Practice Essentials
Environmental noise is a common and preventable cause of hearing loss in industrialized societies. Hearing loss that is caused by the noise exposure due to recreational or nonoccupational activities is termed socioacusis. Hearing loss due to injurious noise at workplace is referred to as occupational noise-induced hearing loss (ONIHL). The term acoustic trauma means the hearing loss due to single exposure to intense sound.
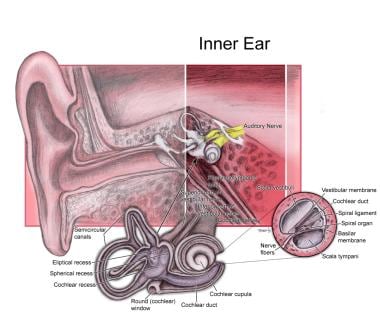
ONIHL is a more common cause of noise-induced hearing loss (NIHL) and much more serious problem than socioacusis for the following 2 reasons: (1) The threat of loss of employment may convince people to remain in environments with noise levels higher than they would otherwise accept, and (2) in the workplace, high levels of noise may be sustained on a regular basis for many hours each day over many years. Consequently, occupational noise exposure has drawn the most attention and is the best studied. [1] See the image below.
Controversy exists regarding what percentage of age-related hearing loss (presbycusis) is a consequence of a lifetime socioacusis and what percentage is solely due to the physiologic aging process.
Sustained exposure to loud noise is associated with adverse consequences other than hearing loss. For instance, sustained exposure to unwanted loud noise is annoying. Homberg has noted that unwanted noise at any level is annoying; at 72 dB, 100% of subjects rated unwanted noise as either "somewhat annoying" or "rather annoying." Even with hearing protection, Melamed reported that 60% of workers rated high levels of unwanted background noise as "highly annoying." [2]
Dornie and Laakssonen have investigated the impact of the annoying quality of noise exposure. The annoying quality of loud noise may serve as a warning that it is adversely affecting health, ie, injuring the auditory system. Moreover, the annoying quality of noise reduces processing capacity, thereby increasing the cost of performing a given task. Bhatia reported that individuals who are sensitive to noise show decreased efficacy on multiplication tasks in the presence of unwanted background noise.
Melamed et al have also shown that chronic noise exposure increases fatigue symptoms and postwork irritability. [2] They found that, after the workday was over, these fatigue symptoms and postwork irritability made relaxing and being able to unwind extremely difficult. Noise protection that attenuated the unwanted background noise by 30-33 dB for 7 days produced significant improvement in irritability and fatigue symptoms. Furthermore, urinary cortisol secretion was shown to increase with unwanted background noise. The increased urinary cortisol levels decreased toward normal after 7 days of noise attenuation.
Simply measuring the physical intensity of the stimulus as a sound pressure level cannot assess the potentially damaging effect of noise. The human ear does not respond equally to all frequencies—high frequencies are much more damaging than low frequencies at the same physical intensity levels. Consequently, most sound level meters are equipped with a filter that is designed to de-emphasize the physical contribution from frequencies to which the human ear is less sensitive. This filter is referred to as the A filter, and measurements taken using the A filter are reported as dBA. This is known as the A level on a sound pressure meter.
Signs and symptoms of noise-induced hearing loss
In occupational NIHL, which is almost always bilateral, loss is always greater at the frequencies 3000-6000 Hz than at 500-2000 Hz. Loss is usually greatest at 4000 Hz. The 4000-Hz notch is often preserved even in advanced stages.
When NIHL is limited to the high frequencies, individuals are unlikely to have difficulty in quiet conversational situations. The first difficulty the patient usually notices is trouble understanding speech when a high level of ambient background noise is present. As NIHL progresses, individuals may have difficulty understanding high-pitched voices (eg, women's, children's) even in quiet conversational situations.
Many patients experience tinnitus associated with both temporary threshold shift (TTS) and permanent threshold shift (PTS).
Workup in noise-induced hearing loss
Audiometric testing is the only diagnostic evaluation relevant to the diagnosis of NIHL. Pure-tone audiometry at the usual octave intervals should be performed. The interoctave interval of 3000 Hz should always be included as well; 3000 Hz is a sensitive area for NIHL and is a frequency that contributes significantly to speech understanding. The speech reception threshold (SRT) should also be measured for each ear.
Objective tests of hearing threshold have been used to obtain accurate hearing thresholds in individuals suspected of exaggerating their hearing loss. Cortical evoked response audiometry (CERA) is the most valuable objective test.
