Practice Essentials
Microscopic polyangiitis (MPA) is a vasculitis of small vessels. Patients frequently present with renal manifestations, but systemic manifestations, arthritis, mononeuritis multiplex, and other signs and symptoms are also common. [1, 2] (See Presentation and Workup.)
Vasculitis in small vessels, including arterioles, capillaries, and venules, a characteristic of MPA, is absent in polyarteritis nodosa. This absence is the proposed distinguishing feature between those two disorders. Granulomatosis with polyangiitis (Wegener granulomatosis, GPA), MPA, and eosinophilic granulomatosis with polyangiitis (Churg-Strauss syndrome, EGPA) comprise a category of small vessel vasculitis related to antineutrophil cytoplasmic antibodies (ANCAs) and are characterized by a paucity of immune deposits.
MPA and GPA seem to be part of a clinical spectrum. However, an absence of granuloma formation and sparing of the upper respiratory tract are features of MPA. These features help to distinguish MPA from GPA, although the two conditions are occasionally difficult to distinguish.
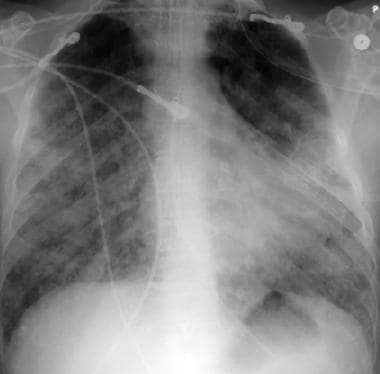
The image below depicts pulmonary alveolar capillaritis.
Immunosuppressive medications are used to control MPA. [3] The choice of agents depends in part on the extent of disease, the rate of progression, and the degree of inflammation. See Treatment and Medication.
Background
MPA was initially considered as a microscopic form of polyarteritis nodosa. In 1990, the American College of Rheumatology developed classification criteria for several types of systemic vasculitis but did not distinguish between polyarteritis nodosa and microscopic polyarteritis nodosa. [4]
In 1994, a group of experts held an international consensus conference in Chapel Hill, North Carolina, to attempt to redefine the classification of small-vessel vasculitides. [5, 6] A second International Chapel Hill Consensus Conference was held in 2012. [7] The conference recommended categorizing small-vessel vasculitis as follows:
-
ANCA-associated vasculitis (AAV) - MPA, GPA, EGPA
-
Immune complex–associated small-vessel vasculitis - Anti-glomerular basement membrane (anti-GBM) disease, cryoglobulinemic vasculitis, IgA vasculitis (Henoch-Schönlein), hypocomplementemic urticarial vasculitis (anti-C1q vasculitis)
In addition, the conference recommended adding the following categories of vasculitis:
-
Variable vessel vasculitis - Behcet disease, Cogan syndrome
-
Single-organ vasculitis (eg, cutaneous leukocytoclastic angiitis, isolated aortitis)
-
Vasculitis associated with systemic disease (eg, lupus, rheumatoid arthritis, sarcoid)
-
Vasculitis associated with probable etiology (eg, hepatitis, drugs, cancer)
Classification criteria
The American College of Rheumatology (ACR) and the European Alliance of Associations for Rheumatology (EULAR) have published classification criteria for MPA. The criteria are intended tobe used for enrolling patients in studies, not for clinical diagnosis. The classification criteria should be applied after a diagnosis of small- or medium-vessel vasculitis has been made, and alternative disorders mimicking vasculitis have been excluded. [8]
Criteria and assigned scores are as follows [8] :
-
Positive test for perinuclear antineutrophil cytoplasmic antibodies (p-ANCA) or antimyeloperoxidase (anti-MPO) antibodies: +6
-
Pauci-immune glomerulonephritis: +3
-
Lung fibrosis or interstitial lung disease: +3
-
Sino-nasal symptoms or signs: -3
-
Positive test for cytoplasmic antineutrophil cytoplasmic antibodies (c-ANCA) or antiproteinase 3 (anti-PR3) antibodies: -1
-
Blood eosinophil count ≥ 1 × 10 9/L: -4
For the purposes of classification, a patient with a total score of 5 or more is said to have MPA. These criteria have a sensitivity of 91% and a specificity of 94%. [8]
Pathophysiology
Vasculitis is inflammation of the vessel walls. This may lead to necrosis and bleeding. MPA is characterized by pauci-immune, necrotizing, small-vessel vasculitis without clinical or pathological evidence of granulomatous inflammation.
