Practice Essentials
Esthesioneuroblastoma (ENB), also known as olfactory neuroblastoma, is a rare neoplasm originating from olfactory neuroepithelium. Due to the rare and complex nature of ENB, multiple opinions exist regarding the etiology, optimal staging system, and treatment modalities. These tumors often display varying biologic activity ranging from indolent growth, with patient survival exceeding 20 years, to a highly aggressive neoplasm capable of rapid widespread metastasis, with survival limited to a few months.
When metastasis occurs, cervical lymph nodes are the most frequent site. Less commonly, metastasis to the lungs and bone has been reported. [1]
Images of esthesioneuroblastomas are shown below.
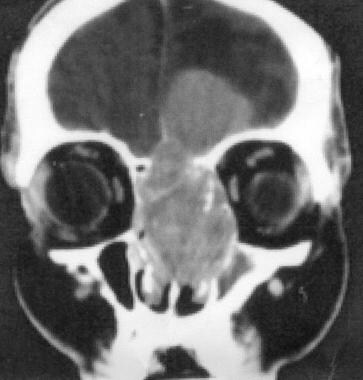 Esthesioneuroblastoma. Coronal CT scan of the orbits and sinuses shows a large, enhancing, and expansile mass occupying the ethmoid air cells that is invading the cribriform plate and breaking through to the left anterior cranial fossa. Image courtesy of Michael Lev, MD.
Esthesioneuroblastoma. Coronal CT scan of the orbits and sinuses shows a large, enhancing, and expansile mass occupying the ethmoid air cells that is invading the cribriform plate and breaking through to the left anterior cranial fossa. Image courtesy of Michael Lev, MD.
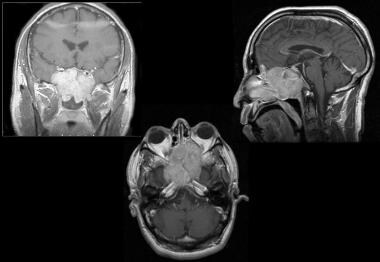 Esthesioneuroblastoma. A 39-year-old man presented with 1 month of decreased vision, left facial numbness, and swelling. Physical examination demonstrated left-sided exophthalmos and blindness. He had also lost his sense of smell. Contrast-enhanced T1-weighted MRI demonstrated a large lesion that originated in the paranasal sinuses and extended through the cribriform plate into the anterior cranial fossa. He underwent a bifrontal craniotomy for resection of this tumor.
Esthesioneuroblastoma. A 39-year-old man presented with 1 month of decreased vision, left facial numbness, and swelling. Physical examination demonstrated left-sided exophthalmos and blindness. He had also lost his sense of smell. Contrast-enhanced T1-weighted MRI demonstrated a large lesion that originated in the paranasal sinuses and extended through the cribriform plate into the anterior cranial fossa. He underwent a bifrontal craniotomy for resection of this tumor.
The prognosis depends on the magnitude of the disease on initial diagnosis. It should be noted that precise histologic diagnosis is difficult because ENBs are often confused with other small round-cell neoplasms of the nasal cavity. Despite the difficulties associated with the treatment of ENB, evolving treatment modalities, including surgery, radiation, and adjuvant chemotherapy, have contributed to better management of ENB and longer survival of these patients. [2] See Treatment and Medication.
Pathophysiology
Esthesioneuroblastomas (ENBs) are undifferentiated tumors of neuroectodermal origin derived from the olfactory epithelium. [3] The tumor cells are mitotically active and are the precursor cells that develop into sustentacular and neuronal cells. Inconsistent histologic presentations initially led to controversy surrounding the exact histologic origin of ENBs, and this ambiguity can confound clinical and prognostic decisions. In essence, ENBs contain variable arrangements of their small cells. Additionally, there exists a variable presence (or absence) of true rosettes and neurofibrillary material.
To date, no certain genetic factor has been identified that can accurately assist in the diagnosis or predict prognosis. This is partially due to the ability to analyze cancer genomes on a whole genome basis. Analysis of ENBs with array comparative genomic hybridization revealed complex gene copy number profiles, which varied by tumor stage. [4] Of the many alterations were identified in this study, chromosomal gains in 7q11 and 20q and deletions in 2q, 5q, 6p, 6q, and 18q have been confirmed by at least 2 other studies. Interestingly, 20q is a region that has been implicated in other cancers, including breast, ovarian, and squamous cell carcinoma. Still, further experimentation will be required to determine the role of these genomic regions in ENB.
