Overview
Introduction to Functional Endoscopic Sinus Surgery
Rhinology and sinus surgery have undergone a tremendous expansion since the discourses of Messerklinger and Wigand in the late 1970s. [1, 2, 3] Imaging advances, increased understanding of the anatomy and the pathophysiology of chronic sinusitis, and image-guided surgery have allowed surgeons to perform more complex procedures with increased safety.
Outstanding short- and long-term results have been reported in the literature. Senior et al reported that symptoms improved in 66 of 72 (91.6%) patients following endoscopic sinus surgery, with a mean follow-up time of 7.8 years. [4] In addition, endoscopic sinus surgery significantly influences quality of life; Damm et al reported an improvement in quality of life for 85% of their patient population, with a mean follow-up time of 31.7 months. [5]
Although functional endoscopic sinus surgery is the primary approach used today for the surgical treatment of chronic sinusitis, the time-honored external approaches still play a role. Therefore, familiarity with endoscopic and external approaches, in conjunction with a precise understanding of the anatomy, ensures optimal patient care and outcome.
A recently developed alternative to functional endoscopic sinus surgery is balloon sinuplasty. This technique uses balloon catheters to dilate the maxillary, frontal, and sphenoid natural ostia without bone or soft-tissue removal. Reports show persistent patient symptom improvement and sinus ostia patency. Further study and long-term outcomes with this technology will determine its role in endoscopic sinus surgery. [6]
Indications for Endoscopic Sinus Surgery
Endoscopic sinus surgery is most commonly performed for inflammatory and infectious sinus disease. The most common indications for endoscopic sinus surgery are as follows:
-
Chronic sinusitis refractory to medical treatment
-
Recurrent sinusitis
-
Nasal polyposis
-
Antrochoanal polyps
-
Sinus mucoceles
-
Excision of selected tumors
-
Cerebrospinal fluid (CSF) leak closure
-
Orbital decompression (eg, Graves ophthalmopathy)
-
Optic nerve decompression
-
Dacryocystorhinostomy (DCR)
-
Choanal atresia repair
-
Foreign body removal
-
Epistaxis control
Typically, endoscopic sinus surgery is reserved for patients with documented rhinosinusitis, based on a thorough history and a complete physical examination, including CT scans if appropriate, and in whom appropriate medical treatment has failed.
Medical therapy alone may be inadequate for treatment of nasal polyposis. Aukema et al found that although 12 weeks of treatment with fluticasone propionate nasal drops reduced the need for sinus surgery in patients with nasal polyposis and chronic rhinosinusitis, 14 of 27 patients still required surgery. [7] Similarly, antrochoanal polyps require surgical removal.
Nasal masses
Increasingly, selected nasal masses and tumors are being removed endoscopically. Endoscopic removal of inverted papilloma is controversial. Endoscopic surgery can be performed for limited lesions in which definitive control and margins can be obtained endoscopically; this circumstance can be predicted preoperatively via nasal endoscopy and imaging.
More extensive lesions should be approached externally; either a lateral rhinotomy method or a midfacial degloving method can be used for en bloc tumor removal. Further research with long-term monitoring in this area will better delineate the optimal treatment for these patients.
Cerebrospinal fluid leaks
CSF leaks associated with CSF rhinorrhea can be managed endoscopically. Success rates of 80% have been reported in the literature with primary endoscopic attempts; success rates increase to 90% if revision endoscopic closures are included.
With endoscopic repair of CSF leaks, the more extensive neurosurgical external approaches via craniotomy can be avoided. In certain clinical settings, endonasal encephaloceles are repaired via endoscopic approaches.
Ophthalmic procedures
Endoscopic approaches may also be applied for ophthalmic procedures, including orbital decompression, endoscopic DCR, and optic nerve decompression for traumatic indirect optic neuropathy. Traditionally, these procedures were performed through external approaches, but as clinical experience in nasal endoscopic techniques has increased, they are now performed endoscopically. Only surgeons with extensive training in, and expertise with, endoscopic techniques should perform these procedures.
Contraindications to Endoscopic Sinus Surgery
Certain sinus conditions may not respond completely to endoscopic treatment; these include intraorbital complications of acute sinusitis, such as orbital abscess or frontal osteomyelitis with Potts puffy tumor. An open approach, with or without additional endoscopic assistance, may be preferable in these instances. A careful review of preoperative CT or magnetic resonance imaging (MRI) scans helps guide the surgeon.
