Practice Essentials
Breast cancer is the common term for a set of breast tumor subtypes with distinct molecular and cellular origins and clinical behavior. Most of these are epithelial tumors of ductal or lobular origin (see the image below). Worldwide, breast cancer is the most frequently diagnosed life-threatening cancer in women and the leading cause of cancer death among women.
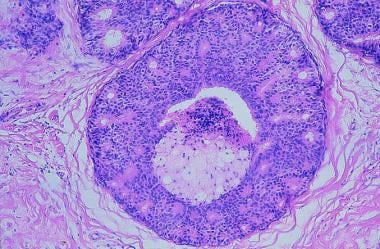 Breast cancer. Intraductal carcinoma, comedo type. Distended duct with intact basement membrane and central tumor necrosis.
Breast cancer. Intraductal carcinoma, comedo type. Distended duct with intact basement membrane and central tumor necrosis.
See Oncology Decision Point for expert commentary on breast cancer treatment decisions and related guidelines. Also see the following Medscape–Memorial Sloan Kettering e-tumor boards:
Signs and symptoms
Early breast cancers may be asymptomatic, and pain and discomfort are typically not present. If a lump is discovered, the following may indicate the possible presence of breast cancer:
-
Change in breast size or shape, even if no lump is palpable [1]
-
Skin dimpling or skin changes
-
Recent nipple inversion or skin change, or nipple abnormalities
-
Single-duct discharge, particularly if blood-stained
-
Axillary lump
See Presentation for more detail.
Diagnosis of breast cancer
Breast cancer is often first detected as an abnormality on a mammogram before it is felt by the patient or health care provider.
Evaluation of breast cancer includes the following:
-
Clinical examination
-
Imaging
-
Needle biopsy
Physical examination
The following physical findings should raise concern:
-
Lump or contour change
-
Skin tethering
-
Nipple inversion
-
Dilated veins
-
Ulceration
-
Eczemalike rash or redness on the nipple or the surrounding area
-
Nipple discharge
-
Edema or peau d’orange
If a palpable lump is found and possesses any of the following features, breast cancer may be present:
-
Hardness
-
Irregularity
-
Focal nodularity
-
Fixation to skin or muscle
Screening
Early detection remains the primary defense in preventing advanced breast cancer. Screening modalities include the following:
-
Mammography with tomosynthesis [2]
-
Ultrasonography
-
Magnetic resonance imaging (MRI) with and without contrast
Ultrasonography and MRI are more sensitive than mammography for invasive cancer in nonfatty breasts. Combined mammography, clinical examination, and MRI are more sensitive than any other individual test or combination of tests.
Breast self-examination is no longer recommended. Instead, breast awareness is recommended; women should be familiar with how their breasts normally look and feel, and report any changes promptly to their health care provider. [2, 3] Most guidelines also recommend against clinical breast examination for screening. [4, 5, 6]
Biopsy
Core biopsy with image guidance is the recommended diagnostic approach for newly diagnosed breast cancers. This obtains breast tissue without surgery and can eliminate the need for additional surgeries. Open excisional biopsy is the surgical removal of the entire lump.
See Workup for more detail.
Management of breast cancer
Surgery, radiation therapy, and adjuvant hormone or chemotherapy when indicated are considered primary treatment. Surgical therapy may consist of lumpectomy or total mastectomy with sentinel lymph node biopsy (SLNB) or complete axillary lymph node dissection (ALND). Radiation therapy may follow surgery in an effort to eradicate residual disease while reducing recurrence rates. Adjuvant systemic therapies (eg, hormonal therapy, chemotherapy, targeted therapies), when indicated, are recommended on the basis of tumor biology, stage, and gene expression assay results, as well as individual patient factors such as comorbidities and personal preferences.
Pharmacologic agents
Pharmacologic treatment for breast cancer is typically selected according to the molecular characteristics of the tumor and the disease stage. Agents used (alone or in combination) include the following [7] :
-
Hormone therapy (eg, tamoxifen, aromatase inhibitors)
-
HER2-targeted therapy (monoclonal antibodies [eg, trastuzumab, pertuzumab]; antibody-drug conjugates [eg, ado-trastuzumab emtansine, trastuzumab deruxtecan); tyrosine kinase inhibitors [eg, tucatinib, neratinib])
-
CDK4/6 inhibitors (eg, palbociclib, ribociclib, abemaciclib)
-
mTOR inhibitors (everolimus)
-
PIK3CA inhibitors (alpelisib)
-
AKT inhibitor (capivasertib)
-
Chemotherapy (eg, cyclophosphamide, doxorubicin, carboplatin, methotrexate)
-
Immunotherapy (pembrolizumab)
In patients receiving adjuvant aromatase inhibitor therapy for breast cancer who are at high risk for fracture, the monoclonal antibody denosumab or either of the bisphosphonates zoledronic acid and pamidronate may be added to the treatment regimen to increase bone mass. These agents are given along with calcium and vitamin D supplementation.
See Treatment and Medication for more detail.
Prevention
Two selective estrogen receptor modulators (SERMs), tamoxifen and raloxifene, are approved for reduction of breast cancer risk in high-risk women. Aromatase Inhibitors are also approved for risk reduction in postmenopausal women. Prophylactic mastectomy is also an option for risk reduction.
