Overview
Medical practitioners often encounter benign lesions of the external ear. Primary care physicians and specialists must be able to distinguish these disease processes and institute proper therapy or referral, if indicated. This article outlines several benign lesions and tumors of the external ear and gives the reader a basic understanding of their clinical features and treatment options. [1]
See the image below.
Anatomy of the External Ear
The external ear consists of the auricle and the external auditory canal (EAC).
Auricle
See the list below:
-
Tissue components
Cartilage
Elastic tissue
Skin
-
Topography
Helix
Antihelix
Tragus
Antitragus
Concha
Triangular fossa
Scaphoid fossa
Lobule
-
Musculature
Superior, anterior, and posterior auricular muscles
Innervated by seventh cranial nerve (facial nerve)
Serves to attach and support auricle
-
Blood supply
Derived from external carotid artery (postauricular and superficial temporal branches)
-
Sensory innervation
Anterior - Auriculotemporal nerve
Posterior - Great auricular nerve and lesser occipital nerve
Concha - Branches from vagus and facial nerves
-
Lymphatics
Anteriorly into parotid region
Inferiorly into superficial and deep cervical chains
Posteriorly into postauricular and occipital regions
Important in the treatment of malignant lesions, as parotidectomy and neck dissection may be necessary
External auditory canal
See the list below:
-
General anatomy
S-shaped and approximately 4 cm in length from tragus to tympanic membrane
Cartilaginous lateral third and osseous medial two thirds
-
Vasculature and lymphatics
Vasculature - Supplied by postauricular, superficial temporal, and deep auricular arteries
Lymphatics - Drain anterior (parotid gland lymph nodes), posterior, and inferior to the auricle
-
Innervation
Vagus nerve - Inferior and posterior regions of the canal
Auriculotemporal nerve - Anterior and superior
Facial nerve - Movement of auricle by the extrinsic muscles, the sensory innervation of conchal, and portions of the posterior EAC
-
Glandular structures
Sebaceous - Numerous and open into the follicles of fine vellus hairs, primarily in lateral third
Ceruminous - Variable in number, secrete cerumen into lateral third of EAC
Benign Lesions of the External Ear
Chondrodermatitis nodularis chronica helicis
Chondrodermatitis nodularis chronica helicis (CNCH; also known as the Winkler nodule) is uncommon and has a male predominance. Lesions typically present as a solitary tender erythematous nodule with central crusting or ulceration. They most commonly are located on the helical rim in men and on the antihelix and antitragus in women. Nodules are dome shaped, firm, reddish gray, and measure 3-18 mm. They appear spontaneously and reach maximum size in a short time. The lesions can last for several years and rarely regress spontaneously. [2, 3, 4] See the images below.
The etiology of CNCH remains unknown. Some authors think that it begins with some minor trauma to the ear that then incites chronic inflammation of the perichondrium, resulting in local vascular compromise. This vascular disruption then creates the observed clinical sequelae of painful nodules.
The pathophysiology of CNCH is thought to be related to the anatomy of the ear. The skin over the lateral and anterior aspect of the auricle is thin and tightly stretched over the underlying cartilage. Subcutaneous tissue is lacking in this region, which creates an area of limited vascularity. Various insults, such as trauma, frostbite, and tight-fitting headgear, can result in ischemia. This ischemia is thought to create a chronic perichondritis, which in turn leads to the clinical symptoms of pain and a nodule.
Histologic findings include dermal inflammation and fibrosis associated with either a central hyperkeratotic plug or ulceration. The cartilage is disrupted, hemorrhagic, and even necrotic.
Spontaneous resolution of CNCH has been described but is rare. Discontinuing the traumatic trigger to the ear should be employed first. [5] Surgical excision is generally considered the treatment of choice for CNCH, while observation is clearly an option. Surgical methods of treatment include curettage, electrocautery, carbon dioxide laser ablation, and excision of skin and cartilage with closure. Munnoch et al recommend a minimal skin excision combined with a more extensive cartilage resection to avoid recurrence. Healing can be hampered and infection can result if the remaining cartilage is not meticulously trimmed and smoothed in a patient with CNCH.