Management of noise-induced hearing loss
No well-recognized and scientifically validated treatments are specifically directed to NIHL. The following treatable conditions have been alleged to exacerbate NIHL by some authors, and appropriate management of these may influence the development or progression of NIHL.
-
Smoking
-
Cardiovascular disease
-
Diabetes mellitus
-
Hyperlipidemia
-
Exposure to ototoxic drugs
Pathophysiology
When animals exposed to impulse noise are examined, anatomic changes that range from distorted stereocilia of the inner and outer hair cells to complete absence of the organ of Corti and rupture of the Reissner membrane are found. Generally, no changes are found in the blood vessels, spiral ligament, or limbus. A few minutes after exposure to impulse noise, edema of the stria vascularis appears and may persist for several days.
A cochlear inflammatory response is also initiated in response to acoustic trauma and involves the recruitment of circulating leukocytes to the inner ear. [3]
Outer hair cells are more susceptible to noise exposure than inner hair cells. Temporary threshold shifts (TTS; see History) are anatomically correlated with decreased stiffness of the stereocilia of outer hair cells. The stereocilia become disarrayed and floppy. Presumably, in such a state they respond poorly. At a minimum, permanent threshold shifts (PTS; see History) are associated with fusion of adjacent stereocilia and loss of stereocilia. With more severe exposure, injury can proceed from a loss of adjacent supporting cells to complete disruption of the organ of Corti. Histopathologically, the primary site of injury appears to be the rootlets that connect the stereocilia to the top of the hair cell. With loss of stereocilia, hair cells die. Death of the sensory cell can lead to progressive Wallerian degeneration and loss of primary auditory nerve fibers.
NIHL and hair cell loss are known to show only moderate correlation because NIHL may reflect not only the sum of dead hair cells but also impaired, but still living, hair cells. High-frequency hair cells in rat cochlea may die relatively rapidly after injury, indicating a linear relation between them, but the low-frequency hair cells may survive without auditory function.
Two general theories have been advanced to account for the mechanism of injury. NIHL from constant noise exposure may be secondary to accumulated microtrauma and have a similar mechanism to injury produced from impulse noise. On the other hand, TTS may be due to metabolic exhaustion. Consequently, TTS is sometimes referred as auditory fatigue. Metabolic exhaustion sustained for prolonged periods may be so profound as to result in cell death. The concept of auditory fatigue as an explanation for TTS (with an opportunity for recovery if the noxious acoustic stimulus is removed) may account for the well-described clinical fact that intermittent noise is much less likely to produce permanent injury than continuous noise at the same intensity level.
Apoptosis (programmed cell death) was observed in noise-exposed cochlea. [4] An Src–protein tyrosine kinase (PTK) signaling cascade may be involved in both the metabolic and mechanically induced initiation of apoptosis in the sensory cells of cochlea. They may also be activated in outer hair cells following noise exposure. This knowledge, obtained from studies on chinchillas, has led to trials with Src-PTK inhibitors such as KXI-004, KXI-005, and KXI-174 by placing them on round window membrane and noting its beneficial effect in the prevention of NIHL. This may eventually lead to the development of more effective drugs for the prevention of NIHL.
A study on the fate of outer hair cells after acoustic or ototoxic insults showed that outer hair cell remains are phagocytosed by supporting cells within the epithelium. [5]
Evidence is available to support both the theory of metabolic exhaustion and the theory of mechanical trauma. Experimental animal studies have shown decreased endolymphatic oxygen tension directly related to the duration of intensity of noise exposure. Decreases in succinic dehydrogenase and glycogen content have been observed. However, mechanical models are more compatible with the observation that the greatest area of injury in occupational NIHL appears to be to that portion of a cochlea sensitive to frequencies of about 4000 cycles per second (Hz).
Recent work has clearly demonstrated the presence of glucocorticoid signaling pathways in the cochlea and their protective roles against noise-induced hearing loss. Therefore, taking advantage of current molecular and pharmacological tools to dissect the role of GC signaling in hearing loss is important. [6]
A gene association study for NIHL in 2 independent noise-exposed populations revealed that PCDH15 and MYH14 may be NIHL susceptibility genes, but further replication in independent sample sets is mandatory. [7]
The equal energy hypothesis assumed that hearing damage is a function of total acoustic energy received. That the hearing organ reacts uniformly to sounds of various intensities and duration, provided that the total sound energy remains constant, is an oversimplification and does not explain noise-induced hearing damage. A study by Pourbakht et al found that, although the total energy of intermittent sound of 125 dB noise was greater than that of continuous 115 dB sound pressure level, the latter was found to cause significantly greater PTS and hair cell loss. [8]
Hearing loss from sustained exposure to intermittent or continuous noise should be differentiated from acoustic trauma. Acoustic trauma is due to one-time brief exposures followed by immediate permanent hearing loss. The sound stimuli generally exceed 140 dB and are often sustained for less than 0.2 seconds. Acoustic trauma appears to have its pathophysiologic basis in mechanical tearing of membranes and physical disruption of cell walls with mixing of perilymph and endolymph. Damage from impulse noise appears to be a direct mechanical disruption of inner ear tissues because their elastic limit was exceeded. At high energies, acoustic trauma can result in disruption of the tympanic membrane and ossicular injury.