After 2 failures to endoscopically manage CSF leaks associated with CSF rhinorrhea, patients should be referred to a neurosurgeon for closure using a neurosurgical approach. Likewise, after failure to endoscopically manage frontal sinus disease, open approaches should be considered.
Clinical Evaluation
The cornerstone of accurate diagnosis and treatment of chronic sinusitis is a thorough history and a complete physical examination, including nasal endoscopy. Surgery should not be considered unless the evaluation clearly identifies chronic sinusitis as the cause of the patient's constellation of symptoms.
The history should elucidate the frequency of infections, the type and the duration of symptoms, and the response to medical therapy. Patients with chronic or recurrent symptoms typically report the following symptoms:
-
Nasal congestion
-
Purulent drainage
-
Postnasal drip
-
Facial pressure and headache
-
Hyposmia or anosmia
-
Nasal obstruction
However, other conditions can mimic chronic sinusitis, causing 1 or more of the above symptoms. Therefore, ruling out other etiologies for the patient's symptoms is imperative. For example, patients with allergic rhinitis may have similar problems, such as sneezing, watery eyes, itchy eyes, nasal congestion, and postnasal drip. If the patient's only problem is allergic rhinitis, then endoscopic sinus surgery is not the solution, and proper medical treatment should be prescribed.
A physical examination is an excellent adjunct to patient history in diagnosing or excluding chronic sinusitis. A complete head and neck examination, along with anterior rhinoscopy, should be performed. If further nasal examination is required, a full nasal endoscopy should be carried out. The patient should be assessed for the following conditions:
-
Septal deviation
-
Turbinate hypertrophy
-
Nasal polyps
-
Nasal airway problems, including dynamic internal or external valve collapse
-
Ostiomeatal complex, if visible
-
Adenoidal hypertrophy
Rigid nasal endoscopy with mild septal deviation is depicted in the videos below.
Percussion of the sinuses to elicit tenderness may provide additional information; however, this is an imperfect technique in terms of sensitivity and specificity.
Patients with suspicious findings on history and physical examination should undergo computed tomography (CT) scanning. In patients with normal findings on paranasal sinus CT scans and no change in symptoms after undergoing medical treatment, a diagnosis of chronic sinusitis is suspect at best. These patients should not be offered functional endoscopic sinus surgery as a treatment for their symptoms.
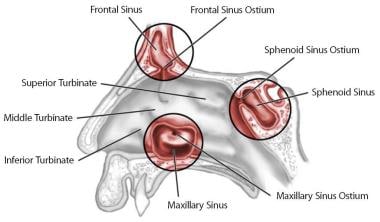
Relevant Anatomy
Intimate knowledge and understanding of the anatomy of the lateral nasal wall and the sinuses (see the image below), in conjunction with a careful preoperative review of CT scans, are paramount in the safe and complete performance of endoscopic sinus surgery. The following description of endonasal anatomy is roughly based on the order of dissection during nasal endoscopy and surgery.
Nasal septum and inferior turbinate
Immediately upon entering the nasal cavity, the first structures encountered are the nasal septum and the inferior turbinate. The nasal septum consists of the quadrangular cartilage anteriorly, extending to the perpendicular plate of the ethmoid bone posterosuperiorly and the vomer posteroinferiorly.
Recognizing deflections of the nasal septum preoperatively is important because they may significantly contribute to nasal obstruction and limit endoscopic visualization during surgery. As appropriate, patients with septum deflections may be counseled regarding the need for septoplasty in conjunction with functional endoscopic sinus surgery.
The inferior turbinate extends along the inferior lateral nasal wall posteriorly toward the nasopharynx. In patients with a significant allergic component to their problems, the inferior turbinates may be edematous. These patients may benefit from a turbinate reduction at the same time as the endoscopic sinus surgery. The inferior meatus, where the nasolacrimal duct opens, is located approximately 1 cm beyond the most anterior edge of the inferior turbinate.
Middle turbinate
As the endoscope is further advanced into the nose, the next structure encountered is the middle turbinate. The middle turbinate is a key landmark in endoscopic sinus surgery. It has a vertical component (lying in the sagittal plane, running from posterior to anterior) and a horizontal component (lying in the coronal plane, running from medial to lateral).
Superiorly, the middle turbinate attaches to the skull base at the cribriform plate. As such, care should always be taken when manipulating the middle turbinate.
