Background
In January 2014, Colorado became the first state in the United States to legalize marijuana for recreational purposes, marking the beginning of what will likely become the end of marijuana prohibition. Marijuana was legal in the United States until 1937, when Congress passed the Marijuana Tax Act, effectively making the drug illegal. The American Medical Association (AMA) opposed the legislation at the time of its passage. Additionally, from 1850 to 1942, marijuana was listed in the US Pharmacopoeia, the official list of recognized medical drugs. Cannabis was marketed as extract or tincture by several pharmaceutical companies and used for ailments such as anxiety and lack of appetite.
Despite the medical establishment's views on the benefits of marijuana, the passage of the Comprehensive Drug Abuse Prevention and Control Act of 1970 classified marijuana as a Schedule I drug, defined as a category of drugs not considered legitimate for medical use. Other Schedule I drugs include heroin, phencyclidine (PCP), and lysergic acid diethylamide (LSD). [1]
A significant paradox and disconnect continues to exist between the federal government's outdated policies versus changing state laws, the general public's perception and acceptance of marijuana, and even former President Barack Obama. In discussing his own marijuana use with New Yorker editor David Remnick, President Obama commented, "As has been well documented, I smoked pot as a kid, and I view it as a bad habit and a vice, not very different from the cigarettes that I smoked as a young person up through a big chunk of my adult life. I don’t think it is more dangerous than alcohol." He elaborated that marijuana was actually less dangerous than alcohol "in terms of its impact on the individual consumer." [2]
Marijuana laws are constantly changing throughout all 50 states ranging from fully legalized to illegal. Current status of marijuana laws by state are available.
In 2014, 38 states and the District of Columbia had legalized marijuana for medicinal purposes, with many others actively considering the issue. Additionally, a survey by NBC News/The Wall Street Journal shows that the majority of Americans support legalizing marijuana. [3] Federal policy changes have attempted to redress the inconsistencies between federal and state law. In 2009, the Justice Department issued a federal medical marijuana policy memo to the Drug Enforcement Administration (DEA), Federal Bureau of Investigation (FBI), and US Attorneys instructing prosecutors not to target medicinal marijuana patients and their providers for federal prosecution in states where medicinal marijuana has been legalized. In the summer of 2010, the Department of Veteran Affairs issued a department directive to "formally allow patients treated at its hospitals and clinics to use medical marijuana in states where it is legal, a policy clarification that veterans have sought for years." [4]
In the Netherlands, where the distribution of marijuana has been legalized, the effect of decriminalization has had little effect on the consumption rate of cannabis. [5] In 2004, Reinarman et al looked at the consumption of marijuana rates between San Francisco and Amsterdam to see what effect decriminalization had on these different populations. [6] The results showed that the consumption habits between the two populations were negligible. Little evidence has shown that the decriminalization of cannabis has changed the consumption habits of the populations involved. [7]
While there is a rich history of anecdotal accounts of the benefits of marijuana and a long tradition of marijuana being used for a variety of ailments, the scientific literature in support of medicinal uses of marijuana is less substantial. Considered one of the first scientifically valid papers in support of marijuana’s medicinal benefit, in 2007, Dr. Donald Abrams and colleagues published the results of a randomized placebo-controlled trial examining the effect of smoked cannabis on the neuropathic pain of HIV-associated sensory neuropathy and an experimental pain model. The authors concluded that smoked cannabis effectively relieved chronic neuropathic pain in HIV-associated sensory neuropathy and was well tolerated by patients. The pain relief was comparable to chronic neuropathic pain treated with oral drugs. [8]
According to Harvard Medical School's April, 2010 edition of the Harvard Mental Health Letter [9] : Consensus exists that marijuana may be helpful in treating certain carefully defined medical conditions. In its comprehensive 1999 review, for example, the Institute of Medicine (IOM) concluded that marijuana may be modestly effective for pain relief (particularly nerve pain), appetite stimulation for people with AIDS wasting syndrome, and control of chemotherapy-related nausea and vomiting.
These widely held beliefs in the medical community supporting the medicinal benefit of marijuana are starting to gain support in the form of rigorous empirical evidence demonstrating its clinical benefit and limited potential for harm. In 2012, the AMA published a landmark study that followed more than 5,000 patients longitudinally over 20 years. The results of the study were somewhat surprising. Although many had assumed that regular exposure to marijuana smoke would result in pulmonary function damage, similar to the deleterious effects seen with regular tobacco smoke exposure, the study convincingly demonstrated that regular exposure to marijuana smoke did not adversely affect lung function. Even more surprising, regular marijuana smokers demonstrated increased total lung function capacity.