Current medical therapy consists of a trial of intralesional injections of 0.1-0.2 mL triamcinolone acetate (10-40 mg/mL). Nitroglycerin gel and photodynamic therapy have also been used with good results. Previously reported medical options used to treat CNCH include radiation therapy, cryotherapy, topical antibiotics, and injection of procaine hydrochloride; however, these have been abandoned because of high recurrence rates.
Patients with CNCH can expect a good prognosis, but lesions recur at the edges of the resected cartilage in as many as 10% of patients, even with wide removal of diseased cartilage.
Idiopathic cystic chondromalacia
Idiopathic cystic chondromalacia (ICC) is uncommon and generally affects men of all ages, but it most commonly is observed in the third decade of life. As its name suggests, ICC is of unknown etiology. Theories involving embryologic malformation of the auricle have been offered to explain its occurrence. During development of the external ear, the 6 hillocks of His are thought to fuse and fold around the first branchial groove. ICC is believed to originate during this fusion and folding process when potential planes and spaces are created in areas of decreased structural resistance. Cysts can occur in these potential planes and spaces of the cartilage. The other main theory to explain ICC is related to abnormal lysozymal enzyme release that causes cartilage degradation and cyst formation.
Lesions of ICC present as unilateral asymptomatic swelling on the auricle and appear in the scaphoid fossa in 80% of patients. The lesions contain viscous yellow fluid that causes slight fluctuance. Usually, no ulceration is present. Histology reveals an intracartilaginous cavity filled with granulation tissue. No epithelial lining of the cavity is observed, and the surrounding cartilage is benign.
ICC can be treated with intralesional steroids; however, the high incidence of a resulting cosmetic deformity limits use of this treatment. Simple aspiration of the cyst fluid has been tried, but re-accumulation is universal. Complete excision of the cyst can lead to significant cosmetic deformity. The most common surgical technique involves excising the anterior cyst wall followed by sclerosing the posterior cyst wall with 1% iodine solution and applying a bolster dressing postoperatively. The sclerosing creates inflammation and scarring that prevents the cyst from reforming, and the preserved posterior cartilage gives cosmetic support to the auricle. The surgeon should be careful to avoid extensive posterior cyst wall resection because floppy ear deformities can result. No significant recurrence is associated with complete excision of ICC.
A study by Ungar et al indicated that in the treatment of auricular pseudocysts (which include ICC lesions), patients who undergo incision and curettage along with deroofing, that is, excision of the anterior cyst wall, experience a recurrence rate of below 17% and good cosmetic results. As indicated above, increased recurrence rates were seen with aspiration alone. [6]
Kimura disease
Kimura disease is a rare chronic inflammatory disorder that is most commonly observed in individuals of Asian descent. According to the Armed Forces Institute of Pathology (AFIP) series, the average age of presentation is 36 years. Kimura disease has a male predominance; the etiology is unknown. Immune dysregulation and atopic reaction to a continuous antigenic stimulus are being investigated as causes. One prominent theory claims that Candida albicans acts as a source of persistent antigen stimulus. This results in production of interleukin 5 (IL-5), which serves as an inflammatory mediator and chemotactic agent for eosinophils. A parasite has also been suggested as a potential cause, but none has been demonstrated.
Kimura disease usually occurs in the head and neck but can involve other parts of the body and present with painless subcutaneous masses. Lesions present as nontender subcutaneous swellings with a smooth or nodular surface. Color varies from deep red to skin colored. Ear involvement includes the auricle, postauricular sulcus, EAC, and meatus; the average lesion is 1.2 cm. Lesions can be associated with firm and palpable posterior cervical or supraclavicular lymph nodes. Kimura disease can be associated with nephrotic syndrome, and renal failure has been reported in patients with aggressive cases. Referral to a nephrologist may be indicated. [5]
Histologically, reactive prominent germinal centers are observed along with a cellular infiltrate of eosinophils, plasma cells, and histiocytes. Microabscesses can be present, and vascular proliferation with plump endothelium also is noted. Heavy immunoglobulin G (IgG) and immunoglobulin E (IgE) deposits can be seen on immunohistochemistry. Laboratory tests can be important for the evaluation of patients with Kimura disease. Renal function is assessed with creatinine and urinary protein levels. In addition, peripheral eosinophil counts and serum IgG and IgE levels can be elevated. Imaging may be helpful in Kimura disease. CT scan with contrast can highlight the lesion and any associated lymphadenopathy. MRI shows increased signal in T1 and T2 sequences.