Much acoustic trauma is caused by impulse noise, which is usually due to blast effect and the rapid expansion of gases. Acoustic trauma is often the consequence of an explosion. Impact noise results from the collision of metals. It is highly reverberant, has both peaks and valleys, and is less likely to reach critical levels. Impact noise is more likely to be seen in the context of occupational noise exposure. It is frequency superimposed on a background of more sustained noise. Boettcher has shown that when impact noise is superimposed on continuous noise, the injurious potential is synergistically enhanced.
Animals with large PTS from an initial noise exposure showed less PTS following second noise exposure at a specific intensity compared with animals with little or no previous NIHL, indicating that these animals are less sensitive to subsequent noise exposures. However, total PTS in these ears is higher. This suggests that the major factor responsible for these results is lower effective intensity of the second noise for the ears with large initial PTS.
Other physiologic conditions that affect the likelihood and progression of NIHL have been identified. Evidence appears in the literature that decreased body temperature, increased oxygen tension, decreased free radical formation, and removal of the thyroid gland can all lessen an individual's sensitivity to NIHL. Hypoxia potentiates the noise-induced damages. Good experimental evidence shows that sustained exposure to moderately high levels of noise can reduce an individual's sensitivity to NIHL at higher levels of noise. This process is referred to as sound conditioning. It is at least superficially analogous to the protective effect a deliberate training regimen has for severe physical activity.
Epidemiology
Frequency
United States
According to the Occupational Health and Safety Administration (OSHA), 5-10 million Americans are at risk for noise-induced hearing loss (NIHL) because they are exposed to sounds louder than 85 dBA on a sustained basis in the workplace. [9] Forty-eight million Americans engage in shooting sports, the most common cause of nonoccupational NIHL (socioacusis).
A study by Carroll et al using data from the 2011-2012 National Health and Nutrition Examination Survey (NHANES) estimated that 39.4 million adults in the United States aged 20-69 years have unilateral or bilateral noise-induced hearing loss. [10]
Evaluating audiograms for 1.4 million US workers, including over 17,000 noised-exposed workers in the agriculture, forestry, fishing, and hunting (AFFH) sector, Masterson et al determined that the overall prevalence of hearing loss in the AFFH sector was actually lower than that for all industries combined (15% vs 19%, respectively). However, the hearing-loss prevalence for certain AFFH subsectors was higher than the overall percentage, being 36% for the forest nurseries and gathering of forest products sector, and 22% for timber tract operations. The AFFH subsector with the highest adjusted risk for hearing loss was aquaculture. [11]
A study by Park et al using the OSHA Information System found that between 1972 and 2019, there were 119,305 violations of OSHA noise standards involving occupational noise exposure in general industry, occupational noise exposure in construction, hearing protection in construction, and recording criteria for cases associated with occupational hearing loss. [12]
International
A literature review by Lie et al indicated that the incidence of ONIHL is decreasing in industrialized countries, most likely as a result of preventive measures, with the incidence of such hearing loss instead being highest in developing nations. [13]
Sex
More males than females are reported to have noise-induced hearing loss (NIHL). However, whether this is a consequence of greater sensitivity to NIHL in the workplace or whether it represents a higher level of exposure to nonoccupational noise is unclear.
Age
No clear-cut differences exist between young and older individuals in their susceptibility to noise-induced hearing loss (NIHL). [14]
Morbidity
A study by Deng et al indicated that in persons with occupational NIHL, risk factors for depression include longer duration of hearing loss and higher scores on the Pittsburgh Sleep Quality Index and Tinnitus Handicap Inventory. The investigators found that 84.2% of the patients with depression suffered from sleep disorders, compared with 20.4% of occupational NIHL patients without depression. Among the study’s 106 subjects, the prevalence of depressive symptoms was 53.8%. [15]
-
Anatomy of the inner ear.