The horizontal component of the middle turbinate is referred to as the basal (or grand) lamella, and it represents the dividing point between anterior and posterior ethmoid air cells. Posteriorly and inferiorly, the middle turbinate attaches to the lateral nasal wall at the crista ethmoidalis, just anterior to the sphenopalatine foramen.
Uncinate process
The uncinate process is the next key structure to be identified in endoscopic sinus surgery. This L-shaped bone of the lateral nasal wall forms the anterior border of the hiatus semilunaris, or the infundibulum. The infundibulum is the location of the ostiomeatal complex, where the natural ostium of the maxillary sinus opens.
For patients with sinus disease, a patent ostiomeatal complex is critical for improvement of symptoms. Anteriorly, the uncinate process attaches to the lacrimal bone, and inferiorly, the uncinate process attaches to the ethmoidal process of the inferior turbinate.
Natural maxillary ostium
Once the uncinate process is removed, the natural maxillary ostium can be seen, typically just posterior to the uncinate process, roughly one third of the distance along the middle turbinate from its anterior edge. It lies at approximately the level of the inferior border of the middle turbinate, superior to the inferior turbinate.
The natural maxillary ostium is the destination for the mucociliary flow within the maxillary sinus. Therefore, for optimal results, the surgically enlarged maxillary antrostomy must include the natural ostium. In fact, failure to include the maxillary ostium in endoscopic surgical antrostomy is one of the key patterns of failure in functional endoscopic sinus surgery.
The maxillary sinus, approximately 14-15 mL in volume, is bordered superiorly by the inferior orbital wall, medially by the lateral nasal wall, and inferiorly by the alveolar portion of the maxillary bone.
Ethmoid bulla
The next structure to be encountered is the ethmoid bulla, which is one of the most constant anterior ethmoidal air cells. It is just beyond the natural ostium of the maxillary sinus and forms the posterior border of the hiatus semilunaris.
The lateral extent of the bulla is the lamina papyracea. Superiorly, the ethmoid bulla may extend all the way to the ethmoid roof (the skull base). Alternatively, a suprabullar recess may exist above the roof of the bulla. A careful preoperative review of the patient's CT scan clarifies this relationship.
Ethmoid sinus
The ethmoid sinus consists of a variable number (typically 7-15) of air cells. The most lateral border of these air cells is the lamina papyracea, and the most superior border of these cells is the skull base. Supraorbital ethmoid cells may be present. A review of the patient's CT scan alerts the surgeon to these variations.
The basal lamella of the middle turbinate separates the anterior ethmoid cells from the posterior ethmoid cells. Anterior ethmoid cells drain to the middle meatus, and the posterior cells drain into the superior meatus.
Sphenoid sinus
Exenteration of the posterior ethmoid cells exposes the face of the sphenoid. The sphenoid sinus is the most posterior of the paranasal sinuses, sitting just superior to the nasopharynx and just anterior and inferior to the sella turcica. The anterior face of the sphenoid sits approximately 7 cm from the nasal sill on a 30° axis from the horizontal.
Several important structures are related to the sphenoid sinus. The internal carotid artery is typically the most posterior and medial impression seen within the sphenoid sinus. In approximately 7% of cases, the bone is dehiscent.
The optic nerve and its bony encasement produce an anterosuperior indentation within the roof of the sphenoid sinus. In 4% of cases, the bone surrounding the optic nerve is dehiscent. Therefore, controlled opening of the sphenoid sinus, typically at its natural ostium, is critical for a safe outcome.
The location of the natural ostium of the sphenoid sinus is variable. In approximately 60% of people, the ostium is located medial to the superior turbinate, and in 40%, it is located lateral to the superior turbinate.
Frontal recess
The frontal recess, or the frontal sinus outflow tract, is the tract that leads from the frontal sinus into the nasal cavity. Often, the ethmoid bulla is the posterior border of the frontal sinus outflow tract.
Anteriorly, the frontal sinus outflow tract is bordered by the uncinate process or the agger nasi cells (frontal anterior ethmoid air cells). If any of these cells are enlarged or if scarring is present from a previous surgery, resultant outflow tract obstruction, leading to frontal sinusitis, may occur. Typically, the medial wall of the frontal recess is formed by the lamina papyracea.
For more information about the relevant anatomy, see Paranasal Sinus Anatomy, Nasal Anatomy, and Skull Base Anatomy.
