Background
Atrioventricular (AV) dissociation is a condition whereby the atria and the ventricles activate independently of each other. The normal activation—sinus node followed by the atria, AV node, and then the His-Purkinje system causing ventricular activation—is no longer observed. AV dissociation may occur when a subsidiary pacemaker in the AV node or the ventricle overtakes the sinus node for impulse initiation due to slowing of the sinus node, or it may occur when a subsidiary site (ie, the ventricle) beats faster than the sinus node, such as in ventricular tachycardia. The causes of AV dissociation are important to understand as they impact the treatment plan.
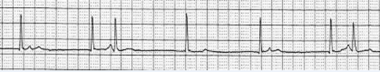
The escape of a subsidiary (latent) pacemaker in cardiac tissue may occur if the dominant pacemaker (the sinus node) slows considerably. A subsidiary pacemaker in the AV junction or below may activate at a faster rate compared to the sinus node and thereby cause AV dissociation without retrograde atrial capture. [1, 2, 3] For example, sinus bradycardia, with a very slow sinus rate, may allow the AV junction to become a subsidiary pacemaker and thus activate independently from the sinus node (see the image below). AV dissociation does not imply AV block, but both AV block and AV dissociation can occur concurrently. [4]
 Atrioventricular Dissociation. Significant slowing of the sinus node allows for a subsidiary pacemaker (atrioventricular [AV] junction) to activate, causing AV dissociation.
Atrioventricular Dissociation. Significant slowing of the sinus node allows for a subsidiary pacemaker (atrioventricular [AV] junction) to activate, causing AV dissociation.
In general, AV block is associated with a faster atrial rate than ventricular rate. The P waves, representing atrial conduction, cannot activate the ventricles in complete heart block. In AV dissociation, a block is not necessarily present. If a P wave is properly timed, it may conduct to the ventricle in AV dissociation; this is termed a capture beat. Heart block, which may occur with AV dissociation, is discussed in detail in the Medscape Drugs & Diseases article Atrioventricular Block.
The prevalence of AV dissociation is unknown. No racial preponderance or age predilection exists, and men and women are equally affected.
Types of AV dissociation
There are two types of AV dissociation, complete and incomplete.
Complete AV dissociation
Complete AV dissociation occurs when the atria and the ventricles activate independently from one another and the atrial rate is slower or equal to the ventricular rate. The fact that none of the P waves conduct has more to do with the timing of the P waves in relation to the QRS complex rather than the presence of AV block. [5]
Incomplete AV dissociation
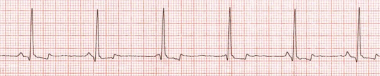
Incomplete AV dissociation occurs when there is either intermittent atrial capture from the ventricles or intermittent ventricular capture from the atria. During incomplete AV dissociation, some of the P waves conduct and capture the ventricles (ie, interference AV dissociation, see the image below).
Interference AV dissociation occurs when a well-timed P wave conducts via a nonrefractory AV conduction system. Interference AV dissociation is initiated by slowing of the sinus node due to sinus bradycardia or sinus arrest, thereby allowing an independent subsidiary pacemaker in the junction (narrow QRS complex) or the ventricle (wide QRS complex) to take over ventricular activation. [6]
 Atrioventricular Dissociation. This rhythm strip reveals interference atrioventricular dissociation, as there is a P wave conducting to the ventricle in the third and seventh beats, whereas the P wave fails to conduct to the ventricle in the other beats.
Atrioventricular Dissociation. This rhythm strip reveals interference atrioventricular dissociation, as there is a P wave conducting to the ventricle in the third and seventh beats, whereas the P wave fails to conduct to the ventricle in the other beats.
In contrast, during isorhythmic AV dissociation, a synchronized dissociation occurs when the atrial and ventricular rates are similar, demonstrating an apparent association of the two cardiac chambers. [7] Either slowing of the sinus node discharge rate or the emergence of a slightly faster subsidiary pacemaker controlling the ventricles is the common initiating event. Junctional rhythms may show isorhythmic AV dissociation as the P waves and QRS complexes appear to have a close relationship to one another; however, they are actually activating independently from one another. With close observation of the rhythm strip, the P wave may be either just prior, inscribed within, or seen in the terminal portion of the QRS complex (see the image below).;
 Atrioventricular Dissociation. Isorhythmic AV dissociation. There is AV dissociation with independent atrial and ventricular conduction at similar rates.
Atrioventricular Dissociation. Isorhythmic AV dissociation. There is AV dissociation with independent atrial and ventricular conduction at similar rates.
Ventricular tachycardia may occur without retrograde atrial activation (due to complete retrograde block) causing AV dissociation, because the atria and ventricles beat independently and the atrial rate is slower than the ventricular rate. An accelerated junctional rhythm with a slower sinus node rate may also be associated with AV dissociation and retrograde block.