Etiology
Based on current understanding of the inflammatory response, cytokine-mediated changes in the expression and function of adhesion molecules coupled with inappropriate activation of leukocytes and endothelial cells are postulated to be the primary factors influencing the degree and location of vessel damage in the vasculitis syndromes. However, the stimuli that initiate these pathologic inflammatory changes are not well understood.
ANCA may play a role in the pathogenesis of MPA.
Case reports have described an association of MPA with medications (eg, propylthiouracil, hydralazine, rifampicin, ethambutol) and with diseases such as primary biliary cirrhosis. [9, 10, 11]
Epidemiology
With the increased availability of ANCA testing, reported cases of MPA have also risen. A 20-year population-based study in Rochester, Minnesota estimated the incidence of MPA at 1.6 per 100,000 persons. [12]
Internationally, the incidence is approximately two cases per 100,000 persons in the United Kingdom. In Sweden and Germany, the incidence is estimated to be 1.3 per 100,000 persons. [13, 14]
The median age of onset is approximately 50 years. MPA is more common in White persons than Black persons; males are affected slightly more frequently than females.
Prognosis
With treatment, 90% of patients with MPA improve and 75% achieve complete remission. The 5-year survival rate is approximately 75%. MPA carries a worse long-term survival rate than granulomatosis with polyangiitis (GPA) or Churg-Strauss syndrome, probably because of kidney involvement at disease onset.
Of patients with MPA, 30% relapse in 1-2 years. Oh et al reported that neither myeloperoxidase (MPO)-ANCA nor proteinase 3 (PR3)-ANCA positivity at diagnosis affected prognosis. However, risk of relapse was significantly higher in patients with chest and renal manifestations, Birmingham vasculitis activity score ≥13.5, or five factor score ≥1. [15]
Long-term damage in a study of 296 patients with MPA or GPA, as measured with the Vasculitis Damage Index (VDI), was associated with the severity of initial disease, older age, the number of relapses, and duration of glucocorticoid treatment. Patients were followed for 7 years post-diagnosis. Mean duration of glucocorticoid treatment was 40.4 months. [16]
In another study of 151 patients with ANCA-associated vasculitis, patients presenting with pulmonary involvement at baseline had higher damage and disease activity scores at 6, 12 and 24 months follow-up. Patients presenting with lung involvement had an increased risk of developing cardiovascular and kidney involvement and were more likely to develop pulmonary fibrosis. [17]
Complications of vasculitis depend on the particular organ system involvement (see Physical). One of the most significant complications of treatment is bladder cancer. Of patients treated with cyclophosphamide, 5% develop bladder cancer after 10 years and 16% develop bladder cancer after 15 years.
One study reviewed cardiovascular outcomes during long-term follow-up of patients with MPA and GPA in the first 4 European Vasculitis Study Group trials. A model was developed and validated to predict those at risk for a cardiovascular event. Older age, diastolic hypertension, and positive PR3-ANCA status were found to be independent determinants of cardiovascular outcomes. Within 5 years of diagnosis, 14% of patients experienced a cardiovascular event. [18]
The French Vasculitis Study Group Relapse Score (FRS) was developed to predict the probability of relapse in patients with MPA or GPA. [19] The FRS assigns each of the following features 1 point:
-
PR3-ANCA positivity
-
Estimated glomerular filtration rate (eGFR) ≥30 mL/min/1.73 m²
-
Age ≤75 years
In the validation cohort, the FRS score and associated 5-year relapse risk was as follows:
-
FRS 0: 8%
-
FRS 1: 30%
-
FRS 2: 48%
-
FRS 3: 76%
Patient Education
Patients with MPA should be aware of the severity of the disease and the risk of recurrence. Compliance with medications and follow-up visits is critical.
-
Pulmonary alveolar capillaritis.
-
Histopathology of alveolar hemorrhage in alveolar capillaritis.
-
Crescentic glomerulonephritis.
-
Focal segmental glomerulonephritis.
-
Histopathology of leukocytoclastic angiitis.
-
Leukocytoclastic angiitis.