Preparation
Anesthesia for Endoscopic Sinus Surgery
Patients may undergo functional endoscopic sinus surgery under intravenous sedation and local anesthesia or under general anesthesia. The authors' institutional preference is general anesthesia.
Technique
Overview of Endoscopic Sinus Surgery
The procedure begins with decongestion of the nose and infiltration of lidocaine with epinephrine (1% lidocaine with 1:100,000 epinephrine is used for injection). The lateral nasal wall near the uncinate process is injected. Using a 3-mL syringe while placing a slight bend to the 27-gauge needle facilitates the injection.
Next, the superior inlet and the anterior face of the middle turbinate are injected submucosally. If the possibility of septoplasty exists, the septum should also be injected.
Next, 4 mL of 4% cocaine is placed onto pledgets, which are placed bilaterally in the nares. A throat pack may be placed, or alternatively, the stomach may be suctioned prior to extubation upon completion of the procedure.
The patient is then draped for surgery. If image-guided surgery is to be used, the appropriate headset apparatus should be applied at this time.
Endoscopic Uncinectomy
Functional endoscopic sinus surgery may begin with uncinectomy. If the uncinate process can be initially visualized without manipulating the middle turbinate, uncinectomy can be performed directly. Otherwise, the middle turbinate is gently medialized, carefully using the curved portion of the Freer elevator to avoid mucosal injury to the turbinate and to avoid forceful medialization and fracture of the turbinate.
Next, uncinectomy may be performed via an incision with either the sharp end of the Freer elevator or a sickle knife. The incision should be placed at the most anterior portion of the uncinate process, which is softer on palpation in comparison to the firmer lacrimal bone, where the nasolacrimal duct is located. Then, a Blakesley forceps is used to grasp the free uncinate edge and to remove it.
Complete uncinectomy is important for subsequent visualization. Incomplete uncinectomy is a common reason for failure with primary surgery. The backbiter may also be directly used to take down the uncinate process.
Maxillary Antrostomy/Ethmoidectomy
Once the uncinate process is taken down, the true natural ostium of the maxillary sinus should be identified. The protected eye may be palpated at this juncture to ensure that there is no dehiscence of the lamina papyracea and to confirm the location of the lamina. The natural ostium is typically at the level of the inferior edge of the middle turbinate about one third of the way back.
A true cutting instrument is used to circumferentially enlarge the natural ostium. The optimal diameter for the maxillary antrostomy is controversial; typically, a diameter of 1 cm allows for adequate outflow and for postoperative monitoring in the office. Care should always be taken to avoid penetrating the lamina papyracea.
Anterior Ethmoidectomy
Next, the ethmoid bulla should be identified and opened. A J-shaped curette may be used to open the bulla at its interior and medial aspect. Once the cell is entered, the bony portions may be carefully removed using a microdebrider or a true-cutting forceps. Complete resection of the lateral bulla facilitates proper visualization and dissection posteriorly. Again, care should be taken laterally to maintain an intact lamina papyracea.
The remainder of the anterior ethmoid cells may be uncapped initially with a J curette and further opened with a microdebrider or a true cutting forceps. Using a curette initially allows for tactile sensation and determination of the thickness of bone and verifies proper orientation prior to further opening of cells with powered instrumentation. Care should always be taken to avoid mucosal stripping, because mucosal preservation results in superior postoperative outcomes.
Anterior ethmoid cells should be cleared to the skull base, with the surgeon exercising caution when approaching the ethmoid roof and maintaining constant reference to the endoscopic view and to the preoperative CT scan. Image-guided surgery or computer-aided surgery also guides the surgeon as to the distance to the skull base, but it does not replace the need for an intimate knowledge of the anatomy.
While moving posteriorly to new air cells, the surgeon should always enter inferiorly and medially and then subsequently open laterally and superiorly once the more distal anatomy can be judged by visualization and palpation. Anterior ethmoidectomy is complete upon reaching the basal lamella of the middle turbinate.
If the sinus disease is limited to the anterior ethmoid cells and the maxillary sinus, the procedure may end with simple anterior ethmoidectomy and maxillary antrostomy. If, however, significant radiographic and clinical disease of the posterior ethmoid and sphenoid is present, then dissection should continue to exenterate the posterior ethmoid cells and to perform adequate sphenoidotomy as appropriate.