Pathophysiology
The cause of atrioventricular (AV) dissociation is due to an increased rate of a subsidiary (escape) pacemaker and/or a decreased rate of the sinus node. The use of certain medications including beta-blockers, digitalis, and calcium channel blockers may lead to slowing of the sinus node and cause a subsidiary pacemaker to activate in the ventricle or AV junction. [8] Vagal activation (eg, neurocardiogenic syncope, vomiting) may cause this as well. AV dissociation can also be seen after radiofrequency ablation of the slow pathway responsible for AV nodal reentry tachycardia, leading to acceleration of an AV junctional activation that is faster than the sinus node activation. After exertion, if AV dissociation is present from an escape pacemaker, it can be a normal phenomenon.
Accelerated activation of the subsidiary pacemaker can occur during surgical and anesthesia interventions (including intubation), conditions that increase catecholamine levels (including vasoconstrictor infusions of inotropes), myocardial infarction, structural heart disease, hyperkalemia, ventricular tachycardia, or ventricular pacing.
Etiology
Major causes of atrioventricular (AV) dissociation include high vagal tone, sinus bradycardia, ventricular tachycardia, nonparoxysmal junctional tachycardia, junctional escape rhythm, and an accelerated idioventricular rhythm. [9, 10, 11, 12, 13]
In nonparoxysmal junctional tachycardia, junctional rhythm/tachycardia occurs at a rate faster than the sinus rate, without retrograde atrial capture. This is observed in clinical situations such as digoxin toxicity, sinus bradycardia with escape junctional rhythm, and after cardiac surgery, particularly aortic valve surgery or replacement due to its close anatomic approximation to the AV node and His-Purkinje system. [14]
Long postectopic cycles allow an escape junctional rhythm as well. A normal sinus beat followed by a premature ventricular beat resets the sinus node timing cycle. Occasionally, especially in sinus node disease, the sinus impulse takes longer to activate than usual and a junctional escape beat or rhythm may follow, and this may lead to AV dissociation as the sinus node activates much slower than the junctional escape rhythm.
Prognosis
The prognosis is generally good, but it may depend on the severity of the underlying problem causing the AV dissociation. Although benign, it may indicate serious underlying cardiovascular issues (eg, ischemia, digoxin toxicity). For conditions in which AV dissociation may be iatrogenic (ie, high doses of beta-blockers, calcium channel blockers, or digitalis in the setting of renal failure), the prognosis is excellent, as removal of the cause eliminates the problem. Occasionally, AV dissociation can affect hemodynamics and cause a reduction in cardiac output or blood pressure, but once treated the prognosis is excellent.
Morbidity/mortality
AV dissociation is generally benign. Any adverse effects are related to the ensuing bradycardia, AV dyssynchrony, or underlying conditions.
Complications
Complications of AV dissociation are generally due to hemodynamic compromise due to the processes that cause AV dissociation (eg, ventricular tachycardia, severe sinus bradycardia). The low blood pressure and very fast or very slow heart rate may lead to traumatic syncope. Hypoperfusion of end organs due to brady or tachyarrhythmias is possible. Acute renal failure from a reduction in renal blood flow due to a low cardiac output is commonly seen in severe bradycardia and AV dissociation. Ischemia or myocardial infarction could occur in cases in which the tachyarrhythmia or bradyarrhythmia coupled with AV dissociation may lead to reduced coronary artery perfusion. These clinical situations may require immediate resuscitative efforts to establish both normal a blood pressure and heart rate to allow adequate end-organ perfusion.
Patient Education
AV dissociation should be discussed with a patient who is symptomatic to identify the underlying cause(s) and discuss methods to prevent the problem. Patients with marked sinus bradycardia and AV dissociation may need a pacemaker. Patients with a history of AV dissociation requiring treatment or withdrawal of an offending drug (ie, medication induced) must be informed of the condition that led to AV dissociation (ie, digitalis use in renal failure or high dose beta blocker use to treat hypertension), be aware of the consequences if no changes in medications are made (recurrent dizziness, syncope, trauma) and must inform their health care providers to avoid such medications to prevent it from recurring. Patients must also be counselled on the effects of deleterious drug-drug interactions (ie, taking clonidine for hypertension and a concomitant beta blocker for atrial fibrillation) to avoid initiation of AV dissociation.
-
Atrioventricular Dissociation. Significant slowing of the sinus node allows for a subsidiary pacemaker (atrioventricular [AV] junction) to activate, causing AV dissociation.
-
Atrioventricular Dissociation. This rhythm strip reveals interference atrioventricular dissociation, as there is a P wave conducting to the ventricle in the third and seventh beats, whereas the P wave fails to conduct to the ventricle in the other beats.
-
Atrioventricular Dissociation. Isorhythmic AV dissociation. There is AV dissociation with independent atrial and ventricular conduction at similar rates.







