Practice Essentials
Papillary thyroid carcinoma (PTC) is the most common form of well-differentiated thyroid cancer, and the most common form of thyroid cancer to result from exposure to radiation. Papillary carcinoma appears as an irregular solid or cystic mass or nodule in a normal thyroid parenchyma.
Despite its well-differentiated characteristics, papillary carcinoma may be overtly or minimally invasive. In fact, these tumors may spread easily to other organs. Papillary tumors have a propensity to invade lymphatics but are less likely to invade blood vessels.
PTC has several histologic variants, which show different patterns of behavior. For example, tall cell PTC (TCPTC) is an uncommon but relatively aggressive variant that is more likely to demonstrate invasion, metastasis, and recurrence. [1] In contrast, the encapsulated follicular variant of PTC (eFVPTC) without capsular or vascular invasion poses so little risk that the American Thyroid Association has recommended that it no longer be considered a carcinoma, and instead be reclassified as noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP). [2]
The life expectancy of patients with PTC is also related to their age. The prognosis is better for younger patients than for patients who are older than 45 years.
Of patients with papillary cancers, about 11% present with metastases outside the neck and mediastinum. Some years ago, lymph node metastases in the cervical area were thought to be aberrant (supernumerary) thyroids because they contained well-differentiated papillary thyroid cancer, but occult cervical lymph node metastases are now known to be a common finding in this disease. [3, 4, 5, 6, 7, 8]
Fine-needle aspiration biopsy (FNAB) is considered the best first-line diagnostic procedure for a thyroid nodule (see Workup). Surgery is the definitive management of PTC. Approximately 4-6 weeks after surgical thyroid removal, patients may have radioiodine therapy to detect and destroy any metastasis and residual tissue in the thyroid. See Treatment.
For patient education information, see Thyroid Cancer.
For discussion of other thyroid cancers, see the following:
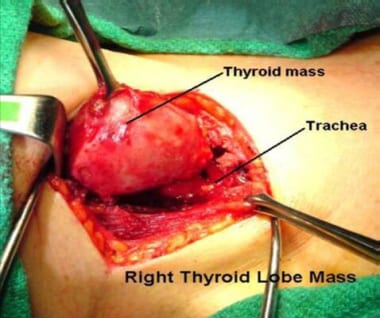
An image depicting a thyroid mass can be seen below.
Pathophysiology
Several chromosomal rearrangements have been identified in papillary thyroid carcinoma. The first oncogenic events identified in papillary thyroid carcinoma were chromosomal rearrangements involving the rearranged during transfection (RET) proto-oncogene, which arises from a paracentric inversion of chromosome 10. [9] RET fusion proteins (the RET/PTC family) appear to play an oncogenic role in approximately 20% of papillary thyroid carcinomas, with RET/PTC1, RET/PTC2, and RET/PTC3 accounting for most cases. [10, 9] In addition, the NTRK1 and the MET proto-oncogene may be overexpressed and/or amplified. [11, 12]
Evidence also suggests that some molecules that physiologically regulate the growth of the thyrocytes, such as interleukin-1 and interleukin-8, or other cytokines (eg, insulinlike growth factor 1, transforming growth factor beta, epidermal growth factor) could play a role in the pathogenesis of this cancer.
Mutation in the BRAF gene resulting in the BRAF V60E protein is prominent in papillary thyroid carcinoma. A single-institution study by Mathur et al reported increasing rates of BRAF V600E mutations in papillary thyroid cancer from 1991 to 2005, suggesting that this may be contributing to the rise in thyroid cancer rates. [13] The BRAF V600E mutation is associated with aggressive clinicopathological characteristics of papillary thyroid carcinoma, including lymph node metastasis, extrathyroidal invasion, and loss of radioiodine avidity, which may lead to failure of radioiodine treatment and disease recurrence. [14, 15]
There is also a clear association between radiation exposure (from radiotherapy or fallout) and incidence of papillary thyroid carcinoma. [16] Port et al reported that papillary thyroid cancers in patients exposed to radiation from the Chernobyl accident could be completely distinguished from sporadic papillary thyroid cancers in patients with no history of radiation exposure, on the basis of gene expression patterns involving seven genes (ie, SFRP1, MMP1, ESM1, KRTAP2-1, COL13A1, BAALC, PAGE1). [17]
Etiology
Ionizing radiation
The thyroid is particularly sensitive to the effects of ionizing radiation. Both accidental and medical exposure to ionizing radiation has been linked to increased risk for thyroid cancer.
