Practice Essentials
Although a review of the literature contains numerous reports on the subject of pediatric thyroid carcinoma, the low incidence and subsequent lack of prospective randomized trials make drawing absolute conclusions regarding the definitive workup, management, and treatment of this disease difficult. In 2015, however, a task force commissioned by the American Thyroid Association (ATA), following an extensive literature search, issued the first guidelines on the management of pediatric thyroid nodules and differentiated thyroid cancer. [1, 2, 3]
A detailed understanding of how to perform a comprehensive evaluation of the pediatric thyroid nodule and persistent cervical adenopathy is necessary in order to establish the diagnosis of pediatric thyroid cancer. Based on retrospective series, the prevalence of thyroid nodules in children ranges from 0.2-5%, compared with approximately 30% in adults. However, pediatric thyroid nodules carry a far greater risk of harboring malignancy compared with adults, at approximately 26.4%. Some authors have reported an incidence of as high as 36%. [4] Because pediatric thyroid nodules carry this increased risk of malignancy, physicians should perform an expeditious workup. [5, 6]
Signs and symptoms of pediatric thyroid cancer
Thyroid carcinoma in pediatric patients usually manifests as an asymptomatic neck mass, with a reported incidence of cervical lymphadenopathy ranging from 35-83%. [7] The neck masses are typically discovered incidentally by parents or patients or by physicians during routine physical examination. Focal fold paralysis in children with thyroid malignancy is much less common than in adults with thyroid malignancy. [8]
Additionally, unlike adults, young patients with thyroid nodules often do not report pain, tenderness, compression of the respiratory tract, problems with swallowing, or inappropriate fixation of the neck. Even young patients who have lung metastases usually do not report pulmonary symptoms. [9] However, 10-20% of patients present with distant metastasis (most commonly to the lungs), and 70% of patients present with extensive regional nodal involvement. [10]
Workup
The recommended diagnostic protocol of thyroid nodules consists of the following steps:
Child's history, including familial history and radiation exposure
Clinical examination
Laboratory tests
Thyroid ultrasonography
Fine-needle aspiration biopsy (FNAB)
The beneficial role of scintigraphy is limited. [11, 9] However, molecular marker analysis of FNAB samples is proving to be beneficial in determining surgical plans.
Most childhood thyroid nodules are asymptomatic and are detected by parents or by physicians during routine examination. Only about 50% of children with thyroid carcinoma present with nodular thyroid enlargement as the presenting symptom. Follicular adenoma is the most common cause of solitary thyroid nodules in the pediatric population; however, solitary nodules in children reportedly have a 20-73% incidence of malignancy. [12, 13, 14] A painless noninflammatory metastatic cervical mass is the presenting symptom in 40-80% of patients. [15] Malignant lesions are usually papillary and follicular carcinomas. Radiation exposure, which is still used either as therapy prior to bone marrow transplantation or as a treatment of Hodgkin disease, remains a major risk factor. [16]
The subsequent diagnostic workup is aimed at determining whether the lesion represents a malignancy. Collected data can be useful in preoperative planning if surgery is indicated. Pediatric and adult thyroid cancers have differing biological behaviors. Despite the fact that pediatric thyroid cancer usually presents at an advanced stage, it carries an excellent prognosis, with long-term survival rates greater than 95%.
An image depicting thyroid cancer can be seen below.
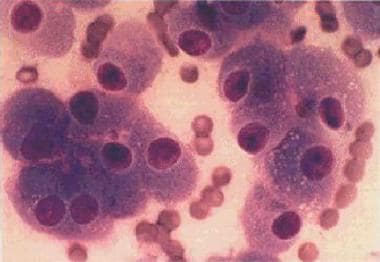 A monomorphous cell population of Hürthle cells arranged in loosely cohesive clusters and single cells. The cells are polyhedral and have abundant granular cytoplasm with well-defined cell borders. The nuclei are enlarged and have a central prominent macronucleolus.
A monomorphous cell population of Hürthle cells arranged in loosely cohesive clusters and single cells. The cells are polyhedral and have abundant granular cytoplasm with well-defined cell borders. The nuclei are enlarged and have a central prominent macronucleolus.
