Background
The diaphragm is the dome-shaped muscle that separates the thoracic and abdominal cavities; it is the major muscle of respiration. Dysfunction of the diaphragm may be an asymptomatic incidental finding, or it may be associated with dyspnea, decreased exercise tolerance, sleep disturbances, respiratory failure, and death. [1, 2, 3, 4]
Diaphragmatic dysfunction may result from disease processes in the central nervous system, the phrenic nerves, the neuromuscular junction, or anatomically. Dysfunction may range in severity from a partial loss of muscle contraction to complete paralysis, and it may involve one or both hemidiaphragms.
The diagnosis and management of unilateral and bilateral diaphragm dysfunction may be challenging for the clinician because of its relative rarity and subtle clinical manifestations, and it is likely underdiagnosed. [5] The workup for suspected diaphragm dysfunction includes chest radiography, pulmonary function testing, fluoroscopy, phrenic nerve conduction studies (NCS), needle electromyogram (EMG) of the diaphragm, and transdiaphragmatic pressure measurements. Each modality has strengths and weaknesses, but all of these produce false-positive and false-negative findings. [6]
Pathophysiology
Disorders of neuromusculature
During normal respiration, the brainstem sends action potentials to the third through fifth cervical spine levels, which then give off dorsal rami that join to form the phrenic nerves bilaterally. The phrenic nerves then traverse the neck and thorax and innervate the diaphragm. The successful impulse of respiratory stimulus from the brain to the diaphragm can be compromised by an interruption of the phrenic nerve at any point along this course.
Traumatic injury to the head or brainstem prevents nerve signals from reaching the phrenic nerve. Generally, injuries that affect the brain and brainstem are catastrophic, with the chance of survival being poor. [7] Other etiologies of central nervous system damage that may affect the brainstem include multiple sclerosis, stroke, Arnold-Chiari malformations, and poliomyelitis.
Injuries or disease processes that affect the phrenic nerves along their course are well described and impair the transmission of action potentials from the brainstem to the diaphragm. Numerous clinical entities can affect the phrenic nerve directly, including trauma, external compression from a tumor, cardiac or thoracic surgery, chiropractic cervical spine manipulation, radiation therapy, demyelinating diseases (eg, Guillain-Barré syndrome, chronic inflammatory demyelinating polyneuropathy, Charcot-Marie-Tooth), uremia, lead neuropathy, and postinfectious neuropathies.
Diseases of the neuromuscular junction can inhibit the production, release, or binding of neurotransmitters at phrenic-diaphragmatic synapses. These processes include myasthenia gravis, Lambert-Eaton syndrome, botulism, organophosphate poisoning.
Diseases that affect the muscle fibers of the diaphragm may result in decreased muscle strength resulting in a decreased ability to generate transdiaphragmatic pressure gradients and thereby less negative maximal inspiratory pressures. These processes include muscular dystrophies, glucocorticoid myopathy, statin myopathy, malnutrition, thyroid disorders, and disuse atrophy in mechanically ventilated patients. [8, 9, 10]
Disorders of anatomy
Anatomic disorders of the diaphragm are typically classified into two broad categories, congenital and acquired.
Congenital diaphragmatic hernias occur when the muscular entities of the diaphragm do not develop normally, usually resulting in displacement of the abdominal components into the thorax (see the image below). [11] The underlying etiologies of these diaphragmatic hernias are not well understood, but a number of studies implicate abnormalities of the retinoid system which may result from maternal vitamin A deficiency. [12, 13, 7]
 Diaphragm Disorders (Diaphragmatic dysfunction). Congenital diaphragmatic hernia is shown in this coronal obstetric ultrasound (the patient's head is to the right of the image; the thorax is center, and the abdomen is left). The stomach (st) and heart (hrt) are both within the thorax. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Cdh0002.jpg), author Dr Laughlin Dawes.