Approximately 7% of individuals exposed to the atomic bombs in Japan developed thyroid cancers. [18] Individuals, especially children, who lived in Ukraine during the time of the Chernobyl nuclear event may have increased risk of papillary thyroid cancer. [19]
From 1920-1960, therapeutic irradiation was used to treat tumors and benign conditions, including acne; excessive facial hair; tuberculosis in the neck; fungal diseases of the scalp; sore throats; chronic coughs; and enlargement of the thymus, tonsils, and adenoids. Approximately 10% of individuals who were treated with head and neck irradiation for such disorders developed thyroid cancer after a latency period of 30 years.
Exposure to diagnostic x-ray beams does not increase the risk of developing thyroid cancers. For adult patients who receive 1 Gy of ionizing radiation to the thyroid, the proportion of thyroid cancers thought to be due to radiation exposure was 88%. [20]
However, patients who receive radiotherapy for certain types of head and neck cancer, especially during childhood, may have an increased risk of developing thyroid cancer. For the pediatric population, doses in the range of 50-100 mGy have been associated with an increased risk of thyroid cancer, with a linear dose response up to about 10-20 Gy. This risk persists for about 4 years from exposure. [20]
Hashimoto thyroiditis
Patients with a history of Hashimoto thyroiditis are at increased risk for papillary thyroid cancer. In a study by Bradly et al, the overall incidence of incidental papillary carcinoma (IPC) in benign operatively resected thyroid disease was 12%, with Hashimoto thyroiditis being associated with the highest rate of IPC. [21] According to this study and others, the association of IPCs with Hashimoto thyroiditis may indicate a causal link to thyroid cancer. [22]
Obesity
One of every six papillary thyroid cancers (PTC) and two thirds of all large PTC tumors in the United States from 1995 to 2015 were attributable to being overweight or obese, according to an analysis of data from three large national US databases. Kitahara et al estimated that total relative risk for PTC was 1.26 for persons who are overweight (body mass index [BMI] 25.0-29.0 kg/m2) and 1.30 for those who are obese (BMI ≥30.0), compared with persons with normal-weight BMI (18.5-24.9). Risk for large (> 4 cm) PTCs was increased nearly 3-fold (hazard ratio [HR] = 2.93, 95% CI 1.25-6.87) with being overweight, and was increased more than 5-fold (HR = 5.42, 95% CI 2.24-13.1) with obesity. [23]
Familial syndromes
Unlike medullary thyroid carcinoma, papillary thyroid cancer is not a part of multiple endocrine neoplasia syndromes. However, uncommon familial syndromes such as familial adenomatous polyposis (FAP), Gardner syndrome and Cowden disease may be associated with thyroid papillary tumors in about 5% of cases. [24]
In particular, FAP is associated with elevated risk of the rare cribriform-morula variant of papillary thyroid carcinoma (CMV-PTC). A study of 129 Japanese patients with FAP who underwent screening with neck ultrasonography found 11 cases of papillary thyroid cancer, eight of which were CMV-PTC. All the patients with CMV-PTC were women 35 years of age or younger. [25]
Other risk factors
Several reports have shown a relationship between iodine deficiency and the incidence of thyroid carcinomas. Many other conditions have been considered as predisposing to papillary thyroid cancer, including oral contraceptive use, benign thyroid nodules, late menarche, and late age at first birth. [26, 27] Tobacco smoking seems to be associated with a decreased risk of thyroid cancer, but, obviously, it poses more health hazards than benefits. [28]
Epidemiology
Thyroid cancers account for only 1.5% of all cancers in adults and 3% of all cancers in children. In females, however, thyroid cancers are the seventh most common cancer, comprising 3% of all cases. [29] Although the rate of new cases had been increasing in recent decades, [30] the incidence rate declined by 2.5% per year from 2014 to 2018, due in part to the adoption of more conservative diagnostic criteria. [29]
The American Cancer Society (ACS) estimates that in 2022, 43,800 new thyroid cancers will occur, 31,940 in women and 11,860 in men; the ACS estimates that 2230 deaths from thyroid cancer will occur, 1160 in women and 1070 in men. [29] The highest incidence of thyroid carcinomas in the world is found among female Chinese residents of Hawaii.
Of all thyroid cancers, 74-80% of cases are papillary cancer. Follicular carcinoma incidences are higher in regions where goiter is common.
Mortality/morbidity
In contrast to many other cancers, PTC is almost always curable. Most thyroid cancers grow slowly and are associated with a very favorable prognosis. The mean survival rate after 10 years is higher than 90%, and is 100% in very young patients with minimal nonmetastatic disease. Distant spread (ie, to lungs or bones) is very uncommon.
