Background
Primary gastrointestinal (GI) sarcomas in general are a very rare entity, accounting for 1%-2% of GI malignancies. Of this uncommon group of highly malignant neoplasms, the leiomyosarcoma is the most common histiotype. [1] Intestinal leiomyosarcomas are mesenchymal tumors of smooth muscle origin. They occur mainly in the fifth and sixth decades of life, and abdominal pain and GI bleeding have been reported to be the most common clinical signs at presentation.
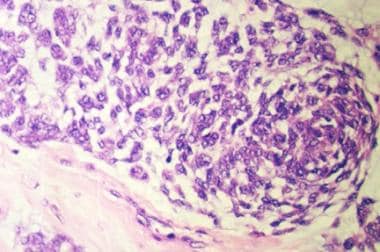
In the past, GI stromal tumors (GISTs) were misdiagnosed as leiomyosarcomas. GISTs, however, have been shown to lack characteristics of smooth muscle tumors on histologic examination. [2] They are often CD34 immunoreactive and express tyrosine kinase c-kit (CD117) receptor activity, in contrast to leiomyosarcomas. [3] Mutations in the c-kit receptor are linked to the neoplastic development. (See image below.)
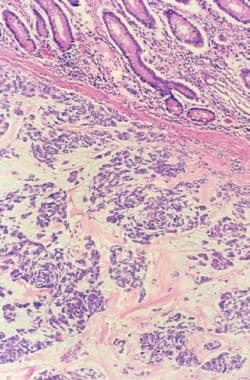 Colonic mucosa with gastrointestinal stromal tumor (GIST) involving the adjacent submucosa (hematoxylin and eosin [H&E] stain, medium power).
Colonic mucosa with gastrointestinal stromal tumor (GIST) involving the adjacent submucosa (hematoxylin and eosin [H&E] stain, medium power).
Approximately 1%-2% of solid tumors are soft-tissue sarcomas, and leiomyosarcomas comprise roughly 2%-9% of these sarcomas. Of the leiomyosarcomas, 20% are found in the GI tract, with sites of occurrence evenly divided between the stomach and the small intestine.
Pathophysiology
The causes of leiomyosarcoma are unknown.
These lesions apparently arise between the muscularis propria and muscularis mucosa layers of the bowel wall, though the exact histological source is in question. The tumors generally are made up of spindle-shaped cells and have a high cellularity. (See the following image.) With high-grade tumors, necrosis often is present.
When considering all the primary malignancies of the small bowel, adenocarcinomas tend to occur more proximally, whereas carcinoids, lymphomas, and leiomyosarcomas occur more distally. Depending on the study reviewed, the primary sites of occurrence of leiomyosarcomas are divided equally between the stomach and the small intestine. As many as 50% of the leiomyosarcomas occurring in the small intestine are found in the ileum. Relatively few leiomyosarcomas have been found in the esophagus, colon, or rectum.
The natural history of this tumor involves local growth initially, with much of its growth being extraluminal; thus, bowel obstruction occurs late. Multiple primary sites are unusual. Often, as the size of the leiomyosarcoma increases, necrosis and bleeding follow. This leads to the most common presenting feature in symptomatic patients, bleeding, which often is massive.
Metastasis is primarily hematologic. Lymph node metastasis is rare, occurring in 0%-15% of cases, depending on the series. Leiomyosarcomas spread to the liver and peritoneum first. Spread to the lungs occurs less frequently than spread to the liver and the peritoneum. This is in contrast to other soft tissue sarcomas in which the lung is the most common site of metastasis. About 20%-40% of patients have metastasis at the initial laparotomy.
The two factors that are recurrent themes in any discussion of leiomyosarcomas are size and grade. These features largely determine the survivability of a patient with this disease. The impact of size is debatable. Logically, resection, which is the only hope for a cure, appears to be more difficult with larger tumors.
If a tumor is large, metastasis is more likely to have occurred. Because these tumors are extraluminal, they can grow quite large before they become symptomatic. They can range from 4-5 cm in diameter to as large as 19 cm.
The grade of malignancy is judged microscopically and is accepted universally as a prognostic indicator. Generally, high-grade change is considered greater than 5 mitotic figures per 10 high-powered fields.
Recurrence occurs in the peritoneum and/or the retroperitoneum. As many as 55% of patients with recurrence have metastatic lesions to the liver at the time that their recurrence is discovered. If a low-grade tumor recurs, it often does so with a new, more aggressive grade of histology.
