead to destruction of nasal cartilage (lepromatous leprosy), ocular involvement, and diffuse thickening of the skin. Advanced cases of leprosy involve the loss of eyebrows and lashes, but these deformities are less common today.
Worldwide, leprosy is considered a common cause of crippling of the hand, which is caused by ulnar nerve involvement. [13] Peroneal nerve involvement can lead to foot drop, posterior tibial nerve involvement, and clawed toes.
Race
Leprosy was once endemic worldwide, and no racial predilection is known. In the late 1800s, the incidence of leprosy in northern Europe and North America dropped dramatically, and the disease now is reported primarily in tropical areas.
Sex
Leprosy generally is more common in males than in females, with a male-to-female ratio of 2:1. In some areas in Africa, the prevalence of leprosy among females is equal to or greater than that in males. [14]
Age
Leprosy can occur at any age, but in developing countries, the age-specific incidence of leprosy peaks in children younger than 10 years, who account for 20% of leprosy cases. Leprosy is rare in infants; however, they are at a relatively high risk of acquiring leprosy from the mother, especially in cases of lepromatous leprosy or midborderline leprosy.
HIV coinfection
Unlike with tuberculosis, preliminary data suggest that coinfection with HIV does not seem to have an effect on leprosy. Furthermore, HIV coinfection does not seem to affect the ratio of lepromatous to tuberculoid leprosy. [12]
-
Hands with Z-thumbs, clawing, contractures, and shortening of fingers due to repetitive injury and healing. Ho Chi Minh City, Vietnam. Courtesy of D. Scott Smith, MD.
-
Patient with facial nerve palsy and contractures of the hand. Daloa, Ivory Coast. Courtesy of D. Scott Smith, MD.
-
Chronic insensate patch due to leprosy infection. Ho Chi Minh City, Vietnam. Courtesy of D. Scott Smith, MD.
-
Characteristic clawed hand deformity caused by ulnar involvement in leprosy. Daloa, Ivory Coast. Courtesy of D. Scott Smith, MD.
-
Chronic nonhealing ulcer at the metatarsal head resulting from loss of sensation in the feet. Karigiri, Tamil Nadu, India. Courtesy of Tara Ramachandra.
-
Multiple flat hypopigmented lesions on shoulder and neck, suggestive of multibacillary leprosy. Note ulceration of hypothenar area of hand, indicative of sensory loss with curled 5th digit, from ulnar neuropathy. Redwood City, California, United States. Courtesy of D. Scott Smith, MD.
-
Man with advanced deformities caused by unmanaged leprosy. Keratitis, loss of eyebrow, thickened skin, and typical hand impairments. Ho Chi Minh City, Vietnam. Courtesy of D. Scott Smith, MD.
-
Histopathology of leprosy: Large numbers of acid-fast bacilli (in clusters) in histiocytes and within nerves. Fite-Faraco stain 500 X. Courtesy of Tara Ramachandra, MD, and D. Scott Smith, MD.
-
Patient with multibacillary leprosy showing subsequent erythema nodosum leprosum reaction. Santa Clara, California. Courtesy of D. Scott Smith, MD.
-
Patient with erythema nodosum leprosum type 2 reaction several weeks after initiation of drug therapy. This photograph was taken after tendon release. Redwood City, California. Courtesy of D. Scott Smith, MD.
-
Increased pigmentation on the face due to clofazimine therapy. Courtesy of D. Scott Smith, MD.
-
2018 leprosy treatment guidelines. Courtesy of the WHO.
-
Map of countries reporting rifampicin resistance in leprosy between 2009 and 2015. Courtesy of the WHO.
-
2018 WHO guidelines for treatment of drug-resistant leprosy. Courtesy of the WHO.
-
2018 guidelines for single-dose rifampicin. Courtesy of the WHO.
-
WHO map showing new cases of new leprosy cases, 2020. Courtesy of the WHO.