Diaphragm Disorders (Diaphragmatic dysfunction). Congenital diaphragmatic hernia is shown in this coronal obstetric ultrasound (the patient's head is to the right of the image; the thorax is center, and the abdomen is left). The stomach (st) and heart (hrt) are both within the thorax. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Cdh0002.jpg), author Dr Laughlin Dawes.
Congenital diaphragmatic hernias are classified by the position of the defect. Bochdalek hernias, which represent between 80% and 90% of congenital diaphragmatic hernias, are posterolateral defects of the diaphragm that result in either failure in the development of the pleuroperitoneal folds or improper or absent migration of the diaphragmatic musculature. [14, 15, 16] Morgagni hernias involve the anterior portion of the diaphragm (see the following image). Congenital diaphragmatic hernias involving the central portion of the diaphragm are rare.
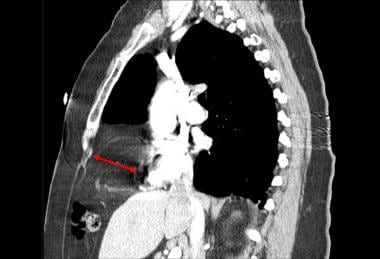 Diaphragm Disorders (Diaphragmatic dysfunction). Sagittal computed tomography scan of the chest with intravenous contrast demonstrates a Morgagni hernia (red arrow) containing abdominal fat. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Morgagni_Hernia.PNG), author Jason Robert Young, MD.
Diaphragm Disorders (Diaphragmatic dysfunction). Sagittal computed tomography scan of the chest with intravenous contrast demonstrates a Morgagni hernia (red arrow) containing abdominal fat. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Morgagni_Hernia.PNG), author Jason Robert Young, MD.
The most common cause of acquired diaphragmatic disorders is trauma. [17, 18] Traumatic diaphragmatic rupture can occur secondary to both blunt and penetrating trauma. Up to 65% of diaphragmatic ruptures are a result of penetrating injury from stab or gunshot wounds. The remainder of traumatic diaphragmatic injury is blunt trauma sustained from motor vehicle accidents, falls, or direct impacts. Left-sided rupture is more common, occurring in 65%-75% of blunt trauma cases. [19, 20, 21]
Etiology
The etiology of diaphragmatic dysfunction is most easily separated into anatomic, neurologic, neuromuscular junction, and myopathic disorders.
Anatomic defects include the following:
-
Congenital defects: Bochdalek hernia, Morgagni hernia, eventration of the diaphragm, and diaphragmatic agenesis
-
Acquired defects: Blunt traumatic rupture, penetrating injuries, and iatrogenic injury during surgery or other invasive procedures
Neurologic defects are include the following:
-
Brainstem stroke
-
Spinal cord disorders: Trauma to the cervical spinal cord, syringomyelia, poliomyelitis, anterior horn cell disease
-
Cervical spondylosis
-
Cervical chiropractic manipulation [22]
-
Guillain-Barré syndrome [25]
-
Diabetic neuropathy
-
Alcoholic neuropathy
-
Viral and postviral neuropathy (polio, West Nile virus, herpes zoster, human immunodeficiency virus [26] )
-
Heavy metal toxicity (lead, arsenic) [27]
-
Multiple sclerosis
-
Amyotrophic lateral sclerosis
-
Connective-tissue disease (eg, systemic lupus erythematosus [SLE], rheumatoid arthritis)
Myopathic causes of diaphragmatic paralysis are include the following:
-
Disuse atrophy due to mechanical ventilation [9]
-
Malnutrition
-
Electrolyte disturbances (hypophosphatemia, hypokalemia, hypocalcemia) [28]
-
Limb-girdle dystrophy
-
Hyperthyroidism or hypothyroidism
-
Acid maltase deficiency
-
SLE
-
Dermatomyositis
-
Mixed connective-tissue disease
-
Amyloidosis
-
Myasthenia gravis
-
Muscular disorders: Myotonic dystrophies, Duchenne muscular dystrophy, and metabolic myopathies
Epidemiology
The exact frequency of diaphragmatic disorders is not known and is difficult to estimate. It is likely that diaphragmatic disorders are underdiagnosed due to subtle clinical findings and varying etiologies. However, the incidence of many specific causes of diaphragmatic disorders is known.