Background
Worldwide, breast cancer is the most frequently diagnosed life-threatening cancer in women. In many less-developed countries, it is the leading cause of cancer death in women; in developed countries, however, it has been surpassed by lung cancer as a cause of cancer death in women. [8] In the United States, breast cancer is the most common cancer in women and is second only to lung cancer as a cause of cancer deaths in women. [9] (For discussion of male breast cancer, see Breast Cancer in Men.)
Many early breast cancers are asymptomatic; pain or discomfort is not usually a symptom of breast cancer. Breast cancer is often first detected as an abnormality on a mammogram before it is felt by the patient or healthcare provider.
The general approach to evaluation for breast cancer has become formalized as triple assessment: clinical examination, imaging (usually mammography, ultrasonography, or both), and needle biopsy. (See Workup.) Increased public awareness and improved screening have led to earlier diagnosis, at stages amenable to complete surgical resection and curative therapies. Improvements in therapy and screening have led to improved survival rates for women diagnosed with breast cancer.
Surgery and radiation therapy, along with adjuvant hormone or chemotherapy when indicated, are now considered primary treatment for breast cancer. For many patients with low-risk early-stage breast cancer, surgery with local radiation is curative. (See Treatment.)
Adjuvant breast cancer therapies are designed to treat micrometastatic disease or breast cancer cells that have escaped the breast and regional lymph nodes but have not yet established an identifiable metastasis. Depending on the model of risk reduction, adjuvant therapy has been estimated to be responsible for 35-72% of the decrease in cancer recurrence.
Over the past 3 decades, extensive and advocate-driven breast cancer research has led to extraordinary progress in the understanding of the disease. This has resulted in the development of more targeted and less toxic treatments. (See Treatment and Medication.)
For patient education information, see Breast Cancer and Breast Cancer Diagnosis: Screening, Detection, and Testing.
Anatomy
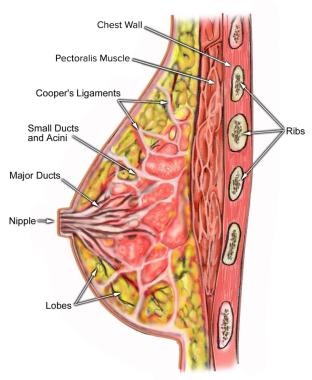
The breasts of an adult woman are milk-producing glands on the front of the chest wall. They rest on the pectoralis major and are supported by and attached to the front of the chest wall on either side of the sternum by ligaments. Each breast contains 15-20 lobes arranged in a circular fashion. The fat that covers the lobes gives the breast its size and shape. Each lobe comprises many lobules, at the end of which are glands that produce milk in response to hormones (see the image below).
Pathophysiology
The current understanding of breast cancer etiopathogenesis is that invasive cancers arise through a series of molecular alterations at the cell level. These alterations result in breast epithelial cells with immortal features and uncontrolled growth.
Genomic profiling has demonstrated the presence of discrete breast tumor subtypes with distinct natural histories and clinical behavior. The exact number of disease subtypes and molecular alterations from which these subtypes arise remains to be fully elucidated, but these generally align with the presence or absence of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2).
This view of breast cancer--not as a set of stochastic molecular events, but as a limited set of separable diseases of distinct molecular and cellular origins--has altered thinking about breast cancer etiology, type-specific risk factors, and prevention and has had a substantial impact on treatment strategies and breast cancer research.
Evidence from The Cancer Genome Atlas Network (TCGA) confirms the following 4 main breast tumor subtypes, with distinct genetic and epigenetic aberrations [10] (see the image below):
-
Luminal A
-
Luminal B
-
Basal-like
-
HER2-positive
It is noteworthy that the basal-like breast tumor subgroup shares a number of molecular characteristics common to serous ovarian tumors, including the types and frequencies of genomic mutations. These data support the evidence that some breast cancers share etiologic factors with ovarian cancer. Most compelling are the data showing that patients with basal-type breast cancers show treatment responsiveness similar to that of ovarian cancers. [11]
The various types of breast cancers are listed below by percentage of cases:
-
Infiltrating ductal carcinoma is the most commonly diagnosed breast tumor and has a tendency to metastasize via lymphatics; it accounts for 75-85% of breast cancers
-
Over the past 25 years, the incidence of lobular carcinoma in situ (LCIS) has doubled, to 3.19 per 100,000 persons/year; the peak incidence is in women aged ≥50 years [12]
-
Infiltrating lobular carcinoma accounts for fewer than 15% of invasive breast cancers
-
Medullary carcinoma accounts for about 5% of cases and generally occurs in younger women
-
Mucinous (colloid) carcinoma is seen in fewer than 5% of invasive breast cancer cases
-
Tubular carcinoma of the breast accounts for 1-2% of all breast cancers
-
Papillary carcinoma is usually seen in women older than 60 years and accounts for approximately 1-2% of all breast cancers
-
Metaplastic breast cancer accounts for fewer than 1% of breast cancer cases, tends to occur in older women (average age of onset in the sixth decade), and has a higher incidence in Black women
Etiology
Epidemiologic studies have identified a number of risk factors that are associated with an increased risk of a woman developing breast cancer. Several risk factors have been found to be clinically useful for assessing a patient’s risk of breast cancer. Many of these factors form the basis of breast cancer risk assessment tools currently used in clinical practice.
