Practice Essentials
Human papillomavirus (HPV) produces epithelial tumors of the skin and mucous membranes. The current classification system for HPV, which is based on similarities in genomic sequences, generally correlates with the 3 clinical categories applied to HPV infection:
-
Anogenital or mucosal (further subclassified as latent [asymptomatic], subclinical, or clinical)
-
Nongenital cutaneous
-
Epidermodysplasia verruciformis (see the images below)
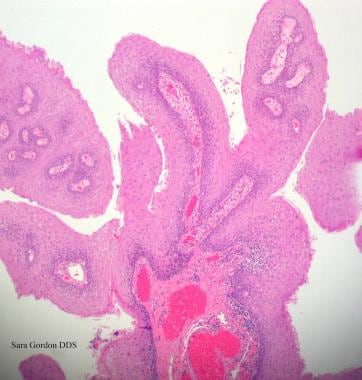
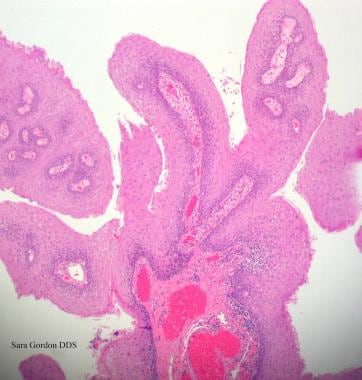 Human papillomavirus (HPV). Verrucae and papillomas appear as frondlike epithelial proliferations. Verrucae tend to be more keratinized with sharper projections than papillomas.
Human papillomavirus (HPV). Verrucae and papillomas appear as frondlike epithelial proliferations. Verrucae tend to be more keratinized with sharper projections than papillomas.
See Pediatric Vaccinations: Do You Know the Recommended Schedules?, a Critical Images slideshow, to help stay current with the latest routine and catch-up immunization schedules for 16 vaccine-preventable diseases.
Signs and symptoms
The clinical history and presentation of HPV infection vary according to the anatomic area involved. The predilection of certain viral genotypes for infecting certain epidermal sites largely determines areas of involvement. Conditions with which HPV is associated include the following:
-
Anogenital warts (condylomata acuminata): These are usually found near moist surfaces (eg, perianal area, vaginal introitus, vagina, labia, and vulva) but may also be found on dry surfaces (eg, penile shaft); they may be smooth and papular or keratotic; they generally are not painful but can be associated with pruritus or bleeding
-
Cervical disease (eg, low-grade squamous intraepithelial lesion [LGSIL] or high-grade squamous intraepithelial lesion [HGSIL])
-
Anal cancer: About 50% of men who are homosexual and have anal squamous cell carcinoma (SCC) have a history of anorectal warts; however, only 20% of women with SCC and men who are not homosexual have this history
-
Nonanogenital mucosal disease (eg, oral warts, respiratory papillomas, and focal epithelial hyperplasia [Heck disease])
-
Nongenital cutaneous disease (eg, common cutaneous warts [verruca vulgaris], flat warts [verruca plana] and Bowenoid papulosis)
-
Epidermodysplasia verruciformis
Physical findings vary, depending on the tissues involved, and may include the following:
-
Typical condylomata are discrete, papillary, cauliflower-like lesions that involve multiple sites on moist surfaces
-
Keratotic warts are often seen on dry surfaces such as the labia majora
-
Discrete papules 1-3 mm in size can present on the shaft of the penis
-
Cervical intraepithelial lesions may be found upon examination of the cervix
-
Subclinical infection may be present, with tiny, slightly raised areas felt or visualized on the vagina or cervix
See Clinical Presentation for more detail.
Diagnosis
The diagnosis of most cutaneous and external genital warts can be made through clinical examination or with application of acetic acid and biopsy. In genital intraepithelial neoplasia, it is essential to determine the extent of disease through careful inspection and colposcopy.