Etiology
No clear etiologic agent or exposure has been documented in humans; however, a single case of occupational exposure has been reported in a woodworker. [5] Esthesioneuroblastoma (ENB) can be consistently induced by nitrosamine compounds in rodents. In cats with spontaneous ENB or in transgenic mice developing ENB, type C retroviral particles have been demonstrated and classified as feline and murine leukemia virus, respectively. The role of retrovirus sequences in human ENB remains to be evaluated.
Epidemiology
Frequency
Interestingly, 80% of the esthesioneuroblastoma (ENB) cases published in the literature since Berger and Luc described the first case in 1924 have been identified in the last few decades. [6] However, the current data set cannot distinguish between a rising incidence and better recognition of the disease.
ENB has an estimated incidence of 4 cases per 10 million individuals and accounts for approximately 5% of all sinonasal tumors. A search of the National Cancer Database by Carey et al identified 1225 cases of ENB. [7] Similar incidence rates have been obtained through epidemiologic studies performed in Denmark. [8] No studies suggest a geographic variation in rates.
Race-, sex-, and age-related demographics
ENB does not show a predilection toward any individual race. ENB does not show familial prevalence and has been reported in all races and on all continents. ENB affects males and females with similar frequency.
ENB occurs in a wide range of age groups (3-90 y). It has a bimodal peak of occurrence in the third and sixth decades of life.
Prognosis
Treatment results before the availability and use of modern diagnostic techniques were flawed, probably by the inclusion of cases of sinonasal undifferentiated carcinoma and sinonasal neuroendocrine carcinoma, which are aggressive diseases associated with poor survival. The importance of correctly differentiating these cancers is highlighted in a report by Rosenthal et al. [9] For a discussion of posttreatment prognosis, see Kane et al. [10]
The 5-year patient survival rates have varied from 50-80%, with the majority of large studies indicating survival rates of higher than 70%. In the 2001 meta-analysis by Dulguerov et al, the average 5-year survival was 45% ± 22% (range,e carcinoma, which are aggressive diseases associated with poor survival. The importance of correctly differentiating these cancers is highlighted in a report by Rosenthal et al. [9] For a discussion of posttreatment prognosis, see Kane et al. [10]
The 5-year patient survival rates have varied from 50-80%, with the majority of large studies indicating survival rates of higher than 70%. In the 2001 meta-analysis by Dulguerov et al, the average 5-year survival was 45 ± 22% (range, 0-86%). [11] A retrospective of long-term outcomes in 139 patients treated at MD Anderson Cancer Center reported 5-year overall survival of 85.6% and disease-specific survival of 93.4%. The recurrence rate was 6.4% in patients receiving nodal radiation therapy, compared with 34.4% in patients who did not undergo radiation treatment. [12]
Whether the Kadish classification system has a definitive prognostic value remains unknown, but the available survival data for Kadish stages A, B, and C are 72%, 59%, and 47%, respectively. According to the Dulguerov staging system, the survival rates were 81% for T1, 93% for T2, 59% for T3, and 48% for T4.
Prognostic survival factors that emerged in the meta-analysis by Dulguerov et al include lower Hyams histopathologic grade (5-year survival of 56% for grades I-II vs 25% for grades III-IV) and absence of neck lymph node metastasis (64% for N0 vs. 29% for N+). [11] Other possible but unconfirmed prognostic factors include a low proliferative index, the completeness of the surgical resection, and tumor shrinkage after induction chemotherapy.
Survival data categorized according to treatment modality favored regimens that include surgery.
The most frequent recurrence is local, with rates from 20-40% (29% in the Dulguerov et al meta-analysis). Craniofacial resection followed by radiation seems to result in fewer recurrences, a rate of approximately 10%. Salvage after local recurrence is possible in one third to one half of cases. Regional recurrence, while disease at the primary site remains under control, occurs in 15% of cases and is salvageable by further treatment in 25-50% of cases. Distant metastasis with locoregional control occurs infrequently (8%) and carries a dismal prognosis.
-
Esthesioneuroblastoma. Coronal CT scan of the orbits and sinuses shows a large, enhancing, and expansile mass occupying the ethmoid air cells that is invading the cribriform plate and breaking through to the left anterior cranial fossa. Image courtesy of Michael Lev, MD.
-
Esthesioneuroblastoma. A 39-year-old man presented with 1 month of decreased vision, left facial numbness, and swelling. Physical examination demonstrated left-sided exophthalmos and blindness. He had also lost his sense of smell. Contrast-enhanced T1-weighted MRI demonstrated a large lesion that originated in the paranasal sinuses and extended through the cribriform plate into the anterior cranial fossa. He underwent a bifrontal craniotomy for resection of this tumor.







