Background
Campylobacter infections are among the most common bacterial infections in humans. They produce both diarrheal and systemic illnesses. In industrialized regions, enteric Campylobacter infections produce an inflammatory, sometimes bloody, diarrhea or dysentery syndrome. [1]
Campylobacter jejuni usually is the most common cause of community-acquired inflammatory enteritis. In developing regions, diarrhea may be watery. [1]
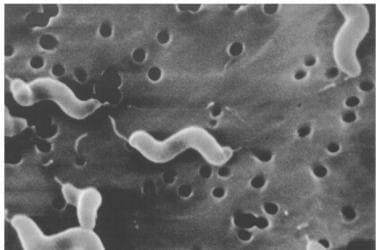 Scanning electron microscope image of Campylobacter jejuni, illustrating its corkscrew appearance and bipolar flagella. Source: Virginia-Maryland Regional College of Veterinary Medicine, Blacksburg, Virginia.
Scanning electron microscope image of Campylobacter jejuni, illustrating its corkscrew appearance and bipolar flagella. Source: Virginia-Maryland Regional College of Veterinary Medicine, Blacksburg, Virginia.
Infections with Campylobacter-like organisms can produce an enterocolitis/proctocolitis syndrome in homosexual males, who are at increased risk for Helicobacter cinaedi and Helicobacter fennelliae infections. [2] Bacteremia also can occur with H fennelliae. [3] C jejuni infections also may produce serious bacteremic conditions in individuals with AIDS. Most reported bacteremias have been due to Campylobacter fetus infection. Campylobacter lari, which is found in healthy seagulls, also has been reported to produce mild recurrent diarrhea in children. Campylobacter upsaliensis may cause diarrhea or bacteremia, whereas Campylobacter hyointestinalis, which has biochemical characteristics similar to those of C fetus, causes occasional bacteremia in immunocompromised individuals.
Campylobacter organisms also may be an important cause of traveler's diarrhea, especially in Thailand and surrounding areas of Southeast Asia. In a study of American military personnel deployed in Thailand, more than half of those with diarrhea were found to be infected with Campylobacter species.
Pathophysiology
Campylobacter is said to be prevalent in food animals such as poultry, cattle, pigs, sheep, and ostriches, as well as pets, including cats and dogs.
The known routes of Campylobacter transmission include fecal-oral, person-to-person sexual contact, unpasteurized raw milk and poultry ingestion, and waterborne (ie, through contaminated water supplies). Exposure to sick pets, especially puppies, also has been associated with Campylobacter outbreaks. [1]
Transmission of Campylobacter organisms to humans usually occurs via infected animals and their food products. Most human infections result from the consumption of improperly cooked or contaminated foodstuffs. Chickens may account for 50% to 70% of human Campylobacter infections. Most colonized animals develop a lifelong carrier state.
Campylobacter has been found in shellfish. [4, 5]
The infectious dose is 1000-10,000 bacteria. Campylobacter infection has occurred after ingestion of 500 organisms by a volunteer; however, a dose of fewer than 10,000 organisms is not a common cause of illness. Campylobacter species are sensitive to hydrochloric acid in the stomach. Conditions in which acid secretion is blocked, for example, by antacid treatment or disease, predispose patients to Campylobacter infections.
Symptoms of Campylobacter infection begin after an incubation period of up to a week. The sites of tissue injury include the jejunum, the ileum, and can extend to involve the colon and rectum. C jejuni appears to invade and destroy epithelial cells. C jejuni is attracted to mucus and fucose in bile, and the flagella may be important in both chemotaxis and adherence to epithelial cells or mucus. Adherence may also involve lipopolysaccharides or other outer membrane components. Such adherence would promote gut colonization. PEB 1 is a superficial antigen that appears to be a major adhesin and is conserved among C jejuni strains.
Some strains of C jejuni produce a heat-labile, cholera-like enterotoxin, which is important in watery diarrhea observed in infections. Infection with the organism produces diffuse, bloody, edematous, and exudative enteritis. The inflammatory infiltrate consists of neutrophils, mononuclear cells, and eosinophils. Crypt abscesses develop in the epithelial glands, and ulceration of the mucosal epithelium occurs.