The authors report, “Marijuana may have beneficial effects on pain control, appetite, mood, and management of other chronic symptoms. Our findings suggest that occasional use of marijuana for these or other purposes may not be associated with adverse consequences on pulmonary function.” [10]
The AMA is urging the federal government to change the classification of marijuana from a Schedule I drug to enable further clinical research on marijuana. Additionally, Harvard Mental Health Letter's authors point out that while marijuana works to relieve pain, suppress nausea, reduce anxiety, improve mood, and act as a sedative, the evidence that marijuana may be an effective treatment for psychiatric indications is inconclusive. [11]
In a systematic review published as a “Report of the Guideline Development Subcommittee of the American Academy of Neurology”, the authors performed a systematic review of medical marijuana from 1948 to November 2013 to identify the role of medical marijuana in the treatment of multiple sclerosis (MS), epilepsy and, movement disorders. The authors concluded that medical marijuana was found to be effective for treating MS-related pain or painful spasms. [11]
While marijuana may have medicinal benefits, its use in excess by some individuals can lead to marked impairment in social and occupational functioning. Published in 2013, the fifth edition of TheDiagnostic and Statistical Manual of Mental Disorders (DSM-5) included significant changes to substance-related and addictive disorders. DSM-5 combined the previously separate categories of substance abuse and dependence into a single disorder of substance use, specific to the substance (eg, Alcohol Use Disorder, Cannabis Use Disorder). The Text Revision of the DSM-5 was published in 2022. It recognizes the following 5 cannabis-associated disorders: [12]
-
Cannabis Use Disorder
-
Cannabis Intoxication
-
Cannabis Withdrawal
-
Cannabis-Induced Mental Disorders
-
Unspecified Cannabis-Related Disorder
An example of Cannabis sativa is shown in the image below.
Case study
Mr. X, a 19-year-old single white male presents complaining of apathy, lack of motivation, and an increasing sense of social isolation. He tried marijuana for the first time at age 15, when he was a junior in high school, and quickly started smoking on a daily basis. He would spend nights and then days with friends, getting "stoned," experiencing the "giggles" and relishing the inevitable "munchies." He quickly noticed that smoking marijuana seemed to quell feelings of anxiety he experienced in social settings. Having graduated from high school a year earlier, he describes unfulfilled plans to attend college, which were foiled by his inability to submit the requisite applications. He describes half-hearted attempts to secure employment and now resides in the basement of his parent's house, supported by them. He describes a typical day in the following fashion:
Upon waking, usually in the late morning, he invariably takes a bong hit or smokes a joint, to "get going." Then he spends a significant amount of time preparing breakfast—he feels the marijuana heightens his culinary senses and he takes great joy in cooking and preparing a large meal.
Following breakfast, he retires back to his room in the basement and spends the next several hours playing video games online. When he senses that he is slowing down and feeling sleepy, he will smoke more marijuana because it gives him more energy and improves his mood.
He will typically break from his immersion in the online gaming world for a late lunch, repeating his earlier efforts associated with breakfast. Occasionally, he will go to the local park to play basketball with the kids that are still in high school. Previously a successful athlete in high school, he feels like he has lost a step and his reflexes on the court are not as quick as they used to be.
He has taken to selling a baseball card collection he painstakingly acquired when he was younger to raise money to pay for his marijuana, and, as that collection has dwindled, he has started to grow marijuana in his basement. He describes his first efforts as generating a meager plant that bears a resemblance to the sad Christmas tree from Charlie Brown.
He does not understand why he no longer has a girlfriend or why it has become difficult to meet new girls. He seems perplexed by his last girlfriend's complaints that he had become boring and it seemed like he was "letting life pass him by." He reports that his parents seem to be growing increasingly frustrated with him and reports arguing with them over his marijuana use—they identify it as a problem, he disagrees. He no longer goes out at night and instead spends most of his time smoking and playing video games alone in his room in the basement.
He denies any difficulty sleeping, although he does not remember dreaming anymore and cannot remember the last dream he had. He reports some cognitive difficulties associated with decreased ability to concentrate and some short-term memory problems. He reports feeling occasionally irritable when too much time passes in between smoking and feels that marijuana makes him less irritable. He is interested in being more social, more engaged, and feeling like he is achieving his goals but seems unable to explain why he cannot accomplish what he sets out to do.
He does not seem to appreciate that his heavy and chronic marijuana use is a significant cause of his symptoms. He indicates that overall he enjoys smoking marijuana and believes it makes it easier for him to enjoy his days, which have become more difficult lately as he appreciates the stark difference between the quality of life he is enjoying compared with his peers who are now working or attending college.