Age and gender
Increasing age and female sex are established risk factors for breast cancer. Sporadic breast cancer is relatively uncommon among women younger than 40 years but increases significantly thereafter. The effect of age on risk is illustrated in the SEER (Surveillance, Epidemiology and End Results) data, where the incidence of invasive breast cancer for women younger than 50 years is 44.0 per 100,000 as compared with 345 per 100,000 for women aged 50 years or older. [13]
The total and age-specific incidence for breast cancer is bimodal, with the first peak occurring at about 50 years and the second occurring at about 70 years. [14, 15] It has been proposed that this bimodal pattern may reflect the influence of age within the different tumor subtypes; poorly differentiated, high-grade disease tends to occur earlier, whereas hormone-sensitive, slower-growing tumors tend to occur with advancing age.
However, a review of Carolina Breast Cancer Study data found that the bimodal peaks occurred regardless of molecular characteristics, although estrogen receptor (ER)-negative cases (as well as those with borderline, low, and intermediate ER expression) had a predominant early-onset peak, while cases with high ER expression had a predominant late-onset peak. In addition, basal-like, HER2-enriched, and luminal B cancers had predominant early-onset peaks with minor late-onset peaks, whereas luminal A cases had the most pronounced peak in late-onset cases. [15]
Family history of breast cancer
A positive family history of breast cancer is the most widely recognized risk factor for breast cancer. The lifetime risk is up to 4 times higher if a mother and sister are affected, and it is about 5 times greater in women who have two or more first-degree relatives with breast cancer. The risk is also greater among women with breast cancer in a single first-degree relative, particularly if the relative was diagnosed at an early age (≤50 years).
Despite a history indicating increased risk, many of these families have normal results on genetic testing. However, identification of additional genetic variants associated with increased risk may prove valuable. Michailidou et al conducted a controlled genome-wide association study (GWAS) of breast cancer that included 122,977 cases of European ancestry and 14,068 cases of East Asian ancestry, and identified 65 new loci associated with overall breast cancer risk. [16] A GWAS by Milne et al identified 10 variants at 9 new loci that are associated with risk of estrogen receptor–negative breast cancer. [17] A similar study by Ahearn et al identified 85 variants associated with at least one tumor feature, including 32 variants associated with triple-negative disease.{ref 212}
A family history of ovarian cancer in a first-degree relative, especially if the disease occurred at an early age (< 50 years), has been associated with a doubling of breast cancer risk. This often reflects inheritance of a pathogenic mutation in the BRCA1 or BRCA2 gene.
The family history characteristics that suggest increased risk of cancer are summarized as follows:
-
Two or more relatives with breast or ovarian cancer
-
Breast cancer occurring in an affected relative younger than 50 years
-
Relatives with both breast cancer and ovarian cancer
-
One or more relatives with two cancers (breast and ovarian cancer or 2 independent breast cancers)
-
Male relatives with breast cancer
-
BRCA1 and BRCA2 mutations
-
Ataxia telangiectasia heterozygotes (quadrupled risk)
-
Ashkenazi Jewish descent (doubled risk)
A small percentage of patients, usually with a strong family history of other cancers, have cancer syndromes. These include families with a mutation in the PTEN, TP53, MLH1, MLH2, CDH1, or STK11 gene.
To aid in the identification of mutation carriers of BRCA1/2, a number of family history–based risk assessment tools have been developed for clinical use, including the following:
-
BRCAPRO
-
Tyler Cuzick
-
Myriad I and II
-
Ontario Family History Assessment Tool (FHAT)
The National Society of Genetics Counselors provides a Find a Genetic Counselor directory. The directory lists over 3300 counselors in the United States and Canada who will meet with patients in person or by phone, video conferencing, or other virtual methods.
Direct-to-consumer genetic testing
In 2018 the US Food and Drug Administration (FDA) authorized the Personal Genome Service Genetic Health Risk (GHR) Report for BRCA1/BRCA2 (Selected Variants). This direct-to-consumer test analyzes DNA collected from a self-collected saliva sample for three specific BRCA1/BRCA2 breast cancer gene mutations that are most common in people of Ashkenazi Jewish descent. The FDA notes that more than 1,000 BRCA mutations have been identified, and the three mutations detected by this test are not the most common BRCA1/BRCA2 mutations in the general population. [18]
Reproductive factors and steroid hormones
Late age at first pregnancy, nulliparity, early onset of menses, and late age of menopause have all been consistently associated with an increased risk of breast cancer. [19, 20, 21, 22, 23] Prolonged exposure to elevated levels of sex hormones has long been postulated as a risk factor for developing breast cancer, explaining the association between breast cancer and reproductive behaviors. [24, 25]
Clinical trials of secondary prevention in women with breast cancer have demonstrated the protective effect of selective estrogen receptor modulators (SERMs) and aromatase inhibitors on recurrence and the development of contralateral breast cancers. [26] Use of SERMs in women at increased risk for breast cancer has prevented invasive ER-positive cancers. [27, 28] These data support estradiol and its receptor as a primary target for risk reduction but do not establish that circulating hormone levels predict increase risk.
A number of epidemiologic and pooled studies support an elevated risk of breast cancer among women with high estradiol levels. [29, 30] The Endogenous Hormones and Breast Cancer Collaborative Group (EHBCG) reported a relative risk of 2.58 among women in the top quintile of estradiol levels. [31]
Upon thorough review of the collective data, the Breast Cancer Prevention Collaborative Group (BCPCG) prioritized additional factors that might be included in the validation phase of a risk prediction model and gave a high priority score to free plasma estradiol levels. [30] At present, routine measurement of plasma hormone levels is not recommended in the assessment of breast cancer risk.