Laboratory studies that may be considered include the following:
-
Cervical cytologic testing with the Papanicolaou (Pap) test to screen for cervical neoplasia (guidelines for cervical cancer screening now include a delay in the initiation of screening and longer intervals between subsequent screens [1] )
-
HPV DNA testing (eg, with Hybrid Capture II or polymerase chain reaction [PCR] assay) for detection of HPV and posttreatment follow-up of cervical intraepithelial neoplasia
-
The acetic acid test: This test can be used in conjunction with colposcopy to examine cervical lesions; however, it is reserved for suspicious lesions and should not be used for routine screening
In some cases, tissue biopsy can be used to confirm HPV infection. A biopsy is recommended for the following scenarios:
-
Women with a history of vulvar dysplasia
-
Postmenopausal women
-
Women in whom medical therapy fails
-
Clinical doubt about the diagnosis
Histologic findings that can help elucidate the diagnosis include the following:
-
Common cutaneous warts: Marked hyperkeratosis, acanthosis, parakeratosis, and papillomatosis; warts can be distinguished from other papillomas by the presence of koilocytes, vertical columns of parakeratosis, and foci of clumped keratohyaline granules
-
Condyloma acuminatum: Disruption of the epidermis with hyperkeratosis, coarse keratohyaline granules, and koilocytes in a prominent granular layer; the epidermis or mucosa of flat condylomata demonstrates acanthosis
-
Bowenoid papulosis: Psoriasiform hyperplasia and hyperkeratosis of the epidermis, with increased mitotic figures at all epidermal levels and keratinocytes displaying enlarged pleomorphic and hyperchromic nuclei
See Workup for more detail.
Management
All medicines used to treat HPV disease are applied topically; they should not be applied to mucosal surfaces and should not be used to treat dysplastic lesions, squamous cell carcinoma, verrucous carcinoma, or Bowenoid papulosis. The following 2 broad categories of medications are effective:
-
Immune response modifiers (eg, imiquimod and interferon alfa): These are primarily used in treatment of external anogenital warts or condylomata acuminata
-
Cytotoxic agents: These include both antiproliferative drugs (eg, podofilox, podophyllin, and 5-fluorouracil [5-FU]) and chemodestructive or keratolytic agents (eg, salicylic acid, trichloroacetic acid [TCA], and bichloracetic acid [BCA]); the latter are the only agents recommended for treatment of nongenital cutaneous warts
Sinecatechins ointment is another option.
Surgical interventions are commonly considered when a large number of warts are present, a large area is affected, or the patient has refractory disease. Overall, physical destruction or excision has been more effective in eradicating genital warts than medical therapy. Primary surgical therapy can often be accomplished in the office and includes the following options:
-
Cryosurgery
-
Electrosurgery (electrodesiccation or a loop electrosurgical excision procedure [LEEP])
-
Simple surgical excision with a scalpel, scissors, or curette
Alternative surgical procedures include the following:
-
Carbon dioxide laser ablation
-
Cavitron Ultrasonic Surgical Aspiration (CUSA)
-
Mohs surgery
Vaccines are available for prevention of HPV infection, and recommended vaccination schedules have been outlined.
See Treatment and Medication for more detail.
Background
HPV produces epithelial tumors of the skin and mucous membranes. More than 100 HPV types are known, and the genomes of more than 80 have been completely sequenced. People with multiple sexual partners and those who already have persistent HPV infection are at increased risk for acquiring additional HPV strains. [2, 3, 4, 5] The current classification system, which is based on similarities in genomic sequences, generally correlates with the 3 clinical categories applied to HPV:
-
Anogenital or mucosal
-
Nongenital cutaneous
The mucosal HPV infections are classified further as latent (asymptomatic), subclinical, or clinical. Clinical lesions are grossly apparent, whereas latent infections are detected only with tests for viral DNA. Subclinical lesions are identified by application of 3-5% acetic acid and inspection under magnification. Most HPV infections are latent; clinically apparent infections usually result in warts rather than malignancies.
Infections due to HPV are common and lead to a wide variety of clinical manifestations that involve the epidermal surfaces. Condylomata acuminata (genital warts) are generally recognized as benign proliferations of the anogenital skin and mucosa resulting from HPV infection. Genital warts are transmitted by sexual contact. Approximately two thirds of individuals who have sexual contact with an infected partner develop genital warts. The exact incubation time is unknown but estimated to be 3 weeks to 8 months. [6, 7]
Despite the generally benign nature of these proliferations, certain types of HPV can place patients at a high risk for anogenital cancer. [8, 9, 10] Some have also been implicated in laryngeal and oral cancer and some lung cancers.
HPV types 6 and 11 are typically labeled as low risk because infection with these types has low oncogenic potential and usually results in the formation of condylomata and low-grade precancerous lesions. HPV types 16 and 18 have emerged as the high-risk types of HPV because they are responsible for most high-grade intraepithelial lesions that may progress to carcinomas, particularly those in the anogenital or mucosal category.
HPV infection alone does not cause malignant transformation of infected tissue. Cofactors, such as tobacco use, ultraviolet radiation, pregnancy, folate deficiency, and immune suppression, have been implicated in this process.