Treatment of Kimura disease includes medical and surgical options. Complete surgical excision is generally recommended. The prognosis is generally good, but recurrence after surgery can be a problem. Renal involvement indicates a worse prognosis. Several medical regimens have been tried, including steroids and radiation therapy. Intralesional steroids have not proven very successful. Systemic steroids are reserved for patients in whom surgery fails or for those with renal involvement. Radiation therapy is used as a last resort. [7, 8]
A meta-analysis by Ye et al indicated that a combination of surgical resection and postoperative radiation therapy is more effective in discouraging local recurrence of Kimura disease than is either resection or radiation therapy by itself. [9]
Seborrheic keratosis
Seborrheic keratosis (SK) is common in the head and neck region, but ear involvement is rare. SK results from intracellular changes that create intraepidermal basal cell proliferation. It presents as an oval verrucous plaque. Early, the lesion appears light yellow, and it becomes more brown as its size increases. While usually asymptomatic, the lesions can cause itching, otorrhea, and otalgia. Histologically, thickened epidermis secondary to accumulation of immature keratinocytes between the basal layer and the surface, as well as invaginations of the thickened epithelium that create keratin tunnels, are seen. The tumor protrudes above the horizontal plane of the skin. While diagnosis may be based on the clinical presentation, SK should be differentiated from other lesions of the auricle and EAC. Recommended treatment involves removal of the lesion via various methods, including curettage, cryotherapy, laser ablation, topical vitamin use, or complete surgical excision, and a good prognosis is expected. Malignant transformation has been rarely reported. [10, 11] See the images below.
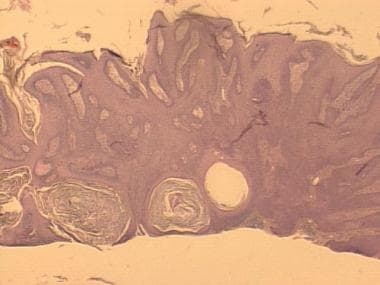 Seborrheic keratoses projecting above the level of the epidermis. Cysts represent sections of hyperkeratotic follicles.
Seborrheic keratoses projecting above the level of the epidermis. Cysts represent sections of hyperkeratotic follicles.
Exostoses
Exostoses are the most common bony abnormality of the EAC; they are present in approximately 1 of every 150 patients examined for otolaryngologic problems. Exostoses manifest as a gradual narrowing of the bony canal by multiple, bilateral, broad-based mounds of bone that arise from the anterior and posterior canal walls. Their multicentric and bilateral nature easily distinguishes them from osteomas (which are usually solitary and unilateral). Exostoses are most often observed in individuals with a history of cold-water exposure, such as swimmers or surfers. The bone deposition responsible for exostosis is thought to be secondary to a chronic periostitis due to exposure to cold temperatures. Exostoses are generally asymptomatic. Clinical manifestations, which can develop if the canal becomes occluded, include conductive hearing loss, postobstructive cerumen impaction and cholesteatoma, and otitis externa.
Histologic findings include a dense stratified arrangement of new bone that is remodeled over time into normal lamellar bone.
Medical management focuses on avoiding and preventing secondary otitis externa due a stenotic EAC. Ototopical drops are used for infection. Avoidance of water exposure (eg, watertight ear plugs) is recommended to reduce the risk of infection. Exostoses can be managed surgically if canal obstruction and symptoms arise. A canalplasty can be performed to remove the offending lesions. Tympanic membrane perforation can be avoided by raising medially based canal skin flaps and reflecting them onto the tympanic membrane. Bone curettes and diamond burrs are used to remove the bony growths. Split-thickness skin grafts may be needed for denuded canal skin. Patients undergoing surgical removal can expect a good prognosis unless cold-water exposure recurs.