One of the most widely studied factors in breast cancer etiology is the use of exogenous hormones in the form of oral contraceptives (OCs) and hormone replacement therapy (HRT). [32, 33] The overall evidence suggests an approximately 25% greater risk of breast cancer among current users of OCs. The risk appears to decrease with age and time since OC discontinuance. For OC users, risk returns to that of the average population risk about 10 years after cessation.
Data obtained from case-control and prospective cohort settings support an increased risk of breast cancer incidence and mortality with the use of postmenopausal HRT. [34] Increased risk of breast cancer has been positively associated with length of exposure, with the greatest risk being observed for hormonally responsive lobular, mixed ductal-lobular, and tubular cancers. [34] Risk is greater among women taking combination HRT than among those taking estrogen-only formulations. [35, 36]
A meta-analysis by the Collaborative Group on Hormonal Factors in Breast Cancer of 58 international studies that included 143,887 postmenopausal women with invasive breast cancer and 424,972 without breast cancer concluded the following about menopausal HRT and breast cancer [37] :
-
Estrogen plus daily progestin, used for 5 years starting at age 50 years, would increase 20-year breast cancer risks at ages 50–69 years from 6.3% to 8.3%, an absolute increase of 2.0 per 100 women (one in every 50 users).
-
Estrogen plus intermittent progestin, used for 5 years, would increase the 20-year risk from 6.3% to 7.7%, an absolute increase of 1.4 per 100 women (one in 70 users).
-
Estrogen-only menopausal HRT would increase the 20-year risk from 6.3% to 6.8%, an absolute increase of 0.5 per 100 women (one in 200 users), especially in lean women, with little excess risk in obese women.
-
For 10 years of use, the 20-year increases in incidence would be about twice as great as for 5 years of use.
In the Women’s Health Initiative (WHI) trial, the incidence of invasive breast cancer was 26% higher in women randomly assigned to combination HRT than in those assigned to placebo. In contrast, the use of conjugated equine estrogen alone in women who had undergone hysterectomy was associated with a 23% (but not significant) decrease in breast cancer risk in comparison with placebo at initial reporting. On extended follow-up (median, 11.8 years), estrogen-only therapy for 5-9 years in women with hysterectomy was associated with a significant 23% reduction in the annual incidence of invasive breast cancer (0.27%; placebo, 0.35%). [38] Fewer women died of breast cancer in the estrogen-only arm.
A 23% reduction in breast cancer diagnosis in women assigned to estrogen-only HRT persisted over 16 years of cumulative follow-up in two WHI trials in more than 10,000 women (hazard ratio [HR] 0.77, 95% CI 0.62-0.92); most of the reduction was due to fewer diagnoses of estrogen receptor–positive/progesterone receptor–negative disease. In addition, breast cancer deaths were 44% lower with estrogen-only HRT (HR 0.56, 95% CI 0.34-0.92). [38]
To aid the medical community in the application of HRT, a number of agencies and groups have published recommendations for HRT use in the treatment of menopause and associated bone loss. At present, HRT is not recommended for prevention of cardiovascular disease or dementia or, more generally, for long-term use to prevent disease. Recommendations differ slightly by agency and by country. For more information see Menopausal Hormone Replacement Therapy
When prescribing HRT, the clinician should provide a discussion of the most current evidence and an assessment of the potential benefit and harm to the patient. Because of the known risk of endometrial cancer with estrogen-only formulations, the US Food and Drug Administration (FDA) currently advises the use of estrogen-plus-progesterone HRT for the management of menopausal symptoms in women with an intact uterus tailored to the individual patient, at the lowest effective dose for the shortest time needed to abate symptoms.
There are currently no formal guidelines for the use of HRT in women at high risk for breast cancer (ie, women with a family history of breast cancer, a personal history of breast cancer, or benign breast disease). Only a few studies have evaluated the effect of HRT after a diagnosis of breast cancer. The largest of these, the HABITS (Hormonal replacement therapy After Breast cancer—is IT Safe?) study was stopped early because unacceptable rates of breast cancer recurrence and contralateral disease with 2 years of HRT use (hazard ratio, 3.5). [39]
In another randomized clinical trial, no increase in the risk of breast cancer recurrences was observed in women at a median follow up of 4.1 years. [40] Use of progesterone-containing HRT was limited by intermittent use, with continuous exposure avoided.
Combination formulations containing estrogen plus progesterone are contraindicated in women with a prior history of invasive disease, a history of ductal or lobular carcinoma in situ, or a strong family history of breast cancer. This recommendation poses a significant challenge when confronted with a patient suffering severe menopausal symptoms.
Many new treatments for menopausal symptoms have been suggested (eg, clonidine, venlafaxine, gabapentin, and combination venlafaxine plus gabapentin). To date, no randomized clinical trials among women at increased risk of breast cancer or women with a history of breast cancer have assessed the overall efficacy or risks associated with these treatments. [41] Use of these agents is controversial and should target the severity of menopausal symptoms.
Other hormone-based approaches (eg, low-dose vaginal estrogen for vaginal and urinary symptoms, including dyspareunia) are generally considered to be safer, particularly in patients receiving SERMs. However, these agents may also carry a slight increased risk, in that they are capable of raising estradiol levels, at least transiently, depending on the dose and frequency of administration. Little evidence supports the benefit of commonly used dietary isoflavones, black cohosh, or vitamin E.