Physicians’ understanding of the natural history of HPV disease has significantly improved over the last 20 years, but key issues remain unanswered. Topics requiring further research include HPV age-specific outcomes, the likelihood of progression or regression of disease, and factors important in the acquisition of immunity following infection. [11]
Pathophysiology
Papillomaviruses are nonenveloped viruses of icosahedral symmetry with 72 capsomeres that surround a genome containing double-stranded circular DNA with approximately 8000 base pairs. Their genome is divided into the following 3 major functional regions:
-
The early (E) region codes for 6 nonstructural genes, several of which are associated with cellular transformation.
-
The late (L) region codes for 2 structural proteins, L1 and L2, that form the capsid
-
The long control region is a noncoding region that regulates replication and gene function
Papillomaviruses are highly species-specific and do not infect other species, even under laboratory conditions. Humans are the only known reservoir for HPV. Papillomaviruses have never been grown in vitro but have been characterized by molecular methods. These viruses are classified by the molecular similarity of their genetic material and are assigned a genotype number.
Although some overlap exists, most papillomaviruses have distinct anatomic predilections, infecting only certain epidermal sites, such as skin or genital mucosa. The virus has the potential to integrate into host DNA, frequently with the loss of the early regulatory function.
HPV infects the basal keratinocyte of the epidermis, presumably through disruptions of the skin or mucosal surface. At this location, the virus remains latent in the cell as a circular episome in low copy numbers. Autoinoculation of virus into opposed lesions is common. Spread of HPV infection is usually through skin-associated virus and not blood-borne infection. Cell-mediated immunity (CMI) probably plays a significant role in wart regression; patients with CMI deficiency are particularly susceptible to HPV infection and are notoriously difficult to treat. [12]
Papillomaviruses are thought to have 2 modes of replication:
-
Stable replication of the episomal genome in basal cells
-
Runaway, or vegetative, replication in more differentiated cells to generate progeny virus
As the epidermal cells differentiate and migrate to the surface, the virus is triggered to undergo replication and maturation, and at the keratitic layer, the virus is present in high copy numbers and is shed in the exfoliation cells. The process of virus replication alters the character of the epidermis, resulting in cutaneous or mucosal excrescences known as warts.
Note the figures below detailing the mechanisms of action for HPV.
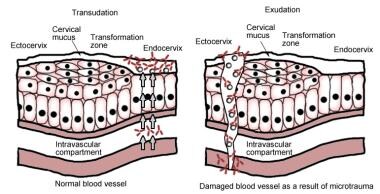 The left panel is transudation of serum antibodies to the site of human papillomavirus infection, and the right panel is exudation of serum antibodies to the site of human papillomavirus infection.
The left panel is transudation of serum antibodies to the site of human papillomavirus infection, and the right panel is exudation of serum antibodies to the site of human papillomavirus infection.
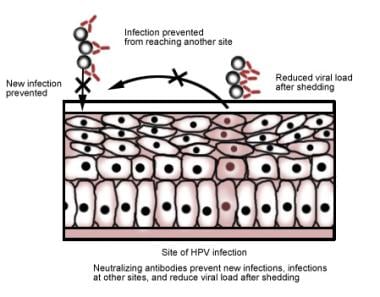 The figure shows proposed mechanisms used by the human papillomavirus vaccine to neutralize antibodies and protect against infection.
The figure shows proposed mechanisms used by the human papillomavirus vaccine to neutralize antibodies and protect against infection.
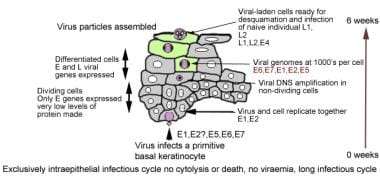 Figure showing how human papillomavirus penetrates the basal layer and eventually is released at the surface.
Figure showing how human papillomavirus penetrates the basal layer and eventually is released at the surface.
Although all cells of a lesion contain the viral genome, the expression of viral genes is tightly linked to the state of cellular differentiation. Most viral genes are not activated until the infected keratinocyte leaves the basal layer. Production of virus particles can occur only in highly differentiated keratinocytes; therefore, virus production occurs only at the epithelial surface where the cells are ultimately sloughed into the environment.
HPV infections have not been shown to be cytolytic; rather, viral particles are released as a result of degeneration of desquamating cells. The HPV virus can survive for many months and at low temperatures without a host; therefore, an individual with plantar warts can spread the virus by walking barefoot.
Viral multiplication is confined to the nucleus. Consequently, infected cells exhibit a high degree of nuclear atypia. Koilocytosis (from Greek koilos “empty”) describes a combination of perinuclear clearing (halo) with a pyknotic or shrunken (raisinoid) nucleus and is a characteristic feature of productive papillomavirus infection.