The 5-year relative survival rates by stage of diagnosis are as follows [31] :
-
All stages: 98.3%
-
Local: 99.9%
-
Regional: 98.3%
-
Distant: 53.3%
Sex
Thyroid cancer is approximately three times more common in females than males. The female-to-male ratio varies by patient age, as follows:
-
In patients younger than 19 years, the female-to-male ratio is 3.2:1
-
In patients aged 20-45 years, the female-to-male ratio is 3.6:1
-
In patients older than 45 years, the female-to-male ratio is 2.8:1
Race
PTC occurs more frequently in Whites than in Blacks. In 2019, incidence rates were as follows [31] :
2019 Incidence Rates per 100,000 US Population (Open Table in a new window)
| Race | Females | Males |
|---|---|---|
| White | 30.8 | 14.3 |
| Black | 18.5 | 5.6 |
| Asian/Pacific Islander | 37.2 | 10.5 |
| American Indian/Alaska Native | 41.7* | —* |
| Hispanic | 32.8 | 10.3 |
*Less than 16 cases in 2019; 2018 value used when applicable
Age
Thyroid carcinoma occurs in persons of all ages, but is most often diagnosed in persons aged 45–54; median age at diagnosis is 51 years. [31] In the younger population, papillary thyroid carcinoma tends to occur more frequently than follicular carcinoma, with a peak in patients aged 30-50 years.
Prognosis
The prognosis in patients with papillary thyroid cancer (PTC) is related to age, sex, and stage. Prognosis is better in females and in patients younger than 40 years. In general, if the cancer does not extend beyond the capsule of the gland, life expectancy is minimally affected. The survival rate is at least 95% with appropriate treatments.
If neglected, any thyroid cancer may result in symptoms because of compression and/or infiltration of the cancer mass into the surrounding tissues, and the PTC may metastasize to lung and bone. Metastases, in descending order of frequency, are most common in the neck lymph nodes and lung, followed by the bone, brain, liver, and other sites. Metastatic potential seems to be a function of the primary tumor size. Metastases in the absence of thyroid pathology on physical examination are rare in patients with microscopic papillary carcinoma (occult carcinomas).
In a long-term follow-up study of children and adolescents with PTC, Hay et al found that all-causes mortality rates did not exceed expectation through 20 years after treatment, but the number of deaths was significantly higher than predicted from 30 through 50 years afterward. Nonthyroid malignancy accounted for 68% of deaths, and, of that group, 73% had received postoperative therapeutic irradiation. [32]
A study by Yu et al found that papillary thyroid microcarcinomas are generally associated with an excellent prognosis; however, 0.5% of patients may die. Risk factors for overall survival include the following:
-
Age older than 45 years
-
Male sex
-
Minority race*
-
Node metastases
-
Extrathyroidal invasion
-
Distant metastases
However, it should be noted that structural and systemic racism has been shown to be a confounding risk factor in the minority population. [33]
If two or more risk factors are present, patients should be considered for more aggressive management. [34]
A study by Miyauchi et al found that serum thyroglobulin doubling time was a significant prognostic predictor in patients with papillary thyroid carcinoma. The authors concluded that this finding was superior to classical prognostic factors, including TNM stage, age, and gender. [35]
In a study of 39,562 patients with papillary thyroid carcinoma from the National Cancer Data Base, risk factors for central lymph node metastasis included the following [36] :
-
Age ≤45 years
-
Male sex
-
Asian race
-
Tumor > 1 cm
A family history of papillary thyroid carcinoma is an independent risk factor for disease recurrence in patients with papillary thyroid microcarcinoma. [37]
For patients found to be at intermediate risk on the basis of established prognostic factors, Brennan and colleagues report that gene expression signatures may permit classification into intermediate-good prognosis and intermediate-poor prognosis groups. The authors note that their findings require validation, but they observe that tests that routinely measure expression of hundreds of genes are already commercially available. [38]
A retrospective study of clinicopathological outcomes of 6282 patients with PTC demonstrated significant differences in recurrence and disease-specific patient survival with three histologic variants of PTC. Particularly in patients at least 45 years old, patients with tall-cell PTC had the worse prognosis; those with conventional PTC had an intermediate prognosis, and those with follicular-variant PTC had the best prognosis. [1]
Indeed, the American Thyroid Association has recommended that the encapsulated follicular variant of PTC (eFVPTC) without capsular or vascular invasion be reclassified as noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP). [2] Recurrence of NIFTP is extremely rare, even in patients treated with surgery alone, without radioactive iodine therapy, and ceasing to classify it as a cancer may help clinicians avoid unnecessary aggressive treatment. [39]
Diffuse sclerosing papillary thyroid carcinoma (DSPTC) is an uncommon variant of PTC. A systematic review and meta-analysis by Vuong et al concluded that DSPTC should be considered a high-risk condition, because it has a high propensity for tumor invasion, metastasis, relapse, and mortality, compared with classic PTC. [40]
-
Standard open thyroidectomy.
-
Algorithm for the workup of a solitary thyroid nodule. FNAB = fine needle aspiration biopsy.
-
Planar and color Doppler image showing a cystic papillary thyroid carcinoma.