Prior breast health history
A history of breast cancer is associated with a 3- to 4-fold increased risk of a second primary cancer in the contralateral breast. [42, 43, 44] The presence of any premalignant ductal carcinoma in situ (DCIS) or LCIS confers an 8- to 10-fold increase in the risk of developing breast cancer in women who harbor untreated preinvasive lesions. [45, 46]
A history of breast biopsy that is positive for hyperplasia, fibroadenoma with complex features, sclerosing adenosis, and solitary papilloma have been associated with a modest (1.5- to 2-fold) increase in breast cancer risk. [45, 46] In contrast, any diagnosis of atypical hyperplasia that is ductal or lobular in nature, especially in a woman under the age of 45 years, carries a 4- to 5-fold increased risk of breast cancer, with the increase rising to 8- to 10-fold among women with multiple foci of atypia or calcifications in the breast. [47]
Benign breast lesions, including fibrocystic disease such as fibrocystic change without proliferative breast disease or fibroadenoma, have not been associated with increased risk. [48]
Lifestyle risk factors
The wide variability of breast cancer incidence around the world (eg, the nearly 5-fold difference between Eastern Africa and Western Europe) has long been attributed to differences in dietary intake and reproductive patterns. [49, 50, 51, 52] In general, rates differ according to the level of industrial development: there are more than 80 cases per 100,000 in developed countries, compared with fewer than 40 per 100,000 in less developed countries.
As with cancers of the colon and prostate, diets that are rich in grains, fruits, and vegetables; low in saturated fats; low in energy (calories); and low in alcohol—the more common pattern in less-industrialized countries—are thought to be protective against breast cancer. [53]
One such diet is the Mediterranean diet, which comprises a high intake of plant proteins, whole grains, fish, and monounsaturated fat, as well as moderate alcohol intake and low intake of refined grains, red meat, and sweets. The Netherlands Cohort Study, which included 62,573 women aged 55-69 years with more than 20 years of follow-up, found that close adherence to a Mediterranean diet is associated with lower risk for breast cancer—in particular, for types of breast cancer that carry a poorer prognosis in postmenopausal women. [54]
Compared with women who reported the least adherence to a Mediterranean diet, women who most closely adhered to the diet had a 40% reduced risk for estrogen receptor–negative (ER-) breast cancer, (hazard ratio [HR], 0.60; ptrend = 0.032) and a 39% reduced risk for progesterone receptor–negative (PR-)/ER- disease (HR, 0.61; ptrend = 0.047). The study found no significant associations with the diet and the risk of ER+ disease or total breast cancer risk. [54]
Obesity
Increased risk of postmenopausal breast cancer has been consistently associated with the following:
-
Western dietary pattern (high energy content in the form of animal fats and refined carbohydrates)
-
Sedentary lifestyle
-
Regular, moderate consumption of alcohol (3-5 alcoholic beverages per week)
The Western lifestyle (ie, chronic excess energy intake from meat, fat, and carbohydrates and lack of exercise) strongly correlates with development of the following:
-
Obesity, particularly abdominal obesity
-
Chronic hyperinsulinemia
-
Higher production and availability of insulinlike growth factor (IGF)-1
Studies of dietary fat, total energy, and meat intake levels have largely been inconsistent in population studies of adult women with regard to risk of breast cancer. In contrast, epidemiologic studies have more consistently found a positive relation between breast cancer risk and early-life exposures such as diet, obesity, and body size (including height). [59, 60, 61] The mechanism of this relation is unknown.
Environmental risk factors
A number of environmental exposures have been investigated in relation to breast cancer risk in humans, including the following [62, 63, 64, 65] :
-
Tobacco smoke (both active and passive exposure)
-
Dietary (eg, charred and processed meats)
-
Alcohol consumption
-
Environmental carcinogens (eg, exposure to pesticides, radiation, and environmental and dietary estrogens)
Alcohol consumption has been linked with breast cancer. [66, 67, 68] Regular consumption of alcoholic beverages can prevent the absorption of nutrients, contribute to weight gain, and raise the levels of estrogen. [67]
High doses of ionizing radiation to the chest area, particularly during puberty, have been unequivocally linked with an increased risk of breast cancer in adulthood. [65, 69] Because of the strong association between ionizing radiation exposure and breast cancer risk, medical diagnostic procedures are performed in such a way as to minimize exposure to the chest area, particularly during adolescence.
Women with a history of radiation exposure to the chest area should be examined and counseled regarding their risk of breast cancer on the basis of the timing and dose of the previous exposure. A patient treated for Hodgkin lymphoma with Mantel radiation that includes the breasts in the radiation field has a 5-fold higher risk of developing breast cancer. This risk increases markedly for women treated during adolescence [70] ; evidence suggests that cumulative risk increases with age as a function of age of exposure and type of therapy. [71]
Current evidence does not support a significant and reproducible link between other environmental exposures and breast cancer risk. Thus, a number of factors remain suspect but unproven.