Pathophysiology
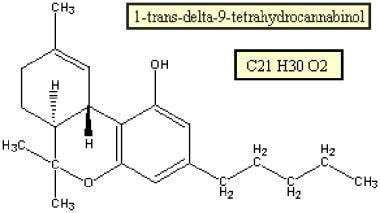
The term cannabinoid refers to compounds that can activate either the cannabinoid receptor 1 (CB1) or CB2 receptor, or both. Additionally 50-60 additional substances have been isolated from cannabis that do not activate the CB1 or CB2 receptors. Delta-9-tetrahydrocannabinol (THC) is recognized as the major psychoactive component of cannabis (see the image below). THC potently activates the G-protein–coupled cannabinoid receptor CB1 and modulates the cannabinoid receptor CB2. [13, 14]
Cannabidiol is considered the most abundant nonpsychoactive cannabinoid in cannabis. It is the constituent thought now to reduce many of the undesirable effects of THC; it significantly reduces the anxiety and psychoticlike symptoms that can be associated with THC. It is currently under investigation for use as an anxiolytic and antipsychotic. Double-blinded tests on volunteers have demonstrated its usefulness as an anxiolytic in anxiogenic test situations. Animal and human studies also suggest that it has a pharmacologic profile similar to atypical antipsychotics; as such, cannabis is being considered as an alternative effective treatment for schizophrenia. [15] However, THC has been more extensively studied; therefore, much of our understanding of the physiological changes induced by marijuana is predicated on the binding and metabolism of THC.
Smoking is the most common and efficient means of ingestion, with the dose being titrated by the user through varying the depth and frequency of inhalation; thus, the delivery mechanism poses a challenge for cannabis as a medication. THC can also be extracted by fat-containing foods or dissolved in oil for pharmaceutical purposes.
Synthetic cannabinoids exist that are more potent and somewhat more water soluble. Currently, the following 2 medications containing synthetic THC are US Food and Drug Administration (FDA) approved:
-
Dronabinol (Marinol): This drug is indicated for anorexia associated with weight loss in patients with AIDS and nausea and vomiting associated with cancer chemotherapy in patients who have not responded adequately to conventional antiemetic treatments.
-
Nabilone (Cesamet): This drug is indicated for nausea and vomiting associated with cancer chemotherapy in patients who have not responded adequately to conventional antiemetic treatments.
After intake, THC undergoes metabolism to an inactive metabolite (8-11-DiOH-THC) and to a highly active metabolite (11-OH-delta-9-THC). The half-life of THC is approximately 4 hours. The long life of the active metabolite is explained by the incorporation of the compound in lipid storage depots and similar storage sites in muscle tissue. Thirty to 60% of THC, in all forms, is excreted in feces; the remaining amount is excreted in urine.
The endocannabinoid system is now understood to be a complex lipid–signaling network in which different proteins play specific roles in controlling or modulating a variety of physiological and pathophysiological processes. [14] Delta-9-THC is believed to exert all of its effects on the brain via the CB1 receptor. High densities of CB1 receptors are found in the cerebral cortex (especially frontal), basal ganglia, cerebellum, anterior cingulate cortex, and hippocampus. They are relatively absent in the brainstem nuclei. Stimulation of these receptors causes monoamine and amino acid neurotransmitters to be released. Endogenous ligands for CB1 receptors include anandamide and 2-arachidonylglycerol—the endocannabinoids.
Epidemiology
Frequency
Marijuana remains the most commonly used illicit drug. In 2020, 17.9% of people aged 12 years or older (49.6 million people) used marijuana in the past year. [16]
According to the 2021 Monitoring the Future survey, the percentage of students who reported using marijuana (in all forms, including smoking and vaping) within the past year decreased significantly for 8th, 10th, and 12th grade students. [17]
-
8th graders: 7.1% reported using marijuana in the past year in 2021, compared to 11.4% in 2020
-
10th graders: 17.3% reported using marijuana in the past year in 2021, compared to 28.0% in 2020
-
12th graders: 30.5% reported using marijuana in the past year in 2021, compared to 35.2% in 2020
Throughout their lifetime, approximately 9% of the American adult population has met criteria for a cannabis use disorder. [18]
An estimated 80.5 million European adults have used marijuana at least once and it is widely accepted that it is the most frequently used illicit substance in Western countries. [19]
Mortality/Morbidity
Cannabis consumption has never directly resulted in mortality, and no fatalities have been documented that identify cannabis consumption as the etiologic agent. However, cannabis consumption has been associated with multifactorial deaths, including marijuana-related accidents and deaths attributed to abuse of alcohol and other illicit substances. [20]
Studies using simulated driving and flying situations have shown that the use of cannabis has a profound effect on estimations of time and distance and causes impairment of attention and short-term memory. These effects are still discernible 24-48 hours after use of the drug. A linear relationship is noted between level of impairment and serum/saliva THC level in tasks necessary for driving, such as perceptual motor control, motor impulsivity, and cognitive function. A double-blind, placebo-controlled, randomized study showed that therapeutic doses of medicinal THC (dronabinol) impairs driving ability in healthy adults to the same extent as alcohol at blood levels of 0.5–1 mg/mL, suggesting that driving is impaired with even small doses of psychoactive cannabinoids. [21]
Cannabis dependence is associated with morbidity, including impaired occupational and social functioning. Cannabis use can be comorbid with the presence of other psychiatric disorders, characterized by a disordered thought process, perceptual disturbances, or symptoms of anxiety. When marijuana is believed to be the etiologic agent, clinicians may diagnose a cannabis-induced disorder.
