Practice Essentials
An adrenal crisis , a potentially life-threatening disorder, arises from an acute deficiency of the adrenal hormone cortisol, a glucocorticoid. Adrenal crisis should not be confused with chronic, stable adrenal insufficiency, such as Addison disease (primary adrenal insufficiency). [1]
In 1855, Thomas Addison described a syndrome of long-term adrenal insufficiency that develops over months to years, with weakness, fatigue, anorexia, weight loss, and hyperpigmentation as the primary symptoms. In contrast, an acute adrenal crisis can manifest with vomiting, abdominal pain, and hypovolemic shock. [2, 3] When not promptly recognized, adrenal hemorrhage can be a cause of adrenal crisis. Administration of glucocorticoids in supraphysiologic or stress doses is the only definitive therapy for adrenal crisis. [4, 5, 6, 1] See the images below.
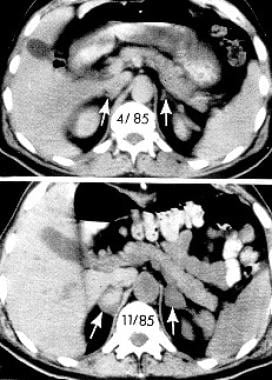 Computed tomographic (CT) scans of the abdomen show normal adrenal glands several months before the onset of hemorrhage (upper panel) and enlarged adrenals 2 weeks after an acute episode of bilateral adrenal hemorrhage (lower panel). The attenuation of the adrenal glands, indicated by arrows, is increased after the acute event. Reproduced from Rao RH, Vagnucci AH, Amico JA: Bilateral massive adrenal hemorrhage: early recognition and treatment. Ann Intern Med. Feb 1 1989;110(3):227-35 with permission from the journal.
Computed tomographic (CT) scans of the abdomen show normal adrenal glands several months before the onset of hemorrhage (upper panel) and enlarged adrenals 2 weeks after an acute episode of bilateral adrenal hemorrhage (lower panel). The attenuation of the adrenal glands, indicated by arrows, is increased after the acute event. Reproduced from Rao RH, Vagnucci AH, Amico JA: Bilateral massive adrenal hemorrhage: early recognition and treatment. Ann Intern Med. Feb 1 1989;110(3):227-35 with permission from the journal.
Workup in adrenal crisis
Serum chemistry abnormalities are present in as many as 56% of patients. Hyponatremia is common (although not diagnostic); hyperkalemia, metabolic acidosis, and hypoglycemia also may be present. However, the absence of laboratory abnormalities does not exclude the diagnosis of adrenal crisis.
Chest radiography can be used to assess for tuberculosis, histoplasmosis, malignant disease, sarcoid, and lymphoma. Abdominal computed tomography (CT) scanning is used to visualize the adrenal glands for hemorrhage, atrophy, infiltrative disorders, and metastatic disease. Adrenal hemorrhage appears as hyperdense, bilaterally enlarged adrenal glands.
In primary adrenocortical failure, histologic evidence of infection, infiltrative disease, or another condition may be demonstrated. Secondary adrenocortical insufficiency may cause atrophy of the adrenals or no histologic evidence at all.
Management of adrenal crisis
Administration of glucocorticoids in supraphysiologic or stress doses is the only definitive therapy. [4, 5] Dexamethasone does not interfere with serum cortisol assay and, thus, may be the initial drug of choice. However, because dexamethasone has little mineralocorticoid activity, fluid and electrolyte replacement are essential.
A thorough search for a precipitating cause of adrenal crisis and administration of empiric antibiotics are indicated. Reversal of coagulopathy should be attempted with fresh frozen plasma. Pressors (eg, dopamine, norepinephrine) may be necessary to combat hypotension.
Pathophysiology
The adrenal cortex produces 3 steroid hormones: glucocorticoids (cortisol), mineralocorticoids (aldosterone, 11-deoxycorticosterone), and androgens (dehydroepiandrosterone). The androgens are relatively unimportant in adults, and 11-deoxycorticosterone is a fairly weak mineralocorticoid in comparison with aldosterone. The primary hormone of importance in acute adrenal crisis is cortisol; adrenal aldosterone production is relatively minor.
Cortisol enhances gluconeogenesis and provides substrate through proteolysis, protein synthesis inhibition, fatty acid mobilization, and enhanced hepatic amino acid uptake. Cortisol indirectly induces insulin secretion to counterbalance hyperglycemia but also decreases insulin sensitivity. Cortisol exercises a significant anti-inflammatory effect by stabilizing lysosomes, reducing leukocytic responses, and blocking cytokine production. Phagocytic activity is preserved, but cell-mediated immunity is diminished, in situations of cortisol deficiency. Finally, cortisol facilitates free-water clearance, enhances appetite, and suppresses adrenocorticotropic hormone (ACTH) synthesis.
Aldosterone is released in response to angiotensin II stimulation via the renin-angiotensin-aldosterone system, hyperkalemia, hyponatremia, and dopamine antagonists. Its effect on its primary target organ, the kidney, is to promote reabsorption of sodium and secretion of potassium and hydrogen. The mechanism of action is unclear; an increase in the sodium- and potassium-activated adenosine triphosphatase (Na+/K+ ATPase) enzyme responsible for sodium transport, as well as increased carbonic anhydrase activity, has been suggested. The net effect is to increase intravascular volume. The renin-angiotensin-aldosterone system is unaffected by exogenous glucocorticoids, and ACTH deficiency has a relatively minor effect on aldosterone levels.
Adrenocortical hormone deficiency results in the reverse of these hormonal effects, producing the clinical findings of adrenal crisis.