Epidemiology
United States statistics
In the United States, approximately 297,790 new cases of invasive breast cancer in women are predicted to occur in 2023, along with 2800 cases in men. [9] Among US women in 2023, in addition to invasive breast cancer, 55,720 new cases of ductal carcinoma in situ (DCIS) are expected to be diagnosed. [9]
The incidence of breast cancer in the United States increased rapidly from 1980 to 1987, largely as a consequence of the widespread use of mammography screening, which led to increased detection of asymptomatic small breast tumors. After 1987, the increase in overall rates of invasive breast cancers slowed significantly, specifically among White women aged 50 years or older. Incidence over this period of time varied dramatically by histologic type. Common ductal carcinomas increased modestly from 1987 to 1999, whereas invasive lobular and mixed ductal-lobular carcinomas increased dramatically during this time period. [72]
Whereas a decline in invasive breast cancer rates was evident as early as 1999, rates decreased dramatically in women aged 50 years or older between 2001 and 2004. During this same period, no significant change was observed in the incidence of ER-negative cancers or cancers in women younger than 50 years. The decline in rates from 2001 to 2004 was greatest between 2002 and 2003 and was limited to non-Hispanic whites. [73, 74, 75, 76]
The reason for the decline has been extensively debated. Breast cancer rates decreased significantly after the reports from the Million Women Study [77] and the Women’s Health Initiative showing higher numbers of breast cancers in women using combination HRT with estrogen and progestin for menopausal symptoms. The near-immediate decrease in the use of combination HRT for that purpose has been widely accepted as a primary explanation for the decrease in breast cancer rates. [75]
However, Jemal and Li argued that the decline in breast cancer incidence started earlier than the reduction in combination HRT use and that the decline is due in part to a “saturation” in mammographic screening mammography that produced a plateau in incidence when such screening stabilized in the late 1990s. [72, 74] Saturation of the population would be predicted to reduce the pool of undiagnosed or prevalent cases.
For women aged 69 years or older, breast cancer rates started to decline as early as 1998, when screening first showed a plateau. This observation is consistent with the prediction that if widespread screening and earlier detection are effective, they should result in a peak incidence among women during the sixth and seventh decades of life, followed by a decline. This is exactly the pattern now being reported for screened populations. [78]
The second observation noted by Jemal et al was that despite evidence for a plateau effect, screening saturation alone could not explain the dramatic declines or the pattern of decline. The decline in incidence was observed only for ER-positive tumors and not for ER-negative ones; these findings support the competing hypothesis that exposure to HRT as estrogen in combination with synthetic progesterone promoted the growth of undetected tumors.
Under this scenario, withdrawal of combination HRT at the population level may have resulted in regression or a slowing of tumor growth. The latter, it has been argued, would result in a delay in detection. Overall, incidence figures from 2005-2009, for which the most recent data are currently available, suggest that overall new breast cancer case rates have remained fairly stable since the initial drop.
It is notable, however, that the annual percentage change from 2005 to 2009 increased in women aged 65-74 years by 2.7% during this period, rates that parallel 2001 incidence figures for this age group. [13] This rise occurred in spite of very low use of HRT by this population [79] and suggests that the drop in combination HRT use immediately after 2002 may not have resulted in a sustained decrease in new breast cancer cases.
At present, it is unclear whether decreased use of combination HRT has resulted in a sustained reduction in the incidence of breast cancer at the population level or has shifted the age at which preexisting disease would become detectable. Longer-term follow-up of post-2002 trends in relation to combination HRT use are needed to address this question.
In 2010-2019, the incidence of invasive breast cancer incidence rose by 0.4% per year in women older than 50 and 1% per year in women ages 20-49 years. The incidence of DCIS declined by 0.7% and 0.8% per year in each age group, respectively. [80]
International statistics
The final decades of the 20th century saw worldwide increases in the incidence of breast cancer, with the highest rates reported in Westernized countries. Reasons for this trend are largely attributed to introduction of screening mammography. Changes in reproductive patterns—particularly fewer children and later age at first birth—may also have played a role, as may changes in lifestyle factors, including the following:
-
Western dietary patterns
-
Decreased physical activity
-
Rising obesity rates
-
More widespread use of exogenous hormones for contraception and treatment of menopausal symptoms
The beginning of the 21st century saw a dramatic decrease in breast cancer incidence in a number of Westernized countries (eg, the United Kingdom, France, and Australia). These decreases paralleled those noted in the United States and reflected similar patterns of mammography screening and decreased use of combination HRT. [8]
In 2020, there were an estimated 2.26 million new cases of invasive breast cancer worldwide. The 2020 incidence of female breast cancer ranged from 26.2 cases per 100,000 in South Central Asia to 95.5 cases per 100,000 in Australia/New Zealand. [8]
Age-related demographics
The incidence rate of breast cancer increases with age, from 1.5 cases per 100,000 in women 20-24 years of age to a peak of 421.3 cases per 100,000 in women 75-79 years of age; 95% of new cases occur in women aged 40 years or older. The median age of women at the time of breast cancer diagnosis is 63 years. [13] Among women over the age of 50, breast cancer incidence rates were relatively stable from 2005-2014. In contrast, incidence rates, among women under age 50 have increased 0.2% per year since the mid-1990s. [80]