Psychotic symptoms represent a significant morbidity associated with cannabis use in select patients. While cannabis and the development of psychosis have been linked, this link is not without considerable controversy and there are differing perspectives on whether this relationship is indeed causal, temporal, or coincidental. Given marijuana's clinical benefits, some have argued that patients diagnosed with psychotic disorders gravitate toward self-medicating with marijuana for these effects, while others have advanced the view that marijuana can help precipitate the onset of psychosis in those who are genetically vulnerable. A study examining this controversial topic concluded that marijuana use can play a "catalytic role" in the onset of psychosis as demonstrated by cannabis use being associated with an association of an earlier age at on onset of psychosis treatment. Unfortunately, this study is not without limitations. [22]
Another article examining this topic observed patients over 10 years and reached some similar conclusions. This study appears to provide additional evidence supporting the hypothesis that cannabis use is associated with an earlier age of onset of psychosis. However, the authors' findings complicate the debate further regarding the potential role of cannabis as an etiologic agent versus its use as self-medication by patients with psychotic symptoms. The authors note that there is a bidirectional relationship between psychosis and cannabis use; cannabis exposure predicted psychosis severity and those with more severe psychotic symptoms were more likely to use cannabis in the future. [23]
A study conducted in Germany stated that the use of cannabis in adolescence is a risk factor for the development of incident psychotic symptoms. [24] This study was not without significant limitations; the study ignored the impact of genetic inheritability as a risk factor in the development of psychosis, the impact of confounding risk factors associated with other drug use (eg, PCP, methamphetamine), and the authors’ assumption that transient psychotic experiences were a surrogate for clinically relevant psychosis.
A meta-analysis examining 83 different studies reached similar conclusions, reporting that cannabis use was associated with an earlier age of onset of psychosis. Unfortunately despite a dearth of evidence, the authors argued that this temporal association supported their personal view that marijuana was an etiological risk factor for the development of psychosis. [25] The exact role marijuana plays in the development of psychosis and whether or not it has any causal role remains a matter of debate and controversy.
Marijuana abuse may be a factor in vehicle or machinery accidents because intoxication affects coordination and motor performance. Perform the appropriate tests for use of marijuana after these accidents.
Demographics
Given how widespread cannabis use is globally, across cultures, race is not a significant risk factor associated with cannabis use nor does it represent a useful criterion for identifying acute or chronic marijuana users. However, a study in California demonstrated a significant disparity in arrest rates for users of marijuana based on race. According to the report, from 2004–2008, in Sacramento and San Francisco Counties, Black residents were arrested for marijuana possession 4 times as often as White residents. In Los Angeles County, the disparity was more than 3 to 1. [26]
A report looking at factors that could predict transition from abuse to dependence provided additional epidemiological data. According to the authors, rates of cannabis use were higher among White males. [27]
Similarly to other addictive drugs, fewer females than males use marijuana. [16]
Use, abuse, and dependence on marijuana tends to cut across demographics, including age.
Risk factors among adolescents that may increase the likelihood for marijuana abuse include the presence of comorbid substance use and environmental stressors, including difficulty in school.
Pregnancy
A multicenter cohort found maternal cannabis use evaluated by biological sampling was associated with adverse pregnancy outcomes related to placental dysfunction. Among 9257 participants whose urine was analyzed, 610 individuals showed cannabis use during pregnancy. Of these individuals, 32.4% had cannabis exposure only during the first trimester and 67.6% had ongoing exposure beyond the first trimester. Primary composite outcome included small-for-gestational-age birth, medically indicated preterm birth, stillbirth, or hypertensive disorders of pregnancy. Cannabis use during the first trimester only was not associated with the primary composite outcome; however, ongoing cannabis use was associated with the primary composite outcome (adjusted relative risk, 1.32 [95% CI, 1.09-1.60]). [28]
Patient Education
See the list below:
-
American Council for Drug Education, Basic Facts About Drugs: Marijuana
-
National Institute on Drug Abuse, Infofacts, Marijuana
-
National Institute on Drug Abuse, Marijuana: Facts for Teens
-
Office of National Drug Control Policy, Marijuana
-
eMedicineHealth, Substance Abuse Center
-
eMedicineHealth, Drug Dependence and Abuse and Substance Abuse
-
National Institute on Drug Abuse, Parents and Teachers
-
Cannabis sativa.
-
The major psychoactive component of marijuana is tetrahydrocannabinol (THC).