Background
Physicians and aestheticians use a variety of facial resurfacing techniques to improve the appearance of the skin by addressing skin quality, age spots, fine lines, and scarring. These techniques include traditional dermabrasion, chemical peeling, laser resurfacing, and microdermabrasion. All of these modalities exert their effects by resurfacing or ablating the skin at various depths and promoting skin healing. Microdermabrasion ablates the most superficial aspects of the skin using a high-pressure flow of crystals. The clinical results of these various skin-resurfacing techniques relate to the skin target depth desiring correction and the depth of ablation performed.
History of the Procedure
The concept of facial resurfacing dates back to 1500 BCE, when Egyptians reportedly used sandpaper to improve scars. [1] In the early 1900s, dermabrasion was developed to promote skin rejuvenation and was modified to its modern form in the 1950s. Dermabrasion involves ablating the skin to the level of the dermis to promote skin regrowth. Based on the power dental equipment design, the dermabrasion machine uses a wire brush with a diamond fraise to mechanically ablate the skin. Local anesthesia is required to perform the dermabrasion procedure. The technique is operator dependent, and, thus, highly skilled surgical technique is required to obtain optimal results. Reported complications include excessive bleeding, infection, scarring, and hypopigmentation. Furthermore, healing usually takes up to 7-10 days, owing to the deep dermal damage.
Microdermabrasion was designed by Marini and Lo Brutto in Italy in 1985 and addressed some of the adverse effects inherent with dermabrasion. [2] Advantages included ease of use, painless nature with minimal complications, minimal inconvenience to the patient, and proposed overall effectiveness. Monteleone presented the clinical effectiveness of this new technique at the Third Meeting of the Southern Italy Plastic Surgery Association in 1988.
The technique spread throughout Europe during the late 1980s and mid 1990s, until eventually Mattoli Engineering introduced microdermabrasion to the US market in 1996. [3] Microdermabrasion quickly gained widespread popularity, owing to its low risk, rapid recovery time for patients, and apparent results.
Problem
Most skin resurfacing techniques demonstrate clinical efficacy, but also carry the potential for serious complications such as pigmentary changes and scarring. These complications are related to the depth of skin abrasion obtained.
The advantages of microdermabrasion are also related to the superficial skin disruption that results from the procedure, which leads to an overall painless procedure that does not require anesthesia, is relatively simple and quick to perform, can be repeated at short intervals, and does not significantly interrupt the patient’s life. Since microdermabrasion produces a superficial ablation primarily limited to the epidermis, it is mainly effective for fine lines and superficial scars
Limitations of the procedure include a clinical effectiveness limited to more superficial issues and the need for multiple treatments to achieve clinical results. It is ineffective for deeper wrinkles or scars that extend beyond the epidermis.
Relevant Anatomy
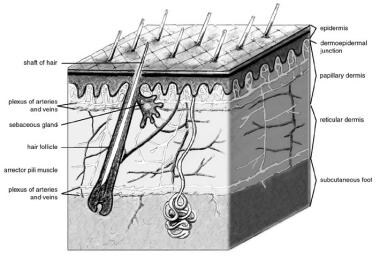
The skin is functionally divided into two layers—the epidermis and the dermis. [4]
Epidermis
Overall, the epidermis replaces itself every 12-14 days. The epidermis is composed of epithelium and can be further subdivided into the following five layers:
-
Stratum corneum
-
Stratum lucidum
-
Stratum granulosum
-
Stratum spinosum
-
Stratum basale
The most superficial later is the stratum corneum, which is composed of multiple layers of keratinocytes that are constantly sloughed and regenerated. This is the layer that provides the major barrier function and is targeted during mechanical exfoliation.
The stratum lucidum is found mainly in the palms of the hands and soles of the feet and contains a dense layer of keratin filaments that provides additional structural support. The stratum granulosum contains granules containing a lipid rich content that creates a waterproof barrier for the skin. The stratum spinosum is the thickest layer of the epidermis and contains multiple polygonal spiny cells rich in cytokeratin and with desmosomal intercellular connections. Langerhans cells, dendritic cells, and other immunomodulating cells are located throughout this layer.
The stratum basale contains one to three layers of cuboidal or columnar cells that are mitotically active and generate the cells that comprise the other layers of the epidermis. Melanocytes and Merkel cells can also be found within this layer.
See the image below.