Cytotoxin production has been reported in Campylobacter strains from patients with bloody diarrhea. In a small number of cases, the infection is associated with the hemolytic-uremic syndrome and thrombotic thrombocytopenic purpura through a poorly understood mechanism. Endothelial cell injury, mediated by endotoxins or immune complexes, is followed by intravascular coagulation and thrombotic microangiopathy in the glomerulus and the gastrointestinal mucosa.
Campylobacter species produce the bacterial toxin cytolethal distending toxin (CDT), which produces a cell block at the G2 stage preceding mitosis. CDT inhibits cellular and humoral immunity via the destruction of immune response cells and necrosis of epithelial-type cells and fibroblasts involved in the repair of lesions. This leads to slow healing and results in disease symptoms. [6]
In patients with HIV infection, Campylobacter infections may be more common, may cause prolonged or recurrent diarrhea, and may be more commonly associated with bacteremia and antibiotic resistance.
C fetus is covered with a surface S-layer protein that functions like a capsule and disrupts c3b binding to the organisms, resulting in both serum and phagocytosis resistance.
C jejuni infections also show recurrence in children and adults with immunoglobulin deficiencies. Acute C jejuni infection confers short-term immunity. Patients develop specific immunoglobulin G (IgG), immunoglobulin M (IgM), and immunoglobulin A (IgA) antibodies in serum; IgA antibodies also develop in intestinal secretions. The severity and persistence of C jejuni infections in individuals with AIDS and hypogammaglobulinemia indicate that both cell-mediated and humoral immunity are important in preventing and terminating infection.
The oral cavity contains numerous Campylobacter species, such as Campylobacter concisus, that have been associated with a subtype of inflammatory bowel disease. [7, 8] Campylobacter gracilis is associated with periodontal disease, [9] pleuropulmonary disease, and bacteremia.
Epidemiology
Frequency
United States
An estimated 1.5 million cases of Campylobacter infections occur annually in the United States. [10]
In 2020 the incidence of Campylobacter was 20 per 100,000 population. FoodNet surveillance tracks eight foodborne pathogens (including Campylobacter), and a 26% reduction was noted in 2020 as compared to 2017-2019. [11]
International
C jejuni infections are extremely common worldwide, although exact figures are not available, particularly in low- and middle-income countries. In high-income countries, the incidence has been estimated to be 4.4 to 9.3 per 1000 population. [12] Czech Republic reported the highest national campylobacteriosis rate in 2019, at 126.1 per 100,000 in 2019. [13]
Mortality/Morbidity
Campylobacter infections are usually self-limited and rarely cause mortality. Exact figures are unavailable, but occasional deaths have been attributed to Campylobacter infections, typically in elderly or immunocompromised persons and secondary to volume depletion in young, previously healthy individuals.
Race
Campylobacter infections have no clear racial predilection.
Sex
Campylobacter organisms are isolated more frequently from males than females. Homosexual men appear to be at increased risk for infection with atypical Campylobacter species such as Helicobacter cinaedi and H fennelliae.
Age
Campylobacter infections can occur in all age groups.
Studies show a peak incidence in children younger than 1 year and in persons aged 15 to 29 years. The age-specific attack rate is highest in young children. In the United States, the highest incidence of Campylobacter infection in 2010 was in children younger than 5 years and was 24.4 cases per 100,000 population, [14] However, the rate of fecal cultures positive for Campylobacter species is greatest in adults and older children.
Asymptomatic Campylobacter infection is uncommon in adults.
In developing countries, Campylobacter infection is very common in the first 2 years of life. Asymptomatic infection is also more common. [15]
For additional information on pediatric Campylobacter infections, see Campylobacter Infections.
-
Scanning electron microscope image of Campylobacter jejuni, illustrating its corkscrew appearance and bipolar flagella. Source: Virginia-Maryland Regional College of Veterinary Medicine, Blacksburg, Virginia.