Primary adrenocortical insufficiency occurs when the adrenal glands fail to release adequate amounts of these hormones to meet physiologic needs, despite release of ACTH from the pituitary. Infiltrative or autoimmune disorders are the most common cause, but adrenal exhaustion from severe chronic illness also may occur.
Secondary adrenocortical insufficiency occurs when exogenous steroids have suppressed the hypothalamic-pituitary-adrenal (HPA) axis. Too rapid withdrawal of exogenous steroid may precipitate adrenal crisis, or sudden stress may induce cortisol requirements in excess of the adrenal glands' ability to respond immediately. In acute illness, a normal cortisol level may actually reflect adrenal insufficiency because the cortisol level should be quite elevated.
Bilateral massive adrenal hemorrhage (BMAH) occurs under severe physiologic stress (eg, myocardial infarction, septic shock, complicated pregnancy) or with concomitant coagulopathy or thromboembolic disorders.
Hahner et al investigated the frequency and causes of, as well as the risk factors for, adrenal crisis in patients with chronic adrenal insufficiency. Using a disease-specific questionnaire, the authors analyzed data from 444 patients, including 254 with primary adrenal insufficiency and 190 with secondary adrenal insufficiency. At least one adrenal crisis was reported by 42% of patients, including 47% of those with primary adrenal insufficiency and 35% of patients with the secondary condition. GI infection and fever were the most common precipitating causes of crisis. Identified risk factors for adrenal crisis were, for patients with primary adrenal insufficiency, concomitant nonendocrine disease, and for patients with secondary adrenal insufficiency, female sex and diabetes insipidus. [7]
A study from the Netherlands, by Smans et al, of patients with adrenal insufficiency, found the existence of comorbidity to be the most important risk factor for adrenal crisis, with infections being the most common precipitating factors. [8]
A Japanese study, by Iwasaku et al, found that of 504 patients with adrenal crisis, only about one third had preexisting primary or central adrenal insufficiency. In the rest of the patients, comorbidities included cardiovascular disease (31.6%), infection (18.8%), diabetes (16.5%), cancer (19.1%), hypothyroidism (7.0%), autoimmune disease (9.3%), peptic ulcer (6.1%), chronic obstructive pulmonary disease or asthma (6.1%), and renal failure (6.1%). [9]
Epidemiology
Frequency
The incidence of primary adrenocortical insufficiency is variable and depends on the defining cortisol level and the method of testing (ie, ACTH stimulation versus single random cortisol level). The underlying disease also is a factor. Studies of critically ill patients with septic shock demonstrate a de novo (excluding patients with known adrenal insufficiency or patients on glucocorticoid therapy) incidence ranging from 19-54%. Secondary adrenal insufficiency has been demonstrated in 31% of patients admitted to a critical care unit.
Annane et al's landmark 2002 study found a very high rate, ie, 76% of all enrolled patients with septic shock. Of the general perioperative population, in 62,473 anesthetic administrations, only 419 (0.7%) patients required glucocorticoid supplementation and only 3 hypotensive events were thought to be attributable to glucocorticoid deficiency. [10] Studies of patients undergoing cardiac or urologic surgery reveal an incidence of 0.01-0.1%. In a study of 2000 consecutive general hospital autopsies, only 22 (1.1%) revealed bilateral adrenal hemorrhage; however, as many as 15% of patients dying in shock have been demonstrated to have BMAH.
The aforementioned study from the Netherlands, by Smans et al, found the incidence of adrenal crisis among persons with primary adrenal insufficiency to be 5.2 cases per 100 person-years, while in secondary adrenal insufficiency, the incidence was reported as 3.6 cases per 100 person-years. [8]
In a study of Swiss patients with either primary or secondary adrenal insufficiency, Notter et al found the prevalence of adrenal crisis to be 4.4 per 100 disease-years. [11]
According to a report by Chabre et al, the annual incidence of adrenal crisis in Europe is estimated to be 6-8 cases per 100 adrenal insufficiency patients. [12]
A prospective, multicenter study by Hosokawa et al indicated that the rate of adrenal crisis occurring in pediatric adrenal insufficiency is substantial, at 4.27 per 100 person-years. [13]
No description regarding racial data, sexual predilection, or age is available in the literature.
Mortality/Morbidity
In the absence of bilateral adrenal hemorrhage, the survival rate of patients with acute adrenal crisis that is diagnosed promptly and treated appropriately approaches that of patients without acute adrenal crisis with similar severity of illness. Patients who developed BMAH before the availability of hormonal testing or computed tomography (CT) scanning rarely survived. In one series, patients who were diagnosed using CT scanning had an 85% rate of survival. Because the true incidence of adrenal crisis and BMAH are unknown, the actual mortality rate also is unknown.
A Japanese study, by Ono et al, indicated that among patients with adrenal crisis, the risk of death is relatively high in those who are older and have impaired consciousness and diabetes mellitus. In the study, of 799 patients with adrenal crisis and concomitant primary or secondary adrenal insufficiency at hospital admission, 2.4% (19) suffered in-hospital mortality, including 15 who were older than 60 years, 12 who had impaired consciousness at admission, and 13 who received insulin therapy. [14]
-
Computed tomographic (CT) scans of the abdomen show normal adrenal glands several months before the onset of hemorrhage (upper panel) and enlarged adrenals 2 weeks after an acute episode of bilateral adrenal hemorrhage (lower panel). The attenuation of the adrenal glands, indicated by arrows, is increased after the acute event. Reproduced from Rao RH, Vagnucci AH, Amico JA: Bilateral massive adrenal hemorrhage: early recognition and treatment. Ann Intern Med. Feb 1 1989;110(3):227-35 with permission from the journal.
-
Enlarged, dense, suprarenal masses