Dermis
The dermis forms two layers and is composed of connective tissue—the papillary layer and the reticular layer. The loose papillary layer is located beneath the epidermal stratum basale and contains the capillary network that supplies the skin and the nerve endings responsible for touch sensation. The thicker reticular layer is composed of densely packed collagen that is responsible for the skin’s tensile strength. This layer also serves as the foundation for hair follicles, sweat glands, and sebaceous glands, and it contains the dermal plexus.
Collagen is the main structural component of the dermis. Type I collagen constitutes 80% of dermal collagen and imparts tensile strength. Type III collagen comprises 15% of dermal collagen. It is found throughout the dermis and primarily serves to anchor the epidermis to the dermis. Elastic fibers comprise about 3% of the dermis and provide elasticity and resilience. Ground substance is an amorphous gel-like material that surrounds cells and imparts turgidity and resilience.
The dermis is bound tightly to the epidermis by the dermoepidermal junction, which is the interface between the epidermis and the papillary dermis. The basal layer keratinocytes and dermal fibroblasts produce the components that characterize the dermoepidermal junction, such as anchoring fibrils that bridge the basal epidermal layer and papillary dermis. Beneath the dermis lies the subcutaneous fat, which derives its blood supply from arteries and veins located in the fibrous septa.
Etiology of Aging
Skin quality and appearance are affected by a variety of external and internal factors, which subsequently lead to skin conditions such as aging, photoaging, enlarged pores, and scarring. A distinction can be made between the changes in the skin that occur as a result of chronological aging and photoaging.
Chronological aging, or intrinsic aging, is the irreversible and progressive loss of homeostatic capacity and is assumed to be a genetically programmed phenomenon.
Photoaging results in changes in gene expression and results from exposure to ultraviolet radiation. Ultraviolet (UV) radiation consists of UVA, UVB, and UVC light.
Short-wavelength UVC light is the most damaging type of radiation; however, it is filtered by the atmosphere and does not reach the earth’s surface. Thus, UVB light and UVA light are mostly responsible for tanning and aging. Upon contact with the skin, some light is scattered and reflected by the stratum corneum, while other light is absorbed into the epidermis.
UVB light is shorter in wavelength (320-290 nm) and less able to penetrate the skin
It is mostly absorbed by the epidermis and only about 10% penetrates the deeper layers of the skin. This radiation is responsible for delayed tanning, burning, skin aging, and promoting the development of skin cancer. [5]
UVA light has a longer wavelength (400-320 nm) and is more able to penetrate the skin. UVA radiation accounts for about 95% of the UV radiation that reaches the earth’s surface. About 50% of UVA light penetrates the epidermis and reaches the papillary dermis. It is responsible for the immediate tanning effect, and it also contributes to skin aging. [5] Most of the immediate and long-term effects of photodamage occur in the epidermis and dermis.
Pathophysiology
The process of skin aging can be divided into intrinsic aging and photoaging. [6] Chronologic aging is skin damage resulting from the passage of time, whereas photoaging is damage resulting from exposure to UV radiation. These are two distinct processes. Clinically, naturally aged skin appears smooth, pale, and finely wrinkled. On the other hand, photoaged skin is coarsely wrinkled and associated with dyspigmentation and telangiectasias. [6] The most apparent differences between these two processes are evident in the dermis.
Chronological aging affects all the layers of the face including the bone, ligaments, fat, and skin in the upper middle and lower portions on the face. [7] Clinically, this results in bony resorption and reduction of facial skeletal support, atrophy of subcutaneous fat and volume loss, attenuation of the musculofibrous system, and gravity-induced soft-tissue redistribution. Alterations of the skin surface include thinning of the epidermis and dermis and loss of elasticity. Photoaging from chronic UV radiation exposure causes degenerative changes in the skin that are superimposed onto the normal chronological aging process.