For example, congenital diaphragmatic hernia (CDH) affects 1 in 3500 live-born infants. [29] Coronary artery bypass grafting (CABG) surgery is associated with lesions of the phrenic nerves resulting in postoperative diaphragmatic paralysis, with reported incidences varying from 1% to 5%, with some reports as high as 60%. Internal mammary artery harvesting and the use of frozen slurry during cardiac surgery increase the risk of phrenic nerve injury. [5, 30, 31] Up to 25% of patients with Guillain-Barre disease will develop diaphragmatic weakness requiring mechanical ventilation. [25]
Prognosis
The prognostic and clinical evolution of diaphragm dysfunction are variable and related to the underlying etiology and the extent of the dysfunction.
Patients with congenital diaphragmatic hernias generally present in the neonatal period, with associated postsurgical survival rates of 60%-80%. Despite improvements in surgical correction over the years, complications and comorbidities still affect 20%-40% of the treated children. These include both surgical complications (recurrence, postoperative adhesions and obstruction, stenosis, strictures, and recurrent fistulae) as well as pulmonary problems (chronic lung disease, obstructive and restrictive pulmonary dysfunction), gastrointestinal problems (dysphagia, gastroesophageal reflux, impaired intestinal motility), and failure to thrive. [29]
Patients with diaphragmatic disorders due to transient neuropathies such as postviral neuropathy or Guillain-Barré syndrome as well as patients with iatrogenic phrenic nerve injury from cardiac or thyroid surgery generally have a favorable prognosis, with functional recovery in up to 69% of patients within 2 years. [32, 30, 33]
In the intensive care unit, ventilator-induced diaphragm dysfunction is a negative prognostic marker, with clinical impact on the weaning outcome, length of mechanical ventilation, survival, and long-term outcome. [34, 35] The mechanisms underlying this process include weakness of the diaphragm from defective contractility and reduced diaphragm muscle mass, as well as oxidative loads, structural damage, and muscle fiber remodeling. [34, 36]
Persons with high cervical spine fractures generally fare worse than individuals with transient neuropathies. Trauma to the cervical spine at C1-C2 results in complete diaphragmatic paralysis. Trauma to C3 and C4 may lead to substantial loss of diaphragm function whereas trauma to C4 and C5 are much less likely to require ventilatory support. [7] In the context of degenerative myopathies or neurologic diseases, respiratory muscle weakness frequently progresses relentlessly with the underlying disease and may progress to fulminate respiratory failure. Patients with amyotrophic lateral sclerosis have universally fatal outcomes, but respiratory muscle strength has been demonstrated to be a predictive marker for prognosis. [37]
-
Diaphragm Disorders (Diaphragmatic dysfunction). Radiograph of a man who fell 45 ft from scaffolding, through plate glass windows, and onto the ground. Intraoperatively, he had a completely avulsed diaphragm on the left side. The patient subsequently recovered after a 45-day hospital course of treatment.
-
Diaphragm Disorders (Diaphragmatic dysfunction). Congenital diaphragmatic hernia is shown in this coronal obstetric ultrasound (the patient's head is to the right of the image; the thorax is center, and the abdomen is left). The stomach (st) and heart (hrt) are both within the thorax. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Cdh0002.jpg), author Dr Laughlin Dawes.
-
Diaphragm Disorders (Diaphragmatic dysfunction). Sagittal computed tomography scan of the chest with intravenous contrast demonstrates a Morgagni hernia (red arrow) containing abdominal fat. Courtesy of Wikipedia (https://en.wikipedia.org/wiki/File:Morgagni_Hernia.PNG), author Jason Robert Young, MD.