Posterior Ethmoidectomy
Posterior ethmoidectomy begins with perforating the basal lamella just superior and lateral to the junction of the vertical and horizontal segments of the middle turbinate. Care must be taken to preserve the posterior sagittal section of the middle turbinate and the inferior portion of the coronal segment of the basal lamella. Preserving this L-shaped strut ensures the stability of the middle turbinate. The lateral and superior portions of the basal lamella may then be removed using the microdebrider.
Further posterior ethmoid cells may be taken down in a similar fashion, keeping in mind the location of the skull base and the lamina. The surgeon must be cognizant that the skull base typically slopes inferiorly at an approximately 30° angle from anterior to posterior. Thus, the skull base lies lower posteriorly than anteriorly. This dissection is taken back to the face of the sphenoid.
Enlargement of the Natural Ostium of the Sphenoid Sinus
In the absence of Onodi cells, the sphenoid ostium lies medial and posterior to the final posterior ethmoid cell. A rough guide is that the face of the sphenoid is approximately 7 cm from the nasal sill at a 30° angle from the horizontal. Identifying the superior turbinate aids in the confirmation of position. The superior turbinate inserts on the anterior face of the sphenoid sinus.
The sphenoid sinus is entered just medial and inferior to its natural ostium with a J curette or an olive-tipped suction. Once the sinus is entered safely, the ostium can be enlarged using a mushroom punch forceps. Care must be taken not to aggressively enter the sinus because dehiscences may be present in the bony coverage of the carotid artery or the optic nerve.
Frontal Sinus Work
Frontal sinus work is typically reserved for the end of the surgical procedure because manipulation may create bleeding and obscure further posterior work. If frontal sinus work is indicated, a 45° or a 70° telescope proves useful.
Typically, an agger nasi or frontal cell is the cause of frontal outflow obstruction. Using an angled scope for visualization, a frontal sinus curette is passed above the cell and then pulled anteriorly, thus breaking posterior and superior cell walls.
Particular care must be exercised when working in the frontal recess, because the lamina and the skull base sit in immediate proximity to the outflow tract. Image-guided and navigational systems for computer-aided surgery and intimate knowledge of the anatomy are critical for safe frontal sinus work. Kuhn and Javer provide further discussion of endoscopic frontal sinus surgery. [8]
Nasal Packing and Spacer Placement
Once dissection is complete and hemostasis is achieved, a bacitracin-coated Telfa or Afrin soaked pledget is placed into the nostril. Some surgeons also place Gelfilm or a dissolvable spacer within the middle meatus to keep the space open and to prevent lateralization of the middle turbinate and synechiae formation.
Post-Procedure
Nasal packing is removed prior to discharge of the patient. The patient is discharged with saline nasal spray (eg, OCEAN Nasal Spray) and antibiotics, as well as instructions for a follow-up visit in 1 week. If a spacer was placed in the middle meatus, it should be removed or suctioned away on the first postoperative visit.
Outcome and Prognosis
Outstanding short- and long-term results have been reported for endoscopic sinus surgery. In one study, symptoms improved in 66 of 72 patients following this surgery, with a mean follow-up time of 7.8 years. [1] In another report, quality of life improved for 85% of the patient population, with a mean follow-up time of 31.7 months. [2]
Complications
All risks and benefits should be candidly discussed with patients as part of the informed consent process prior to surgery. A patient should never undergo surgery without a full discussion of all possible complications.
Risks associated with endoscopic sinus surgery are as follows:
-
Bleeding
-
Synechiae formation
-
Orbital injury
-
Diplopia
-
Orbital hematoma
-
Blindness
-
CSF leak
-
Direct brain injury
-
Nasolacrimal duct injury/epiphora
A large retrospective study of the complications associated with functional endoscopic sinus surgery found an overall complication rate of 0.50%; the rates of CSF leakage, orbital injury, hemorrhage requiring surgery, blood transfusion, and TSS were 0.09%, 0.09%, 0.10%, 0.18%, and 0.02%, respectively. [9]
-
Rigid nasal endoscopy performed in the clinic. A mild left septal deviation is seen anteriorly. The left middle turbinate and middle meatus are normal. Video courtesy of Vijay R Ramakrishnan, MD.
-
Rigid nasal endoscopy. The right side contains normal turbinates and middle meatus with a small amount of mucus in the inferior meatus. The endoscopy concludes with visualization of the soft palate, nasopharynx, and Eustachian tube orifices. Video courtesy of Vijay R Ramakrishnan, MD.
-
Lateral nasal wall anatomy and paranasal sinus ostia.