Numerous viral genotypes have the potential to transform cells and are associated with epidermal malignancies. In benign or low-risk HPV lesions, such as those typically associated with HPV types 6 and 11, the HPV genome exists as a circular episomal DNA separate from the host cell nucleus. In malignant lesions, the genomes of high-risk HPV types 16 and 18 are typically integrated into the host cell DNA. Integration of the viral genome into the host cell genome is considered a hallmark of malignant transformation.
HPV proteins E6 and E7 of high-risk serotypes have been shown to inactivate the host’s tumor suppressor proteins p53 and Rb, thereby resulting in unregulated host cell proliferation and malignant transformation.
Etiology
The definitive cause of anogenital warts is HPV infection. [8, 9, 10, 13] The HPV capsid lacks an envelope, which makes the organism very stable and resistant to various treatments. No serologic typing is available, because of the lack of consistent in vitro culture methods. Typing of HPV is based on genotype, which generally is determined by molecular hybridization using molecularly cloned HPV DNA of known type as the standard. Two HPV are of different types when their DNA hybridize (bind) less than 50% as efficiently to each other as to themselves.
The nearly 40 types of HPV that have been found in genital warts [14] are highly host-specific. These viruses do not infect laboratory animals and are not susceptible to acyclovir. In addition, HPV types demonstrate a high degree of site specificity, with some types only found on certain parts of the skin or mucous membranes. As a rule, HPV types causing common warts of the skin do not infect moist epithelium, and vice versa.
Multiple clinical associations with unique genotypes of HPV have been documented. Some of these associations are listed in the Table below.
Table 1. Diseases Associated With Specific HPV Types (Open Table in a new window)
Nongenital Cutaneous Disease |
HPV Type |
Common warts (verrucae vulgaris) |
1, 2, 4, 26, 27, 29, 41, 57, 65, 75-78 |
Plantar warts (myrmecias) |
1, 2, 4, 60, 63 |
Flat warts (verrucae planae) |
3, 10, 27, 28, 38, 41, 49 |
Butcher’s warts (common warts of people who handle meat, poultry, and fish) |
1-4, 7, 10, 28 |
Mosaic warts |
2, 27, 57 |
Ungual squamous cell carcinoma |
16 |
Epidermodysplasia verruciformis (benign) |
2, 3, 10, 12, 15, 19, 36, 46, 47, 50 |
Epidermodysplasia verruciformis (malignant or benign) |
5, 8-10, 14, 17, 20-25, 37, 38 |
Nonwarty skin lesions |
37, 38 |
Nongenital Mucosal Disease |
HPV Type |
6, 11 |
|
6, 11, 16, 18 |
|
Laryngeal papilloma (recurrent respiratory papillomatosis) [15] |
2, 6, 11, 16, 30, 40, 57 |
6, 11 |
|
Maxillary sinus papilloma |
57 |
Squamous cell carcinoma of the sinuses |
16, 18 |
Conjunctival papillomas |
6, 11 |
Conjunctival carcinoma |
16 |
Oral focal epithelial hyperplasia (Heck disease) |
13, 32 |
16, 18 |
|
16, 18 |
|
16, 18 |
|
Anogenital Disease |
HPV Type |
1-6, 10, 11, 16, 18, 30, 31, 33, 35, 39-45, 51-59, 70, 83 |
|
16, 18, 34, 39, 40, 42, 45 |
|
16, 18, 31, 34 |
|
Giant condylomata (Buschke-Löwenstein tumors) |
6, 11, 57, 72, 73 |
Unspecified intraepithelial neoplasia |
30, 34, 39, 40, 53, 57, 59, 61, 62, 64, 66-69 |
Low-grade squamous intraepithelial lesions (LGSIL) |
6, 11, 16, 18, 26, 27, 30, 31, 33-35, 40, 42-45, 51-58, 61, 62, 67-69, 71-74, 79, 81-84 |
High-grade squamous intraepithelial lesions (HGSIL) |
6, 11, 16, 18, 31, 33, 35, 39, 42, 44, 45, 51, 52, 56, 58, 59, 61, 64, 66, 68, 82 |
6, 11, 16, 18 |
|
Carcinoma of vagina |
16 |
16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68, 70, 73, 82 |
|
Carcinoma of anus |
16, 31, 32, 33 |
Carcinoma in situ of penis (erythroplasia of Queyrat) |
16 |
16, 18 |
Risk factors
HPV infection alone does not cause malignant transformation of infected tissue. Cofactors, such as tobacco use, ultraviolet radiation, pregnancy, folate deficiency, and immune suppression, have been implicated in this process, particularly in the anogenital-mucosal category. Patients receiving immunosuppressive drugs and patients with defects in cell-mediated immunity, including those infected with HIV, are especially susceptible to HPV infections.