As the skin ages, the structural stability of the dermis is compromised by the overall degradation of collagen. [7] Collagen is the major insoluble fibrous protein in connective tissue and is the major component of the dermis. Its major function is to provide tissue with the ability to withstand stretching. Type I and type III collagen predominate. [8]
In young, healthy skin, collagen is continuously degraded by matrix metalloproteinases and resynthesized by fibroblasts and other epithelial cells. The resulting long strands of collagen formed in the dermis impart the skin with its tensile strength and stability. UV radiation is known to induce the synthesis of matrix metalloproteinases and other collagen-degrading enzymes, shifting the balance toward collagen degradation and fragmentation. In addition, collagen synthesis slows down more in photoaged skin than in naturally aged skin. [8]
The aging process continues in a cycle of sustained collagen loss. Over time, this clinically results in thinning of the epidermis, wrinkling, loss of elasticity, dyschromia, and dermal atrophy. Histologically, the aging process first begins with hyperplastic response and increase in melanin production as it reacts to environmental insults. The process then shifts to skin atrophy and melanocyte dysfunction in the later stages of aging. [9] Histologic changes in an aging dermis include solar elastosis, degradation of elastin and collagen fibers, and increased ground substance. Furthermore, DNA damage from radiation increases the risk of squamous and basal cell carcinoma.
The degree of skin wrinkling can be classified with the Glogau scale, ranging from type I to IV and corresponding to mild, moderate, advanced, and severe wrinkling, as follows [10] :
-
Type I: No wrinkles and early photoaging such as mild pigmentary changes, no keratosis, and minimal wrinkles; use of minimal or no makeup
-
Type II: Wrinkles in motion and early-to-moderate photoaging with early senile lentigines visible, keratosis that are palpable but not visible, and parallel smile lines beginning to appear lateral to the mouth; usually some foundation worn
-
Type III: Wrinkles at rest and advanced photoaging, including obvious dyschromia, visible keratosis, and wrinkles without movement; always wears foundation
-
Type IV: Only wrinkles and severe photoaging such as a yellow-gray skin tone, prior skin malignancies, and wrinkling throughout with no normal skin; photoaging precludes use of makeup because it cakes and cracks [11]
Indications
Microdermabrasion is most effective for superficial skin conditions, as it targets mainly the superficial skin layers of the skin. Superficial skin conditions include early photoaging, fine lines, superficial scarring, seborrheic skin, melasma, and reduction of pore size. [12] Deep scars, acne scars, and rhytides require a greater depth of skin injury for effective treatment.
Identifying the patient’s skin type and sun reactivity is necessary to define the risk of pigmentary changes with any procedure that wounds the skin, such a resurfacing with microdermabrasion. The Fitzpatrick classification classifies skin according to sun-reactivity and propensity for photodamage. [13]
Table. Fitzpatrick Skin Classification (Open Table in a new window)
| Type | Skin Color | Characteristics |
| I | Very white | Always burns, never tans |
| II | White | Usually burns, tans with difficulty |
| III | White or light brown | Mildly burns, average ability to tan |
| IV | Brown | Rarely burns, tans easily |
| V | Dark brown | Very rarely burns, tans very easily |
| VI | Black | Never burns, darkly pigmented |
Skin types I-III generally tolerate resurfacing procedures with minimal risk of pigmentary complications. Skin types IV-VI have a higher risk of pigmentary changes with deeper wounding, such as dyschromia, postinflammatory hyperpigmentation, and permanent hypopigmentation. Superficial wounding extends to the stratum granulosum or papillary dermis. Medium-depth wounding extends into the upper reticular dermis. Deep wounding extends to the midreticular dermis. Wounds that extend beyond this level can cause scarring, regardless of the skin type. Because microdermabrasion causes only superficial wounding, it does not carry the risks of pigmentary changes or scarring seen in other techniques, such as dermabrasion, chemical peels, or laser resurfacing.
Even patients with Fitzpatrick types IV-VI who may be more at risk of pigmentary changes with other resurfacing techniques can undergo conservative microdermabrasion with relative safety, when performed by an experienced provider.
Contraindications
Contraindications include current or recent use of isotretinoin (within 6 months of treatment) owing to the potential for hypertrophic scarring. [14, 15] Facial surgery within the past 2 months, radiation therapy to the head, or a history of hypertrophic scarring anywhere on the body are also contraindications.
Any bacterial or viral infections affecting the skin—such as impetigo, flat warts, and herpes simplex—are absolute contraindications and must be controlled with systemic therapy prior to undergoing microdermabrasion, owing to the risk of autoinoculation as the handpiece is moved from the affected region to unaffected skin. [16] Some authors propose that antiviral prophylaxis should be given to patients with a history of recurrent herpes labialis. [1]
Relative contraindications include the presence of rosacea and telangiectasias since these may be exacerbated by the treatment. [1]
-
Anatomy of the skin.