Rates of in situ breast cancer stabilized among women 50 years and older in the late 1990s; this is consistent with the proposed effects of screening saturation. However, the incidence of in situ breast cancer continues to increase in younger women. [80]
Race- and ethnicity-related demographics
In the United States, the incidence of breast cancer is higher in non-Hispanic Whites than in women of other racial and ethnic groups. Among women younger than 40 years, African Americans have a higher incidence. In addition, a larger proportion of African-American women are diagnosed with larger, advanced-stage tumors (> 5 cm) and are more likely to die of breast cancer at every age. [80]
According to the American Cancer Society (ACS), breast cancer rates per 100,000 among women from various racial and ethnic groups are as follows [80] :
-
Non-Hispanic White: 133.7
-
Non-Hispanic Black: 127.8.5
-
American Indian/Alaskan Native: 111.3
-
Asian/Pacific Islander: 101.3
-
Hispanic: 99.2
According to the ACS, death rates per 100,000 from breast cancer among women from various racial and ethnic groups are as follows:
-
Non-Hispanic White: 19.7
-
Non-Hispanic Black: 27.6
-
American Indian/Alaska Native: 20.5
-
Hispanic/Latina: 11.7
-
Asian/Pacific Islander: 13.7
Among US women from 2011 through 2020, breast cancer death rates declined by 1% to 1.4% per year in Hispanic, Black, and White women, declined by 0.6% per year in Asians/Pacific islanders, and were stable in American Indians/Alaskan Natives. Breast cancer death rates in Black women began to exceed those in White women in the early 1980s, and the disparity remains large; in 2016-2020, breast cancer death rates were 40% higher in Black women than White women. [80]
Prognosis
From 1990 through 2015, death rates from breast cancer in the United States decreased 39%. The decrease occurred in both younger and older women, but has slowed among women younger than 50 since 2007. [80]
The decrease in breast cancer death rates is thought to represent progress in both earlier detection and improved treatment modalities. [9] The 2022 estimates are 43,780 expected breast cancer deaths (43,250 in women, 530 in men). [9]
Prognostic and predictive factors
Numerous prognostic and predictive factors for breast cancer have been identified by the College of American Pathologists (CAP) to guide the clinical management of women with breast cancer. Breast cancer prognostic factors include the following:
-
Axillary lymph node status
-
Tumor size
-
Lymphatic/vascular invasion
-
Patient age
-
Histologic grade
-
Histologic subtypes (eg, tubular, mucinous [colloid], or papillary)
-
Response to neoadjuvant therapy
-
Estrogen receptor/progesterone receptor (ER/PR) status
-
HER2 gene amplification or overexpression
Cancerous involvement of the lymph nodes in the axilla is an indication of the likelihood that the breast cancer has spread to other organs. Survival and recurrence are independent of level of involvement but are directly related to the number of involved nodes.
Patients with node-negative disease have an overall 10-year survival rate of 70% and a 5-year recurrence rate of 19%. In patients with lymph nodes that are positive for cancer, the recurrence rates at 5 years are as follows:
-
One to three positive nodes – 30-40%
-
Four to nine positive nodes – 44-70%
-
≥10 positive nodes – 72-82%
Hormone receptor–positive tumors generally have a more indolent course and are responsive to hormone therapy. ER and PR assays are routinely performed on tumor material by pathologists; immunohistochemistry (IHC) is a semiquantitative technique that is observer- and antibody-dependent.
This prognostic information can guide physicians in making therapeutic decisions. Pathologic review of the tumor tissue for histologic grade, along with the determination of ER/PR status and HER2 status, is necessary for determining prognosis and treatment. Evaluation of lymph node involvement by means of sentinel lymph node biopsy or axillary lymph node dissection is generally necessary as well. [81] (See the Staging section in this article as well as Breast Cancer Staging.)
HER2
In the past, HER2 overexpression was associated with a more aggressive tumor phenotype and a worse prognosis (higher recurrence rate and increased mortality), independent of other clinical features (eg, age, stage, and tumor grade), especially in patients who did not receive adjuvant chemotherapy. Prognosis has improved with the routine use of HER2-targeted therapies, which consist of the following:
-
Trastuzumab – Monoclonal antibody
-
Pertuzumab – Monoclonal antibody
-
Lapatinib – A small-molecule oral tyrosine kinase inhibitor
-
Neratinib – A small-molecule oral tyrosine kinase inhibitor
-
Ado-trastuzumab emtansine – An antibody-drug conjugate directed specifically to the HER2 receptor
-
Trastuzumab deruxetacan – An antibody-drug conjugate specifically directed against HER2 receptor
HER2 status has also been shown to predict response to certain chemotherapeutic agents (eg, doxorubicin). Retrospectively analyzed results from clinical trials have shown that HER2-positive patients benefit from anthracycline-based regimens, perhaps because of the frequent coamplification of topoisomerase II with HER2. (See Breast Cancer and HER2.)
Molecular profiling assays
In patients with early breast cancer—ER-positive, HER2-negative, and node-negative or with 1-3 positive nodes—genetic testing of the tumor can be used to determine the risk of recurrence, and the likely benefit from chemotherapy. Multiple assays that have been developed and validated for this purpose; see Workup/Tumor Genetic Testing.
Prognosis by cancer type
DCIS is divided into comedo (ie, cribriform, micropapillary, and solid) and noncomedo subtypes, a division that provides additional prognostic information on the likelihood of progression or local recurrence. Generally, the prognosis is worse for comedo DCIS than for noncomedo DCIS (see Workup/Histology).
Approximately 10-20% of women with LCIS develop invasive breast cancer within 15 years after their LCIS diagnosis. Thus, LCIS is considered a biomarker of increased breast cancer risk.
Infiltrating ductal carcinoma is the most commonly diagnosed breast tumor and has a tendency to metastasize via lymphatic vessels. Like ductal carcinoma, infiltrating lobular carcinoma typically metastasizes to axillary lymph nodes first. However, it also has a tendency to be more multifocal. Nevertheless, its prognosis is comparable to that of ductal carcinoma.