Sexual activity
A direct correlation exists between anogenital HPV infection and measures of sexual activity, such as the age of first intercourse and the lifetime number of sexual partners.
Women with a history of high-grade squamous intraepithelial lesions (HGSIL) of the cervix or invasive squamous cell carcinoma (SCC) of the cervix are at increased risk for subsequent development of invasive cancer in other tissues of the anogenital-mucosal category, particularly vaginal and anal carcinoma (relative risks, 5.6 and 4, respectively).
Anal cancer has been strongly associated with male homosexuality and with specific male practices, such as engaging in receptive anal intercourse; relative risk is 33. However, the overall disease prevalence is higher in women than in men, with a female-to-male ratio of 1.5:1.
Tobacco smoking
Women who smoke tobacco have an increased risk of developing cervical neoplasia. Measurable amounts of a potent carcinogen, as well as several compounds from cigarette smoke, have been identified in the cervical mucus of females who smoke. These agents are likely to play a role in the increased prevalence of HPV malignant transformation observed in patients who smoke tobacco.
Oral contraceptive use
Women who take oral contraceptives for longer than 5 years have an increased relative risk of developing cervical carcinoma. This risk declines after oral contraceptive use is stopped, and no risk is demonstrated in women who took these agents for less than 5 years.
Chewing Indian betel quid
A high incidence of oral cancer associated with HPV infection has been demonstrated in India among patients who chew betel quid. This stimulant is made from the leaves of the betel plant and is used in a manner similar to chewing tobacco.
Ultraviolet and x-ray irradiation
EV is particularly susceptible to ultraviolet (UV) and x-ray irradiation; therefore, patients with EV should avoid activities that unnecessarily expose them to these forms of radiation.
Epidemiology
United States statistics
The United States has no reporting system for HPV infections. Infections and the development of warts appear to be common throughout life. In general, genital HPV infection is considered to have become dramatically more frequent over the past several decades.
In the United States, young adults aged 15-24 years account for approximately one half of new HPV infections each year. [18] The frequency of genital infections is associated with the number of sexual partners and the age of sexual debut. Patients receiving immunosuppressive drugs and patients with defects in cell-mediated immunity, including those infected with the human immunodeficiency virus (HIV), are especially susceptible to developing HPV infections.
Using data and self-collected cervicovaginal specimens from 4150 females in 4 consecutive National Health and Nutrition Examination Surveys (2003-2006), Hariri et al found HPV present in 42.5% of US females aged 14-59 years. The highest rate of infection is among young females aged 20-24 years. [19]
The population-based incidence of genital warts was estimated at 106 cases per 100,000 population in Rochester, Minnesota (for 1975-1978) [20] and at 160 cases per 100,000 population in Manitoba, Canada (for 1992), [21] with the highest incidence rate in residents aged 20-24 years.
Figures from 5 Blue Cross/Blue Shield Health Plans projected an incidence of 105 cases per 100,000 population (for 2004). [22] They estimated 340,000 cases nationwide in 2004, with an economic burden of more than $220 million. [22]
These figures differed from those indicated by data collected from STD clinics and private practitioners’ offices. Using data from these sources, the US Centers for Disease Control and Prevention (CDC) suggested much higher figures: an estimated incidence of more than 6 million new patients a year in the United States (in 2008) and an estimated prevalence of more than 20 million. [23, 24, 25, 26, 27] By way of comparison, the CDC estimated that 1.6 million people have genital herpes and 1.6 million have chlamydia or gonorrhea.
According to the “National Disease and Therapeutic Index: United States, 1966–2010, the Initial visits to physicians’ offices for STD,” the increasing trend of HPV infection, after peaking at 351,000 visits in 1987, went down in the following 10 years. Unfortunately, the increasing trend resumed again and reached the highest level ever in 2006 (422,000 visits) before dropping down to 357,000 in 2010.
Studies diagnosing HPV infection through by visual inspection of genital condylomata report the lowest prevalences. The highest prevalences are reported by studies typing HPV from exfoliated genital tract cells. As many as 75% of individuals who have sexual contact with an HPV-infected partner will develop external genital warts. [28]
Condylomata acuminata are clinically apparent in 1% of the sexually active population. Molecular studies indicate that 10-20% of men and women aged 15-49 years have been exposed to HPV. The prevalence of HPV is higher in certain populations. A prevalence of 4-13% has been reported by sexually transmitted disease (STD) clinics.