An update to the 2008 American Academy of Otolaryngology-Head and Neck Surgery Foundation cerumen impaction clinical practice guidelines included the recommendation that any patient with cerumen impaction should be evaluated by a clinician for the presence of exostoses and other treatment-modifying factors. [12]
Premalignant Lesions of the External Ear
Actinic keratosis
Actinic keratosis (AK) is one of the most common premalignant lesions encountered on the ear. It most often is observed in individuals with fair complexions. The average age of onset is 62 years. Both sexes are affected equally. Sun exposure is thought to be the cause of AK. In Australia, where ultraviolet radiation levels are particularly high, the prevalence of actinic keratosis in men is approximately 79% and in women, 68%, between age 60 and 69 years. [13]
AK presents as round or irregularly shaped lesions that are scaly, keratotic, and flat topped. The color varies from gray to deep brown. Basophilic degeneration in the dermis with a chronic nonspecific inflammatory infiltrate and hyperkeratosis of the epidermis are seen on histology. Dysplastic cells can be present. AK may spontaneously regress, may persist, or may undergo malignant transformation; thus, removal of the lesion is recommended. Complete surgical excision is commonly chosen, whereas other methods may include cryotherapy and topical treatment with fluorouracil, imiquimod, and diclofenac. A good prognosis is expected with complete removal. [14]
Benign Tumors of the External Ear
Osteoma
An osteoma manifests as a discrete, pedunculated bony mass that arises in the EAC primarily from the tympanosquamous suture line adjacent to the bony-cartilaginous junction. The masses are solitary and unilateral (versus exostoses, which are multiple and bilateral). Osteomas are slow growing. These are the most common bony neoplasms of the temporal bone (exostoses are not true neoplasms). The incidence of osteoma formation peaks in the fourth decade of life. Osteomas are usually asymptomatic; however, symptoms can arise if canal obstruction occurs. Osteomas are more common in men than in women. No known definite link to cold-water exposure (unlike exostoses) or radiation has been demonstrated.
Histology reveals well-formed lamellae with multiple fibrovascular channels throughout the interlamellar spaces. Surgical removal of osteomas is similar to that of exostoses. Canal skin flaps are raised, and the lesion is drilled away, preferably with a diamond burr. Recurrence is unusual but necessitates more aggressive removal of bone.
Squamous papilloma
This is a more commonly appreciated lesion of the external ear. An AFIP series from 1976-1985 found 66 patients with squamous papilloma. Both sexes and all ages are equally affected. Squamous papilloma may be a result of exposure to the human papillomavirus (HPV), with virally induced genomic changes that cause cell proliferation. [15]
Squamous papilloma presents as a warty, verrucous, and elevated lesion that may be pigmented. It may have an overlying, thickened keratin layer. Histology indicates benign proliferation of uniform squamous cells, with a central core of vascular fibrous tissue. Surgical excision is recommended and is the most effective treatment. No recurrence or malignant degeneration was observed in the AFIP series of 66 patients. Topical treatments have been successfully used for squamous papillomas, but their effect in the EAC has not been examined.
Sebaceous adenoma
Sebaceous adenoma (SA) is rare in any part of the body and even rarer in the ear. Rulon and Helwig reported a series of 95 patients with SA, but only 3 of the lesions were located on the ear. SA has a male-to-female ratio of 2.5:1. [16, 17]
These tumors arise from sebaceous glands located in the skin of the ear and EAC; they present as a smooth, elevated, pedunculated, firm-to-soft lesion. The lesions usually are solitary and smaller than 0.5 cm. Color varies; tan, skin-colored, pink, and red lesions have been observed. SA lesions can bleed from trauma, but they rarely ulcerate.
On histology, the cells replace surface epithelium and represent a duplicate progression of sebaceous cell maturation. Pleomorphism of cells and nuclei can be seen with occasional mitotic figures. Complete surgical excision is recommended for SA, and a good prognosis is noted. Recurrence is rare.