Management
Radioactive therapy with iodine 131 (131I) is indicated to ablate residual normal thyroid and to treat functioning metastases in differentiated thyroid tumors. Because pediatric patients are few and the prognosis is generally excellent, 131I is usually recommended only for patients with extensive unresectable cervical nodal involvement, invasion of vital structures, or distant metastases. Very few instances of solid tumors or leukemia associated with 131I treatment have been reported. [17]
Treatment for thyroid malignancy is primarily surgical. Because of the unusual combination of an excellent prognosis and an advanced-stage disease presentation, the initial extent of surgery is controversial. Some recommend that the initial surgical approach be conservative, while others advocate aggressive management with total thyroidectomy and radioactive iodine (RAI) for all patients. The relative infrequency of thyroid malignancy makes this controversy difficult to resolve.
Thyroid lobectomy is the initial procedure of choice for most solitary thyroid lesions. The need for total versus near-total or subtotal thyroidectomy is controversial. Proponents for near-total or subtotal thyroidectomy believe that these procedures decrease the incidence of complications such as recurrent nerve injury and parathyroid devascularization, although the need to identify and preserve these structures remains. [18]
Although total thyroidectomy has not been proven to decrease recurrence, supporters of this method argue that remaining thyroid tissue may interfere with the use of radioactive iodine (RAI) in the postoperative diagnostic scanning and in the treatment of microscopic regional and distant disease. Total thyroidectomy and central neck dissection are indicated for biopsy-proven medullary carcinoma.
Selective ipsilateral neck dissection in pediatric thyroid surgery is indicated for proven or suspected regional lymph node metastasis.
Guidelines
As mentioned, in 2015 the American Thyroid Association (ATA) issued guidelines for the management of children with thyroid nodules and differentiated thyroid cancer. The guidelines’ 34 recommendations include the following, which have a recommendation rating of A [1, 2] :
-
For pediatric patients with a suppressed thyroid-stimulating hormone (TSH) associated with a thyroid nodule, thyroid scintigraphy should be pursued
-
A comprehensive neck ultrasonogram to interrogate all regions of the neck is required in order to optimize the preoperative surgical plan in children with a newly diagnosed papillary thyroid cancer
-
For the majority of children with papillary thyroid cancer, total thyroidectomy is recommended
-
In order to facilitate 131I uptake by residual iodine-avid cancer, the TSH should be above 30 mIU/L
-
Neck ultrasonography is recommended in the follow-up of children with papillary thyroid cancer; it should be performed at least 6 months after initial surgery and then at 6-12 month intervals for ATA pediatric intermediate- and high-risk patients and at annual intervals for ATA pediatric low-risk patients; follow-up beyond 5 years should be individualized based on recurrence risk
Epidemiology
Frequency
United States
Thyroid cancer, the most common pediatric endocrine neoplasm, represents 3% of all pediatric malignancies and 5-5.7% of malignancies in the head and neck. Only 5% of all thyroid cancers occur in children and adolescents. [19] Thyroid nodules occur in up to 35% of the general adult population and in only 1-2% of the pediatric population. These numbers are estimated using a compilation of data from multiple reports. [16, 20, 21]
Paradoxically, despite the lower incidence of thyroid nodules in children, a pediatric thyroid nodule has a greater risk of containing or developing a malignancy. Whereas 5% of nodules in adults are malignant, in the pediatric population, the percentage of malignant nodules is 26.4%. [8] The incidence of malignancy in multinodular goiter is 1-7% and 10-25% in solitary nodules. [16] Pediatric thyroid cancer (3% prevalence) in adolescents is also associated with juvenile autoimmune thyroiditis. [22]
A study by Bernier et al found that in the United States, between 1998 and 2013, the rate of pediatric differentiated thyroid cancer significantly increased among individuals aged 0 to 19 years, rising by 4.43% per year. This increase was seen in both sexes, with the rates rising in non-Hispanic whites, non-Hispanic blacks, and Hispanics. With regard to cancer stage, the annual rate increases for localized, regional, and distant tumors were 4.06%, 5.68%, and 8.55%, respectively, with the yearly increases for tumors less than 1 cm, 1-2 cm, and over 2 cm in size being 9.46%, 6.92%, and 4.69%. Owing to the climb in large and late-stage differentiated thyroid cancer rates, the investigators suggested that improved medical surveillance cannot entirely account for the changes. [23]