Typical or classic medullary carcinomas are often associated with a good prognosis despite the unfavorable prognostic features associated with this type of breast cancer, including ER negativity, high tumor grade, and high proliferative rates. However, an analysis of 609 medullary breast cancer specimens from various stage I and II National Surgical Adjuvant Breast and Bowel Project (NSABP) protocols indicates that overall survival and prognosis are not as good as previously reported. Atypical medullary carcinomas also carry a poorer prognosis.
Overall, patients with mucinous carcinoma have an excellent prognosis, with better than 80% 10-year survival. Similarly, tubular carcinoma has a low incidence of lymph node involvement and a very high overall survival rate.
Cystic papillary carcinoma has a low mitotic activity, which results in a more indolent course and a good prognosis. However, invasive micropapillary ductal carcinoma has a more aggressive phenotype, even though approximately 70% of cases are ER-positive. A retrospective review of 1400 cases of invasive carcinoma identified 83 cases (6%) with at least one component of invasive micropapillary ductal carcinoma. [82]
Additionally, lymph node metastasis is frequently seen in this subtype (incidence, 70-90%), and the number of lymph nodes involved appears to correlate with survival.
For metaplastic breast cancer, the majority of published case series have demonstrated a worse prognosis than with infiltrating ductal carcinoma, even when adjusted for stage, with a 3-year overall survival rate of 48-71% and 3-year disease-free survival rate of 15-60%. [83] In most case series, large tumor size and advanced stage have emerged as predictors of poor overall survival and prognosis. [84] Nodal status does not appear to impact survival in metaplastic breast cancer.
Paget disease of the breast is associated with an underlying breast cancer in 75% of cases. Breast-conserving surgery can achieve satisfactory results, but at the risk of local recurrence. Poor prognostic factors include a palpable breast tumor, lymph node involvement, histologic type, and age of less than 60 years. Paget disease with a palpable mass usually has an invasive component and a lower 5-year survival rate (20-60%). Those that do not have an underlying palpable mass have a higher 5-year survival rate (75-100%). [85, 86]
Cardiovascular disease
Cardiovascular disease (CVD) risk is increased in women with breast cancer. The increase is due in part to the cardiotoxic effects of some breast cancer treatments (eg, chemotherapy, radiotherapy, hormonal therapies, targeted therapy such as trastuzumab). In addition, breast cancer and CVD, share several risk factors, including smoking, obesity, and the typical Western diet. [87]
In older breast cancer survivors, risk for the development of the CVD risk factors obesity and dyslipidemia is higher than the risk of tumor recurrence. In the population of older postmenopausal women, breast cancer survivors are at higher risk for mortality attributable to CVD, compared with women without a history of breast cancer. The increased risk becomes manifest approximately 7 years after the diagnosis of breast cancer. [87]
-
Anatomy of the breast.
-
Intrinsic subtypes of breast cancer.
-
Breast cancer. Intraductal carcinoma, comedo type. Distended duct with intact basement membrane and central tumor necrosis.
-
Breast cancer. Intraductal carcinoma, noncomedo type. Distended duct with intact basement membrane, micropapillary, and early cribriform growth pattern.
-
Breast cancer. Lobular carcinoma in situ. Enlargement and expansion of lobule with monotonous population of neoplastic cells.
-
Breast cancer. Lobular carcinoma in situ. Enlargement and expansion of lobule with monotonous population of neoplastic cells.
-
Breast cancer. Infiltrating ductal carcinoma. Low-grade carcinoma with well-developed glands invading fibrous stroma.
-
Breast cancer. Colloid (mucinous) carcinoma. Nests of tumor cells in pool of extracellular mucin.
-
Breast cancer. Papillary carcinoma. Solid papillary growth pattern with early cribriform and well-developed thin papillary fronds.
-
Anatomy of the breast. Courtesy of Wikimedia Commons (Patrick J Lynch, medical illustrator).
Tables
What would you like to print?
- Overview
- Presentation
- DDx
- Workup
- Treatment
- Approach Considerations
- Treatment of Invasive Breast Cancer
- Systemic Adjuvant Therapy for Breast Cancer
- Treatment of Carcinoma in Situ
- Treatment of Locally Advanced and Inflammatory Breast Cancer
- Systemic Treatment of Metastatic Breast Cancer
- Surgical Treatment of Metastatic Breast Cancer
- Pharmacologic Reduction of Breast Cancer Risk
- Prophylactic Mastectomy
- Long-Term Monitoring
- Integrative Therapy
- Show All
- Guidelines
- Medication
- Medication Summary
- Antineoplastics, Alkylating
- Antineoplastics, Anthracycline
- Calcium Metabolism Modifiers
- Antineoplastics, Antimetabolite
- Antineoplastics, Vinca Alkaloid
- Monoclonal Antibodies
- Tyrosine Kinase Inhibitors
- Antineoplastics, Antimicrotubular
- Aromatase Inhibitors
- CDK Inhibitors
- Antineoplastics, PARP Inhibitors
- Antineoplastics, Estrogen Receptor Antagonist
- PD-1/PD-L1 Inhibitors
- PI3K Inhibitors
- AKT Inhibitors
- Show All
- Questions & Answers
- Media Gallery
- Tables
- References