Pilomatricoma
Pilomatricoma, previously termed pilomatrixoma, is a benign tumor of the hair follicle. It is relatively rare and has a higher incidence in females than in males. A study by Kwon et al of 137 pediatric patients found the male-to-female ratio to be 1:1.2. [18]
Pilomatricoma most commonly presents in the first 2 decades of life and is believed to arise from the hair follicles. Characteristics include necrosis, keratinization, and proliferation of small epithelial cells. Calcification or ossification is sometimes observed. The lesion presents as a slow-growing, bluish, solitary, and well-circumscribed nodule within the dermis of the auricle or preauricular region. Pilomatricoma can have a history of several years and can appear in other parts of the body. Growth can arrest spontaneously. [19]
Plain radiographs or CT scans can be useful because they may reveal areas of prominent stippled calcification. Histology shows irregular islands of progressively degenerating epithelial cells separated by fibrous stroma. There are 2 main cell types: basaloid cells at the margin of epithelial islands and anucleated shadow cells in the inner core. Calcium deposits are seen as fine basophilic granules. Complete surgical excision is recommended for pilomatricoma. A good prognosis is noted, but malignant transformation rarely occurs and is associated with multiple local recurrences.
Keratoacanthoma
Keratoacanthomas are relatively common and occur most often in white adults; the male-to-female ratio is 2:1. Keratoacanthoma has been linked to sun exposure, chemical carcinogens, trauma, and possibly a viral etiology. Keratoacanthoma arises from the hair follicles and involves 3 phases: proliferation, the developed tumor, and involution. [20] See the image below.
Neoplastic epithelium accumulates in the proliferative phase and results in keratin-filled invaginations or in a crater on the epidermal surface. The lesion presents as an elevated mass that appears flesh colored or slightly reddish; tightly stretched skin gives it a slightly translucent appearance. This phase is characterized by rapid growth within a few weeks. Over time, a central, umbilicated, keratinous plug develops; this plug can ulcerate. A puckered or pitted scar can be left after involution. Histology shows a discrete, highly keratinized crater with epidermis extending across borders. Characteristic marginal cupping is present. A keratoacanthoma larger than 2-3 cm is termed a giant keratoacanthoma and is rare.
Complete surgical excision is recommended. Keratoacanthoma can behave like squamous cell carcinoma and can also progress to carcinoma. However, unlike carcinoma, spontaneous involution can often occur. A good prognosis with low recurrence is noted with complete excision. Topical and intralesional cytotoxic drug therapy, cryotherapy, and radiation have also been used to treat keratoacanthomas.
Ceruminous gland tumors
Ceruminous gland tumors are rare neoplasms originating from the ceruminous glands of the cartilaginous EAC, specialized apocrine glands that secrete cerumen. Ceruminous gland tumors may be present for years and manifest as skin-covered, nonulcerated masses located in the lateral half of the EAC. Tumors can extend medially to involve the bony EAC or the middle ear. Symptoms result from EAC obstruction or discharge. Patient age range is 24-85 years, and there is no sex predilection. [21, 22, 23]
Histology reveals good demarcation from surrounding tissue but without a true capsule. A varied glandular pattern is observed, with an inner cuboidal eosinophilic epithelial component. Mitosis and pleomorphism are not characteristic. Complete surgical excision is recommended. Good prognosis with complete removal is noted; however, clear margins are imperative.
The term ceruminoma is less commonly used to refer to these lesions. The 2022 fifth edition of the World Health Organization Classification of Head and Neck Tumours uses the following classifications of benign and malignant ceruminous gland tumors [1] :
-
Benign - Adenoma NOS (not otherwise specificed), pleomorphic adenoma, and syringocystoma papilliferum
-
Malignant - Adenocarcinoma NOS, adenoid cystic carcinoma, and mucoepidermoid carcinoma
Cylindroma
Benign cylindroma is another rare benign tumor arising from the epidermal adnexa. Also called a turban tumor, it is not conclusive whether this neoplasm originates in the eccrine or apocrine glands, and in fact it may represent a primitive sweat gland tumor.
-
Classic chondrodermatitis nodularis chronica helicis on the superior helix.
-
Close-up view of same patient as in image above.
-
Chondrodermatitis nodularis chronica helicis on the antihelix.
-
Sharply circumscribed elevated seborrheic keratoses.
-
Closer view of multiple seborrheic keratoses in an autosomally dominant mode of inheritance.
-
Seborrheic keratoses projecting above the level of the epidermis. Cysts represent sections of hyperkeratotic follicles.
-
Seborrheic keratosis showing lackluster surface and appearance of being stuck on the skin surface.
-
Keratoacanthoma of the left forehead.