Using the US Cancer Statistics database, a study by Siegel et al found that in the United States, the overall incidence of pediatric thyroid carcinoma increased between 2003 and 2019, the average annual percentage change (AAPC) being 4.2%. In adolescents (ages 15-19 years), thyroid carcinoma was one of the most common of the International Classification of Childhood Cancer (ICCC) types, with a rate of 25.9 per million people (age adjusted to the 2000 US standard population) and an AAPC of 4.5%. The investigators suggested that the rise in pediatric thyroid carcinoma may have derived from overdiagnosis in addition to an actual increase in incidence stemming from various causes (eg, environmental exposures, such as ionizing radiation). [24]
Papillary thyroid cancer is by far the common thyroid malignancy in children, constituting 83% of all pediatric thyroid malignancies. [25] Although papillary carcinoma is more aggressive in children than in adults, pediatric papillary cancer carries a much better prognosis that adult thyroid cancer. [26]
Medullary thyroid cancer (MTC), which constitutes 5% of pediatric thyroid malignancies, is usually associated with multiple endocrine neoplasia type 2 (MEN2) in the pediatric population. The inheritance pattern occurs either sporadically or as familial MTC without other associated endocrine abnormalities. MEN2 consists of MTC and pheochromocytoma and either hyperparathyroidism (2A) or mucosal neuromas (2B). MTC associated with MEN2B is more virulent and may occur and metastasize early in infancy.
International
After the Chernobyl nuclear power plant disaster, individuals living in Russia, Ukraine, and Eastern Europe were exposed to significant levels of radioactive iodines, primarily iodine 131 (131 I). This radioactivity, which is concentrated in the thyroid gland, has resulted in a substantial increase in pediatric thyroid cancer rates among this cohort of children. [27, 28]
Mortality/Morbidity
Pediatric thyroid malignancies are usually a well-differentiated papillary subtype or the papillary-follicular subtype, but all histologic types have been observed. Children commonly present with advanced disease. At presentation, 70% of patients have extensive regional nodal involvement, and 10-20% of patients have distant metastasis. [10] The lungs are the most common sites of metastasis.
Pediatric patients seem to have higher local and distant recurrence rates than adults, but they tend to respond rapidly to therapy. The prognosis for children is excellent, with mortality rates of less than 10%. [29] Benign tumors such as follicular adenomas should be considered at risk for tumor progression toward follicular thyroid carcinoma, and they must be surgically addressed. [8]
A retrospective study by Gruszczynski et al found that although 2- and 5-year overall and disease-specific survival in pediatric thyroid cancer was close to 100% in the report’s patients, various factors, including male sex, non-Caucasian race, poverty, and language isolation, were associated with worse overall survival in these persons. Moreover, male and Black pediatric patients were more likely to present with a higher overall American Joint Committee on Cancer (AJCC) stage. [30]
Sex
Thyroid carcinoma is 2-3 times more common in females. [31]
The gender distribution of thyroid carcinoma differs between adults and children. Thyroid cancer is 4 times as common in women as in men. This difference is not seen in individuals younger than 15 years; the girl-boy ratio is as low as 1.5:1. However, in individuals aged 15–20 years, the female-to-male ratio is 3:1. [32] This implies that female sex hormones, especially during puberty, play a significant yet still undefined role in the increased incidence of thyroid cancer in females. [19]
Age
Age is a major determinant of both the incidence and recurrence of pediatric thyroid carcinoma. Pediatric thyroid carcinoma occurs more frequently in adolescents, although it has been reported in the neonatal period. [33] In children younger than 10 years, identified thyroid lesions are more likely to be malignant. [34] Children younger than 10 years are also more likely to have recurrent cancer. [29]
-
A monomorphous cell population of Hürthle cells arranged in loosely cohesive clusters and single cells. The cells are polyhedral and have abundant granular cytoplasm with well-defined cell borders. The nuclei are enlarged and have a central prominent macronucleolus.