Several investigators report an increased prevalence of anogenital HPV infections during pregnancy. The prevalence of condyloma increases from the first to third trimester and then decreases significantly post partum. The risk of condyloma acuminatum in pregnancy is 2-fold. Vulvar condylomata can rarely become large enough to obstruct labor. Cesarean delivery decreases, but does not completely prevent, HPV transmission with development of laryngeal papillomas in the infant. [29, 30, 31, 32]
HPV infection causes virtually all cases of cervical cancer. [33, 34] In cervical neoplasias, the HPV genome can be detected in more than 95% of tumors. No deaths due to cervical cancer have been documented in women younger than 20 years. The United States National Cancer Institute publishes data on the prevalence of worldwide cervical cancer via their online database.
The incidence of cervical cancer has decreased dramatically during the last century because of the implementation of the Papanicolaou test (Pap Test, or Pap smear), beginning in the 1930s and 1940s. However, between 1990 and 2001, the annual number of estimated new invasive cervical cancers remained relatively constant (13,500 and 12,900, respectively). In the United States, 2.5 million women are estimated to have an annual cytologic diagnosis of a low-grade cervical cancer precursor.
The percentages of other cancers caused by oncogenic HPV are as follows [34] :
-
Anal cancer - 90%
-
Vulvar cancer - 40%
-
Vaginal cancer - 40%
-
Oropharyngeal cancer - 12%
-
Oral cancer - 3%
International statistics
Globally, HPV infection is the most common STD. [35, 36] Genital warts have affected as many as 30 million individuals worldwide. A study in Finland in the mid-1980s found that the annual incidence of cytologic cervical HPV infection was 7%. [37] A study of Finnish males determined that 6.5% had evidence of HPV in exfoliative cells obtained from the urethra and genital epithelium. [38]
In many lesser-developed countries, cervical cancer is the most common cancer among women because of the lack of effective screening programs that monitor cervical cytology by Pap smear. [39] However, a single round of HPV screening has been demonstrated to be far superior to conventional cytology in reducing the incidence of cervical cancer morbidity and mortality. [40]
The prevalence of high-risk HPV in women with normal cervical cytology varies among the different regions of the world. Although the global HPV prevalence was estimated to be approximately 12%, higher prevalences were noted in sub-Saharan Africa (24%), eastern Europe (21.4%), and Latin America (16.1%). [41]
In many developing nations, cervical cancer is the leading cause of cancer mortality among women. Worldwide, it is the second most common cause of cancer mortality among women. The World Health Organization (WHO) estimates that 570,000 new cases of cervical cancers occurred globally in 2018, and approximately 311,000 women died of cervical cancer during the same year. [42]
Age-related demographics
People of any age may develop common warts. HPV infects more than 50% of sexually active adults. Genital infection generally occurs during the sexually active period in a person’s life, and infections increase with the number of sexual partners.
The prevalence of anogenital mucosal HPV infections is highest among college-aged women and men. The prevalence of HPV infection stratified by age in US females is as follows [43] :
-
Age 14-59 years - 26.8%
-
Age 14-19 years - 24.5%
-
Age 20-24 years - 44.8%
-
Age 25-29 years - 27.4%
-
Age 30-39 years - 27.5%
-
Age 40-49 years - 25.2%
-
Age 50-59 years - 19.6%
Thus, the highest rates of genital HPV infection are in young, sexually active females. This incidence is independent of the number of lifetime sexual partners. Most of these infections (90%) are transient. [44, 45, 46] An estimated 5.6% of sexually active adults in the United States aged 18-59 years have been diagnosed with genital warts by a medical provider. [47]
A cytologic screening of the cervix in more than 400,000 women supported a higher incidence of HPV in young women. This study found that the rate of HPV infection in women younger than 30 years is double that in women older than 30 years. [48]
The reason for the higher prevalence in younger women is not completely understood. Some investigators hypothesize that older women have fewer sexual partners and, consequently, less exposure to HPV. An alternative theory is that by age 30 years, women have acquired immunity to HPV. [49]
The presence of genital condyloma in the pediatric population presents a diagnostic and therapeutic challenge. [50] Vertical transmission of HPV can occur via in utero exposure to amniotic fluid or transmission of HPV from the maternal genital tract.
An incubation period of several months is usually required between virus infection at delivery and clinical manifestations in the infant. The average latency period is 3 months, but periods as long as 20 months have been reported. [51] Cases of childhood condylomata outside a reasonable incubation period after vertical transmission should arouse suspicion of child abuse. Treatment of condyloma in the infant includes excision under general anesthesia or the use of podophyllin. [52]
Nongenital cutaneous warts are more common among teenagers and adults who work as meat, poultry, and fish handlers. The incidence approaches 10% in child and young adult populations. However, nongenital cutaneous warts rarely occur in people younger than 5 years and usually regress within 2 years.