Epidemiology
United States statistics
Intestinal leiomyosarcomas are fairly rare, with a frequency of around 1.4 cases per 100,000 patients.
The Martin series, which comprised 11,438 cases of gastrointestinal (GI) tract tumors from 1944 to 1982, included only 280 patients with primary small intestine tumors. [4] If ampullary lesions are excluded from this count, 217 cases of primary small intestine tumors, or 2.4%, were included in the series.
In 1994, DiSario reviewed the cases entered from 1966 to 1990 in the Utah Cancer Registry; only 328 cases of small intestine cancer were recorded. [5] Of these cases, 41% were carcinoid, 24% were adenocarcinomas, and 11% were sarcomas (1% was not clearly identified).
Carcinoid and adenocarcinomas are far more common, even when ampullary lesions are excluded.
A study by Jun Zhan and colleagues determined that malignant tumors were the most common small intestinal neoplasia. [6] Of the 125 patients with malignant tumors, 11% had leiomyosarcoma, 11% had adenocarcinoma, and 9% had small intestinal lymphoma. Patients with primary small intestinal disease most commonly presented with periumbilical pain.
International data
Information on international frequency is unavailable.
Sex- and age-related demographics
Depending on the study, the male-to-female ratio ranges from 1:1 to 2:1. No study was found in which sex was a prognostic indicator.
Leiomyosarcomas primarily are a disease of middle-aged persons, with the average age on presentation falling between the fifth and seventh decades of life.
Prognosis
With curative resection, the 5-year survival rate for patients with leiomyosarcoma of the small intestine is 40%-50%, according to Hill's review. [7]
In cases in which the grade of the tumor was documented, the median survival for patients with high-grade tumors was 25 months in one study, whereas the median survival for patients with low-grade tumors was approximately 98 months. [8]
A benign initial report on a resected tumor does not remove the patient from serious consequences because these tumors sometimes recur as malignancies—about 6% in one study. [9]
In a report on the characteristics of duodenal gastrointestinal stromal tumors (GISTs), Miki et al compared the clinicopathologic findings in and recurrence-free survival of 7 patients with these lesions with the same data for 34 patients with GISTs of the stomach or elsewhere and determined that the rates for symptomatic lesions were 86% in the duodenum, 32% in the stomach, and 56% elsewhere, with melena and anemia being the most common symptoms associated with duodenal GISTs. [10] The rates of 2-year recurrence-free survival among patients were 51.4% for duodenal GISTs, 78.4% for stomach GISTs, and 100% for other GISTs. Using multivariate Cox analysis, the authors concluded that in terms of GIST recurrence, significant prognostic factors included symptoms, mitotic index, and tumor location. [10, 11, 12]
Morbiditymortality
The prognosis ranges from universally fatal to poor. Size and grade are determinants of prognosis, depending on the case series. Histology consisting of high-grade malignancy and a large tumor size portends a poor prognosis.
With curative resection, the 5-year survival rate of patients with a gastric leiomyosarcoma is 68%-90%, whereas small intestine tumors are associated with a survival rate of 40%-50%. Distant metastasis decreases the survival rate to around 30%.
Evans presented a 10-year series in which he followed the outcomes of 56 patients and found that approximately 70% of them had high-grade tumors. [8] Patients with high-grade tumors had a median survival of 25 months. Patients with a low-grade tumor survived much longer, with a median survival of 98 months. In fact, 2 patients (15%) survived the study. Overall, the 5-year survival rate ranges from 18% to 50%. This range largely is a factor of patient selection.
In a study published in 1998, all leiomyosarcomas occurring over the span of 45 years at Charity Hospital in New Orleans were reviewed. [7] The authors found that leiomyosarcomas of the small intestine and uterus had a somewhat better prognosis than those occurring in the retroperitoneum.
-
Colonic mucosa with gastrointestinal stromal tumor (GIST) involving the adjacent submucosa (hematoxylin and eosin [H&E] stain, medium power).
-
Clusters of tumor cells separated by a hyaline and mucin-rich stroma (hematoxylin and eosin [H&E] stain, medium power).
-
Oval- to spindle-shaped cells forming a fascicle (hematoxylin and eosin [H&E] stain, high power).
-
CD-34 stain showing a tumor (medium power). CD-34 is a myeloid progenitor cell antigen.
-
High-power magnification with CD-34 antigen immunohistochemical stain showing membrane positivity of the tumor cells.