EV develops at an average age of onset of 6 years. Beginning in the fourth decade of life, the lesions can undergo malignant transformation into invasive SCC.
Sex-related demographics
The overall prevalence of HPV in women is reported to be 22-35%. In men, the prevalence is reported to be 2-35%, depending on the sexual practices of the population being studied. However, a well-defined population study found the female-to-male ratio to be 1.4:1, [20] and CDC reports demonstrated that this disease affects females more frequently than males.
The prevalence of condyloma acuminatum seems to be similar in men and women. A study from an STD clinic found that 13% of men and 9% of women had condylomata acuminata. [23] HPV infections are reported more frequently in US college females [53] than in male counterparts. This presumed higher incidence of HPV infection in females may be the result of detection of HPV infection in cytologic smears performed for cervical cancer screening. Females seek medical care for genital warts more frequently than men do. [26]
Race-related demographics
In the United States, African Americans have a rate of HPV infection that is 1.5 times higher than their white counterparts. However, most studies indicate that no racial predilection exists for the acquisition of genital warts.
Dinh et al analyzed data from the 1999-2004 National Health and Nutrition Examination Surveys, which collected data from a random sample of the United States civilian population. These investigators reported that the prevalence of genital warts was higher in non-Hispanic whites than in other racial or ethnic groups. [47] One US survey reported that among women, the prevalence of HPV infection due to any HPV type was 39% for non-Hispanic blacks, and 24% for non-Hispanic whites and Mexican Americans. [43]
From 1987 to 1991, the age-adjusted cervical cancer death rate reported by the US National Cancer Institute was higher among black women than among white women, with a ratio of 6:1.
Prognosis
HPV infection primarily involves the basal epithelial cells. As a result, both recurrences and regressions are common. Prognosis is good, and most cases of genital warts are amenable to treatment. Patients who do not develop immunity to HPV can develop potentially serious sequelae.
Genital warts may spontaneously regress, remain unchanged, or increase in size. Treatment of these lesions does not affect the development of cervical cancer. Approximately two thirds of patients with nongenital cutaneous warts experience a spontaneous regression within 2 years; however, some new warts may appear.
HPV infection of the vulva can result in the development of vulvar intraepithelial neoplasia (dysplasia) or squamous cell carcinoma of the vulva. Most research indicates that HPV infection is strongly associated with the development of cervical dysplasia and cervical carcinoma. HPV confers more than 99% of the attributable risk for the development of cervical dysplasia. [54] Vaginal dysplasia and vaginal cancer are also associated with HPV exposure.
Histologic evidence of HPV infection on a cervical Pap smear is similar to mild dysplasia. This subclinical disease often spontaneously regresses.
A direct correlation exists between anogenital HPV infection and measures of sexual activity, such as the age of first intercourse and the lifetime number of sexual partners. Women with a history of HGSIL of the cervix or invasive SCC of the cervix are at increased risk for subsequent development of invasive cancer in other tissues of the anogenital-mucosal category, particularly vaginal and anal carcinoma. In these patients, the relative risk of vaginal carcinoma is 5.6, and the risk of anal carcinoma is 4.
Women who are immunocompromised as a result of immunosuppressive drug therapy or HIV infection are at higher risk for persistent disease. These women are more likely to develop dysplasia or cancer of the vulva, vagina, or cervix.
Anal cancer has been strongly associated with male homosexuality and specific male practices, such as engaging in receptive anal intercourse. Relative risk is 33. However, the overall disease prevalence is higher in women than in men, with a female-to-male ratio of 1.5:1.
Men who are infected with HPV are at risk for genital warts. The 24-month risk varied from 57.9% in men who were infected with HPV type 6 or type 11 to 2% in men who were infected with other HPV types. [55]
Patients who are immunosuppressed, particularly those with cutaneous malignant lesions, have a much higher incidence of EV-HPV infection than the general population. These lesions can undergo malignant transformation. About 10% of patients with EV originate from consanguineous marriages, suggesting an autosomal recessive mode of inheritance (see Epidermodysplasia Verruciformis).
Most patients with EV experience progression of their disease in the third or fourth decades of life. Malignant transformation usually arises from actinic keratoses, particularly in patients who are exposed to irradiation. Patients who remain protected from x-rays and sun exposure generally have satisfactory health.
As many as 20% of patients with genital warts have other sexually transmitted diseases concurrently (Rochester, Minnesota). [22] In an Australian sexual health clinic, 5% of genital wart patients were found to also have chlamydia and/or gonorrhea. [56]
Patient Education
Treatment of genital warts can be difficult and lengthy. Patient expectations should be set appropriately. Counsel patients on their risk of infectivity to others, and advise them of their increased risk of having acquired other STDs. Remind them that genital warts resolve spontaneously in 20-30% of women within 3 months. [28]
Educating women, particularly those who are socially and economically disadvantaged, about behaviors that enhance sexual risk reduction has a proven benefit in reducing the incidence of STDs. Reducing the incidence of STDs potentially could decrease HPV transmission and, consequently, the incidence of cervical carcinoma.
Inform patients that genital HPV is an STD and that the only way to prevent HPV infection is to avoid direct contact with the virus, which is transmitted by skin-to-skin contact. Instruct them to use condoms with vaginal, anal, or oral sex because the virus may be found in the semen in the absence of visible warts. Remind them that latex condoms offer some, but not complete, protection from transmission.
The benefit of evaluating sex partners of patients with genital warts has been apparent. Several consort studies documented that 30% of female consorts and 80% of male consorts had HPV infection. Usually, the same type of HPV involved both parties, and often they were HPV 6, 11, 16, and 18. If the sexual partner has visible genital warts, sexual contact should be avoided until treatment is completed.
For patient education resources, see the Women’s Health Center, the Pregnancy Center, and the Cancer Center, as well as Genital Warts, Plantar Warts, and Pap Smear.
-
Human papillomavirus (HPV). Condyloma acuminatum in a patient with a history of an allograft renal transplant.
-
Human papillomavirus (HPV). Note the extensive labial involvement.
-
Human papillomavirus (HPV). Anal condyloma acuminatum.
-
Human papillomavirus (HPV). These condylomata extend to the anal verge.
-
Verrucous warts in patient with HIV infection.
-
Plantar warts.
-
Flat wart.
-
"Cauliflower" condyloma of penis.
-
Small papilloma on shaft of penis.
-
Human papillomavirus (HPV). Verruca vulgaris on the lateral border of the tongue exhibits the multiple, sharp-tipped, white, verrucous appearance, which is classic for this lesion in the oral cavity. Not all verrucae are so clinically diagnostic. Courtesy of Rose Yin Geist, DDS.
-
This is a verruca vulgaris of the anterior maxillary gingiva in a healthy young male. He had recently resolved a wart on his finger.
-
These small papillomas on the lateral tongue of a young woman showed histologic evidence of HPV in the form of extensive koilocytosis.
-
Human papillomavirus (HPV) lesion on the lingual frenum. Some patients with condyloma acuminatum present with multiple oral lesions. Courtesy of A.K. ElGeneidy, DDS.
-
Human papillomavirus (HPV). Condylomata on the lower lip, as well as other sites at the initial presentation. This presentation is unusually extensive. Multiple condylomata may be synchronous or metachronous. This patient did not present with genital condylomata. Courtesy of A.K. ElGeneidy, DDS.
-
Human papillomavirus (HPV). Heck disease in the buccal mucosa of a 7-year-old boy. Courtesy of Sheldon Mintz, DDS.
-
Human papillomavirus (HPV). Verrucae and papillomas appear as frondlike epithelial proliferations. Verrucae tend to be more keratinized with sharper projections than papillomas.
-
Human papillomavirus (HPV). Condyloma acuminatum generally has a papillary architecture and may microscopically resemble verruca vulgaris and papilloma (hematoxylin and eosin stain, original magnification X10). Courtesy of AK ElGeneidy, DDS.
-
Human papillomavirus (HPV). Koilocytes in the upper epithelium are a helpful, although not completely reliable, indication that a lesion is associated with human papillomavirus. Koilocytes display a dark small nucleus with clear cytoplasm (hematoxylin and eosin stain, original magnification X100). Courtesy of Sheldon Mintz, DDS.
-
Human papillomavirus (HPV). Condyloma acuminatum may show brisk mitotic activity, although oral condyloma acuminatum is not considered a premalignant lesion (hematoxylin and eosin stain, original magnification X40). Courtesy of A.K. ElGeneidy, DDS.
-
The left panel is transudation of serum antibodies to the site of human papillomavirus infection, and the right panel is exudation of serum antibodies to the site of human papillomavirus infection.
-
The figure shows proposed mechanisms used by the human papillomavirus vaccine to neutralize antibodies and protect against infection.
-
Figure showing how human papillomavirus penetrates the basal layer and eventually is released at the surface.